*Consultant & Head; **PG Trainee; ****SMO
Radiology Department, KRL General Hospital, Islamabad (Pakistan)
**PG Trainee, Radiology Department, Pakistan Institute of Medical Sciences (PIMS), Islamabad (Pakistan)
Correspondence: Dr. Muhammad Wasim Awan, FCPS, Consultant & Head, Radiology Department, KRL General Hospital, Islamabad (Pakistan); Phone: 00 92 333 514 2484; E-mail: drrwasim@yahoo.com
ABSTRACT
Obstetrical emergencies are important concerns and need immediate diagnosis and intervention to save the life of mother and fetus. These include obstetrical hemorrhage both ante partum and postpartum, ectopic pregnancy, preeclampsia and other conditions where radiologist, obstetricians, anesthesiologist and ICU team have important role to play. Radiologist play key role in diagnosing emergencies with the use of imaging modalities, though bed side ultrasonography has now become valuable tool in the hands of anesthesiologists as well, in diagnosing various emergencies. The role of interventional radiologist in cases of obstetric hemorrhage is worthwhile especially in postpartum hemorrhage where embolization can be minimally invasive lifesaving procedure.
The aim of this article is to discuss the valuable role that the radiologists play with obstetricians and anesthesiologists in the management of these obstetric and emergencies.
Key words: Ultrasonography; Obstetrical hemorrhage; Placenta previa; Placental abruption; Placenta accreta; Placenta increta; Ectopic pregnancy; Pre-eclampsia; Embolization
Citation: Awan MW, Ather S, Ahmed A, Rashid N. Role of radiology in the diagnosis and management of obstetrical emergencies. Anaesth Pain & Intensive Care 2014;18(4):436-42
INTRODUCTIONObstetrical emergencies (OE) are the leading cause of maternal death worldwide, though active management can bring significant reduction in the maternal mortality rate.
This article is mainly focused on the role of radiological investigations in the management of OE requiring close cooperation between the obstetricians, anesthesiologists and the radiologists. All the three departments have to work as a team in dealing these life threatening situations, and radiology plays a key role in the early diagnosis of obstetric emergencies.
The radiologists use multiple imaging modalities such e.g. ultrasonography (USG), computed tomography (CT), magnetic resonance imaging (MRI), x-rays, nuclear medicine, and positron emission tomography (PET) scan to diagnose or treat diseases. In interventional radiology they use minimally invasive techniques to treat the diseases and avoid major surgeries.
In our radiology department at KRL General Hospital Islamabad (Pakistan), we encounter a number of obstetrical emergencies. In most of the cases, we usually use USG as the cheap, non-invasive investigation as it has no radiation hazard to the mother or the fetus.
Bed side USG is also available in ICU setups of most of the hospitals, where immediate diagnosis is made; here ultrasound has become a valuable tool to be used by anesthesiologists and gynecologist as well. The anesthetist plays an important role as a member of the multidisciplinary team in managing high-risk pregnancies as they are trained in advanced life support and resuscitation, and manage the critically ill patients by providing anesthesia, sedation and pain management
INDICATIONS OF ULTRASONOGRAPHY IN OEBox 1: Major indications of USG
|
Obstetrical hemorrhage is mostly due to placental causes which require immediate diagnosis to avoid maternal and fetal morbidity and mortality. We have to look for placental causes of hemorrhage, retained products of conception (POC’s), placental tumors, metastases, and cystic lesions. Ultrasound remains the imaging modality of choice for evaluation of the placenta. Magnetic resonance imaging (MRI) gives added diagnostic value for further characterization of invasive placental processes such as placenta accreta and gestational trophoblastic disease. Computed tomography (CT) has a limited role in the evaluation of placental disease and also have a radiation risk to the fetus; this risk often outweighs the benefit. The CT is valuable primarily in the evaluation of trauma and gestational trophoblastic disease.1
PLACENTA PREVIA
Placenta previa is low lying placenta reaching or covering the internal cervical os. Painless 3rd trimester bleeding should be considered placenta previa until proven otherwise. It is diagnosed on both transabdominal and transvaginal sonography where placenta can be seen lying low in relation to the internal cervical os.
Figure 1: USG showing a low-lying placenta covering the internal cervical os
Figure 1 is a transabdominal ultrasound image showing placenta which is low lying and covers the internal cervical os.
Sometimes over-distended urinary bladder gives false positive diagnosis of low lying placenta so proper evaluation with adequately filled bladder is necessary. Over-distended bladder pushes the lower uterine segment into more horizontal position and may give false positive diagnosis of placental previa.2
False positive diagnosis of placenta previa is also seen in cases of uterine contractions giving the false impression of abnormally low lying placenta, so again the problem is solved by rescanning after passage of some time to allow uterine contractions to subside.3
Placenta which may appear low lying during early pregnancy has a fair chance to occupy its preferred site in the upper segment during the later half of pregnancy due to differential growth of lower uterine segment. However, the central placenta previa covering the internal os completely in the early pregnancy have less chances to migrate in the late pregnancy and even my not migrate at all.3
Sometimes during the third trimester of pregnancy cervix is not clearly visualized on transabdominal sonography so that it becomes difficult to rule out placenta previa. Transperineal sonography (TVS) provides confirmation of placenta previa when suspected on transabdominal sonography, especially during the 3rd trimester of pregnancy when the cervix is not clearly seen and allows the confident diagnosis. When it shows internal surface of cervix not covered by overlying placental tissue, placenta previa is definitely excluded.4
TYPES OF PLACENTA
Due to advanced maternal age and high frequency of women undergoing cesarean sections incidence of placenta accreta has increased. Placenta accreta is a condition where placenta is abnormally adherent to the uterine wall. On USG during first trimester we look for a low-lying sac that appears to be attached to the anterior wall of the uterus. Irregular vascular sinuses are seen having internal turbulent flow. The bladder wall is sometimes seen to be interrupted or have small bulges of the placenta into the bladder space. Echolucent space between placenta and myometrium is indistinct or lost due to placental invasion into myometrium but is not so reliable as it may be absent in the normal subjects. Color Doppler examinations show placental sinusoidal vessels traversing into myometrium. MRI is also used to diagnose or confirm the findings of placenta accreