Effect of intravenous clonidine on hemodynamic changes in laparoscopic cholecystectomy: a randomized control study
Abstract
Background: Laparoscopic surgery is associated with significant hemodynamic and pathophysiological changes due to creation of pneumoperitoneum. Clonidine is known to inhibit catecholamine and vasopressin release during pneumoperitoneum. This randomized, double-blinded, controlled study was conducted to evaluate the effect of administration of intravenous clonidine for the control of hemodynamic responses during the laparoscopic surgery and also to evaluate requirement of propofol during laparoscopic surgery.
Methodology: 60 patients undergoing elective laparoscopic cholecystectomy were randomized into Group-C (clonidine group) and Group-S (saline group). In clonidine group patients received 3µg/kg of clonidine diluted in 10 ml saline over 10 minutes, while in saline group patients received 10 ml saline. Induction of anesthesia was same in both groups. Heart rate, systolic, diastolic blood pressure and mean arterial pressure were measured before premedication, before induction, after intubation, before CO2insufflation, after insufflation and then subsequently at 15 min interval till desufflation and after extubation. Propofol requirement was calculated in both groups.
Statistical Analysis: Unpaired ‘T’ test was used to compare both groups. Decision of applying unpaired t-test was based on normality test (Shapiro-Wilk).
Results: Heart rate, systolic, diastolic and mean arterial blood pressures were significantly less in clonidine group as compared to control group. Intraoperatively there was significant heart rate variation in control group 82.93 ± 6.53/min to 96.13 ± 6.80/min than in clonidine group 86.30 ± 9.12/min to 73.13 ± 8.51/min (P < 0.001). Mean blood pressure varied from 94.51 ± 4.82 mmHg to 102.18 ± 5.56 mmHg in control group while in clonidine group it varied from 94.14 ± 7.82 mmHg to 72.62 ± 1.87 mmHg. (P < 0.001). Propofol requirement was significantly less in clonidine group.
Conclusion: Administration of clonidine attenuates hemodynamic response to pneumoperitoneum and reduces the requirement of propofol.
Key words: Clonidine; Propofol; Laparoscopic surgery; Pneumoperitoneum
Citation: Ubale P, Hemantkumar I. Effect of intravenous clonidine on hemodynamic changes in laparoscopic cholecystectomy: a randomized control study. Anaesth Pain & Intensive Care 2016;20(2):182-186
Received: 21 March 2016; Reviewed: 30 March, 24 April 2016; Corrected: 5 April, 4 June 2016; Accepted: 10 June 2016
INTRODUCTION
Laparoscopic cholecystectomy has become gold standard surgical option for cholelithiasis. It is a technique with cosmetic advantage, reduction of hospital stay, less postoperative pain and less morbidity; that make it the procedure of choice for gall stone disease. However, in terms of anesthetic care, an increased airway pressure, increased blood pressure values (systolic, diastolic and mean arterial pressures), decreased ventilatory capacities as well as associated hypercarbia have been the problems to be addressed. Pneumoperitoneum affects several homeostatic systems leading to alteration in acid base balance, cardiovascular and pulmonary physiology and stress response.1 The cardiovascular changes associated with pneumoperitoneum include an increase in mean arterial pressure, decrease in cardiac output and increase in systemic vascular resistance, which in turn compromise tissue perfusion.2 Clonidine, an imidazoline derivative is a selective alpha-2 adrenergic agonist and a potent antihypertensive drug which produces a fall in the heart rate, blood pressure, systemic vascular resistance (SVR) and cardiac output. Clonidine inhibits the release of catecholamines and vasopressin and thus modulates the hemodynamic changes induced by pneumoperitoneum in laparoscopic surgery.3,4 Intravenous clonidine has been used in the past as premedicant in neurosurgical patients, cataract surgeries and orthopedic procedures requiring application of tourniquet but very few studies are available which have used intravenous clonidine as premedicant for preventing adverse hemodynamic changes during laparoscopic cholecystectomy.5 Considering all these observations the present study is designed to evaluate the type and extent of hemodynamic changes, efficacy of clonidine in prevention of hemodynamic changes as well as to find out total propofol requirements during laparoscopic surgery.
METHODOLOGY
After approval from the institutional ethics committee and written informed consent from the patients this prospective, randomized double blind study was conducted from January 2013 to February 2014. Sixty patients, ages 18-65 years, ASA physical status I-II, BMI < 30 kg/m2, undergoing elective laparoscopic cholecystectomy under general anesthesia, were randomly divided into two groups, Group-C (clonidine group) and Group-S (saline group), using computer generated randomization list. Patients having gross renal, hepatic dysfunction, hypertension, patients on methyldopa, β receptors blockings drugs, benzodiazepines, MAO inhibitors and patients with anticipated difficult intubation were excluded from the study. Group allocation was done by an anesthesiologist who was not the part of study design. Drugs were administered by the anesthesiologist who was not the part of data collection and analysis. In clonidine group patients received 3 µg/kg of intravenous clonidine diluted to 10 ml normal saline over 10 minutes as premedication, while in saline group patient received 10 ml normal saline over 10 minutes. In case of hypotension mephentermine 6 mg and for bradycardia atropine 0.6 mg was to be used as a rescue treatment. In the operating room, intravenous cannula was secured and basic monitors were attached. Monitoring included heart rate (HR), systolic blood pressure (SBP), diastolic blood pressure (DBP), mean arterial pressure (MAP), pulse-oximetry (SpO2), and end tidal CO2 (EtCO2). Baseline (before premedication) values were noted. Patients were then premedicated with inj. glycopyrrolate 4 µg/kg, inj. ranitidine 1 mg/kg, inj. midazolam 0.03 mg/kg, and inj. fentanyl 2 µg/kg. Ringer lactate 10 ml/kg was infused during premedication. The baseline parameters before induction were then noted. General anesthesia was induced with thiopentone sodium 4-7 mg/kg. Orotracheal intubation was facilitated by 0.1 mg/kg vecuronium. Intubation was done with the appropriate sized endotracheal tube by trained anesthesiologists in all cases. Propofol infusion was started at 5 mg/kg/hr after inj. vecuronium and titrated to maintain mean arterial pressure between 60 to 80 mmHg. Time was noted when propofol infusion was started. Anesthesia was maintained with oxygen, nitrous oxide and propofol infusion. Neuromuscular relaxation was maintained by intermittent boluses of vecuronium 0.03 mg/kg according to TOF response. Pneumoperitoneum was created using CO2 by electronic insufflators. All patients were operated in 15○head-up tilt. Intraabdominal pressure was kept at 12 mmHg. Intermittent positive pressure ventilation (IPPV) was delivered with tidal volume and respiratory rate adjusted to maintain EtCO2 between 35 and 45 mmHg. Data recorded was heart rate, systolic blood pressure, diastolic blood pressure, mean arterial pressure, EtCO2, SpO2 after intubation, before insufflations, after insufflation and then every 15 min interval till desufflation and after extubation. Propofol infusion was stopped after desufflation and amount of propofol was noted. At the completion of surgery, residual neuromuscular block was antagonized with neostigmine and atropine, and each patient was extubated when he/she was fully wake, and transferred to recovery room. In the postanesthesia care unit (PACU) they were monitored for complications or adverse events like bradycardia and hypotension.
Statistical Analysis: After data collection, data entry was done in Microsoft Excel software. Data analysis was done with the help of PSPP software. Power of the study with the available mean and standard deviation for variables in our study was calculated and found to be more than 80%. Sample size of 30 patients in each group were enrolled in our study. Quantitative data was presented with the help of mean and standard deviation. Comparison among study groups was done with the help of unpaired T test. P value < 0.05 was taken as a level of significance.
RESULTS
Demographic data when analyzed did not show any significant difference in age, weight, among study groups and thus the two groups were comparable (P > 0.05).
Mean duration of pneumoperitoneum in clonidine group was 87.50 min vs. 83.33 min in control group, which was statistically not significant (P > 0.05). Mean duration of propofol use was 104.50 min in clonidine group vs, 99.67 in control group, which was statistically not significant (P > 0.05).
Comparison of HR showed significant difference at all intervals except at before premedication and before induction with a P value of 0.106 and 0.381 respectively. Mean HR varied from 86.30 ± 9.12 / min to 73.13 ± 8.51 / min in clonidine group while in control group it varied from 82.93 ± 6.53 / min to 96.13 ± 6.80 / min (P < 0.001). There was significant rise in HR after intubation and after insufflations and throughout the perioperative period. HR remained stable throughout the perioperative period in the clonidine group which was significant (P < 0.05). (Graph 1).
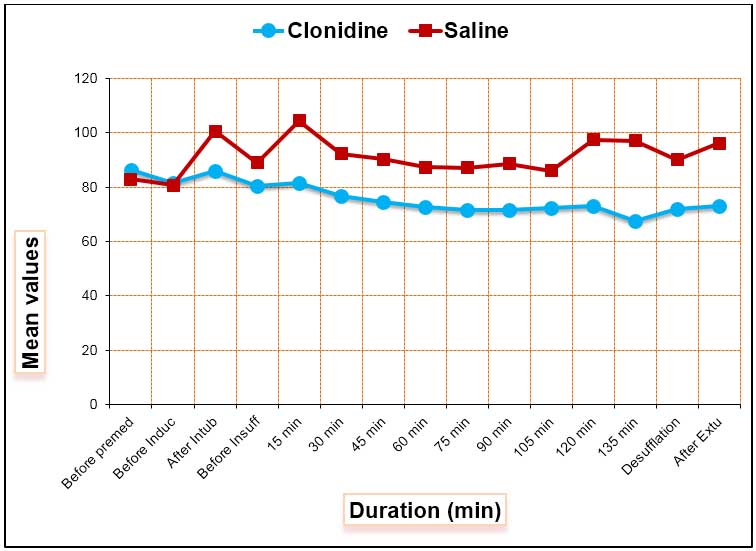
Graph 1: Graphical representation of heart rate between the groups
Comparison of SBP showed significant differences at all intervals except before premedication (P = 0.236). Mean SBP varied from 122.70 ± 11.04 to 99.73 ± 4.16 mmHg in clonidine group while in control group it varied from 125.53 ± 6.80 to 136.67 ± 7.71 (P < 0.001). There was significant rise in SBP after intubation and after insufflations and remained on the higher side in control group. While in clonidine group it remained significantly stable after intubation and after insufflations and throughout the perioperative period (P < 0.05) (Graph 2).
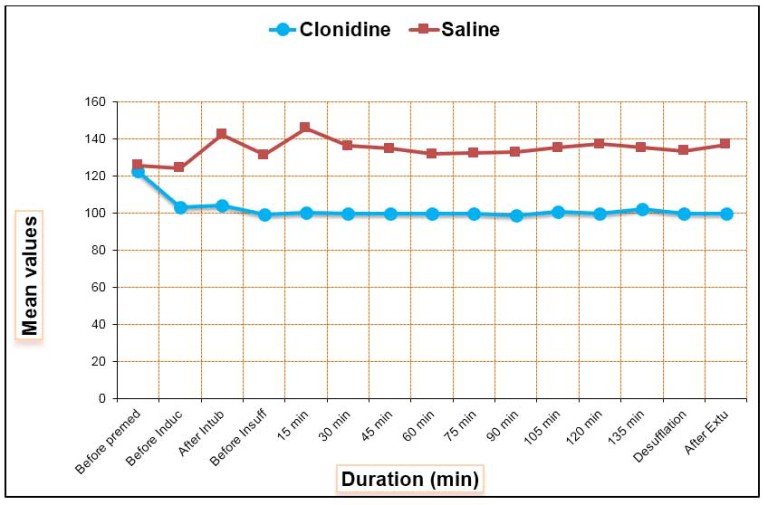
Graph 2: Graphical representation of SBP between the groups
Comparison of DBP shows significant difference at all intervals except before premedication (P = 0.601). Mean DBP varied from 79.87 ± 7.23 to 59.07 ± 3.35 in clonidine group while in control group it varied from 79.00 ± 5.40 to 84.93 ± 5.75 (P < 0.001). There was significant rise in DBP
after intubation and after insufflations and remained on the higher side in control group. While in clonidine group diastolic blood pressure remains stable throughout the intraoperative and postoperative period (P < 0.05) (Graph 3).
Graph 3: Graphical representation of Diastolic BP between the groups
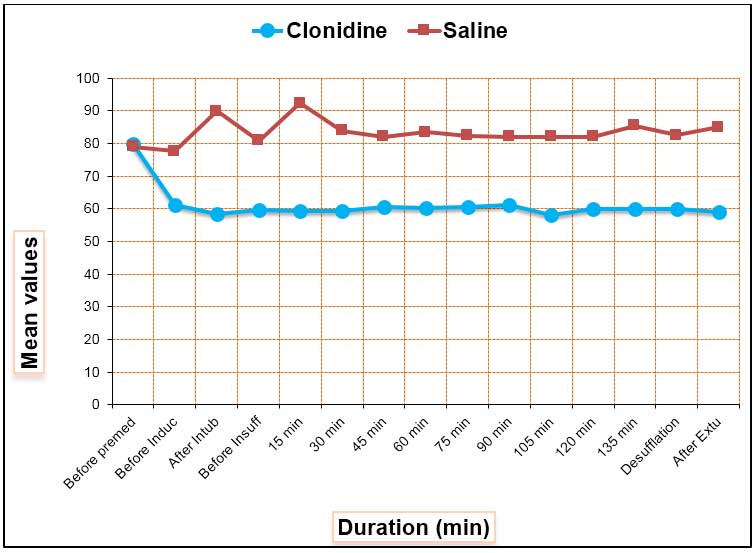
There was significant difference in MAP in the groups at all intervals except, before premedication (P = 0.828). MAP varied from 94.14 ± 7.82 to 72.62 ± 1.87 in clonidine group while in control group it varied from 94.51 ± 4.82 to 102.18 ± 5.56 (P < 0.001). MAP remains on the lower side in clonidine group after intubation and after insufflations and throughout the intraoperative and postoperative period in the clonidine group while in control group it remained on the higher side (P < 0.05) (Graph 4).
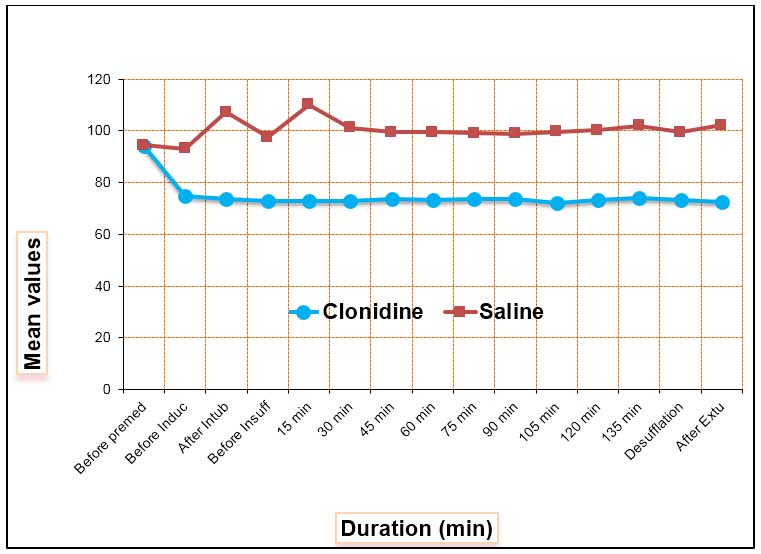
Graph 4: Graphical representation of Mean Arterial Pressure between the groups
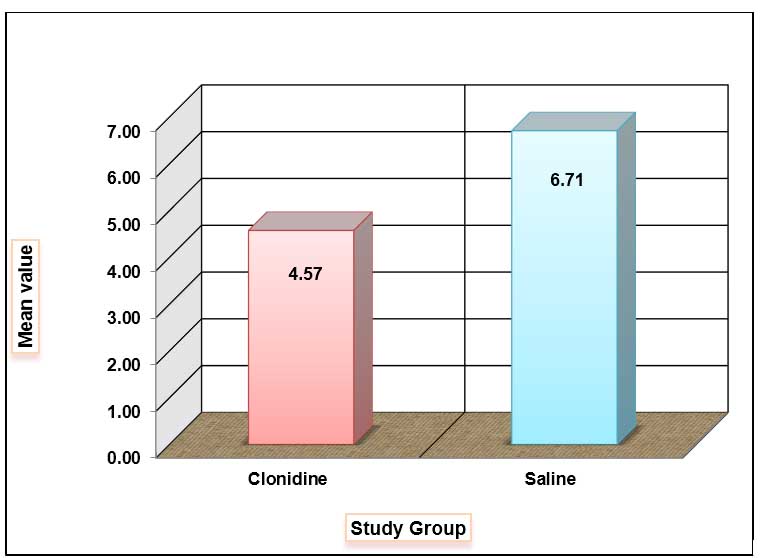
Graph 5: Propofol requirement between two groups
The SpO2 in both groups remained in the range of 98 to 100% and there was no statistical difference found in between the two groups (P > 0.05). Normocapnia was maintained throughout the surgery in both groups and there was no statistically difference in EtCO2 levels between the two groups (P > 0.05).
Total propofol requirement was significantly less in clonidine group than control group (4.57 vs, 6.71 mg/kg/hr) which was statistically significant (P < 0.05) (Figure 5).
DISCUSSION
Laparoscopic cholecystectomy has gained popularity in modern clinical practice as compared to open cholecystectomy. Operations that once required long hospitalization are now being performed on a short-stay basis. The advantages are; small incisions, reduced postoperative pain and discomfort, shorter hospital stay, early ambulation and early return to work. Anesthetic management of these patients is complicated by the major physiologic effects of pneumoperitoneum and patient positioning. The extent of cardiovascular changes associated with pneumoperitoneum includes an increase in arterial pressures, decrease in cardiac output, increase in SVR and PVR which in turn compromise tissue perfusion.
Reid and Brace first described the hemodynamic response to laryngoscopy and intubation due to intense sympathetic discharges caused by stimulation of larynx. Various pharmacological agents like adrenoreceptor blocker,6 betablockers,7 lidocaine,8 pregabalin,9and magnesium sulphate10 have been used to attenuate hemodynamic response during pneumoperitoneum. Inj. propofol, an ultrashort acting agent, also obtunds the hemodynamic response associated with laparoscopy. However, the dose requirements may be high to achieve this goal. Clonidine, an imidazoline derivative is a selective alpha-2 adrenergic agonist. It produces a fall in the heart rate and blood pressure associated with decrease in SVR and cardiac output. Clonidine is known to have longer recovery profile as it has a half life of 9-12 hours, and is thus suitable for anesthesia for major surgical procedures and not recommended for ambulatory anesthesia. Recent α2-adrenoceptor agonists with short duration of action (dexmedetomidine and mivazerol) are adapted for the administration of anesthesia for short stay procedures and in patients at high risk for coronary artery disease during surgery. The α2-adrenoceptor agonists have an analgesic action at several sites of the peripheral and central nervous system. It also prolongs effect of epidural or intrathecal local anesthetics and opioids.11 Clonidine, an α2 agonist inhibits the release of catecholamine and vasopressin and thus modulates the hemodynamic changes induced by pneumoperitoneum during laparoscopy.5
The present study has evaluated the effect of intravenous clonidine during laparoscopic cholecystectomy surgery under general anesthesia. The hemodynamic pressor response was effectively attenuated and the requirement of propofol was significantly reduced by clonidine.
In our study, clonidine 3 µg/kg IV has attenuated the stress response by pneumoperitoneum. Our results show that the hemodynamic parameters remain stable throughout intraoperative period, also the requirement of propofol is reduced, providing stable hemodynamic and protection against stress response.
Clonidine has been used in various doses (from 2 to 8 µg/kg) to attenuate hemodynamic responses to pneumoperitoneum in laparoscopic cholecystectomy. Malek et al12 used 150 μg of clonidine as IV infusion and intramuscularly while Sung et al13 and Yu et al14 used 150 μg of oral clonidine as premedication for maintenance of hemodynamic stability during pneumoperitoneum. They found that clonidine provided reasonably well hemodynamic stability at these doses without adverse effects. Ray et al15 and Altan et al16 used IV 3 μg/kg clonidine 15 min prior to induction, followed by continuous infusion and found significant incidence of bradycardia and hypotension. We used 3 μg/kg clonidine in premedication infused over 10 min. No intraoperative infusion was given, hence incidence of hypotension and bradycardia were insignificant in our study.
LIMITATIONS
Our study has few limitations. In our study design, we did not include observation of postoperative shivering, nausea, vomiting and pain relief. Our aim of the study was to find out effect of clonidine on hemodynamic effect in laparoscopic surgery in the dose we used. We did not compared drugs from a similar group drugs with similar effect to that clonidine like beta blockers.
CONCLUSION
Clonidine 3 μg/kg intravenously in premedication is effective in preventing the hemodynamic stress response during laparoscopic cholecystectomy. It is also cost effective in terms of reduction in the requirement of propofol.
Acknowledgment: We express our sincere thanks to our Head of Department and hospital ethics committee members for making this study possible.
Conflict of Interest: None
Author contribution: PU: Conduction of the study; IHK: Manuscript editing
REFERENCES
- Hong JY, Chung KH, Lee YJ. The changes of ventilatory parameters in laparoscopic cholecystectomy. Yonsei medical journal 1999; 40(4):307-312. [PubMed] [Free full text]
- Cunningham AJ, Turner J, Rosenbum S. Transoesophageal echocardiographic assessment of haemodynamic function during laparoscopic cholecystectomy. Br JAnaesth 1993;70:621. [PubMed]
- Joris J, Chiche JD, Lamy M. Clonidine reduced haemodynamic changes induced by pneumoperitoneum during laparoscopic cholecystectomy. Br J Anaesth. 1995; 74 (suppl): A124.
- Joris JL, Chiche JD, Canivet JL, Jacquet NJ, Legros JJ, Lamy ML. Haemodynamic changes induced by laparoscopy and their endocrine correlates: Effects of clonidine. J Am Coll Cardiol. 1998;32:1389–96.[PubMed] [Free full text]
- Laisalmi M, Koivusalo AM, Valta P, Tikkanen I, Lindgren L. Clonidine provides opioid-sparing effect, stable hemodynamics, and renal integrity during laparoscopic cholecystectomy. Surg Endosc. 2001;15:1331–5. [PubMed]
- Taittonen M, Kirvelä O, Aantaa R, Kanto J. Cardiovascular and metabolic responses to clonidine and midazolam premedication. Eur J Anaesthesiol. 1997;14:190–6. [PubMed]
- Koivusalo A M, Scheinin M, Tikkanen I, Yli- Suomu T, Ristkari S, Laakso J, et al. Effects of esmolol on hemodynamic response to Co2 pneumoperitoneum for laparoscopic surgery. Acta Anaesthesiol Scand.1998; 42: 510-7. [PubMed]
- De Oliveira GS Jr, Fitzgerald P, Streicher LF, Marcus RJ, McCarthy RJ. Systemic Lidocaine to improve postoperative quality of recovery after ambulatory laparoscopic surgery. Anesth Analg 2012; 115: 262-7. doi: 10.1213/ANE.0b013e318257a380. [PubMed]
- Gupta K, Sharma D, Gupta PK. Oral premedication with pregabalin or clonidine for hemodynamic stability during laryngoscopy and laparoscopic cholecystectomy: A comparative evaluation. Saudi J. Anaesth 2011; 5: 179-84. [PubMed] [Free full text]
- Jee D, Lee D, Yun S, Lee C. Magnesium sulphate attenuates arterial pressure increase during laparoscopic cholecystectomy. Br J Anaesth. 2009 Oct; 103(4):484-9. doi: 10.1093/bja/aep196. [PubMed] [Free full text]
- Maze M, Tranquilli W. Alpha-2 adrenoceptor agonists: defining the role in clinical anesthesia. Anesthesiology 1991; 74(3): 581-605. [PubMed] [Free full text]
- Yu HP, Hseu SS, Yien HW, Teng YH, Chan KH. Oral clonidine premedication preserves heart rate variability for patients undergoing laparoscopic cholecystectomy. Acta Anaesthesiol Scand 2003; 47(2): 185-190. [PubMed] [Free full text]
- Sung CS, Lin SH, Chan KH, Chang WK, Chow LH, Lee TY. Effect of oral clonidine premedication on perioperative hemodynamic response and postoperative analgesic requirement for patients undergoing laparoscopic cholecystectomy. Acta Anaesthesiol Sin 2000; 38(1): 23-29. [PubMed]
- Mutzbauer TS, Obwegeser JA, Gratz KW. Clonidine in oral medicine, literature review and our experience. Schweiz Monatsschr Zahnmed 2005; 115(3): 214-218. [PubMed]
- Ray M, Bhattacharjee DP, Hajra B, Pal R, Chatterjee N. Effect of clonidine and magnesium sulphate on anaesthetic consumption, haemodynamics and postoperative recovery: A comparative study. Indian J Anaesth. 2010;54:137–41. [PubMed][Free full text]
- Altan A, Turgut N, Yildiz F, Türkmen A, Ustün H. Effects of magnesium sulphate and clonidine on propofol consumption, haemodynamics and postoperative recovery. Br J Anaesth 2005; 94:438-41. [PubMed] [Free full text]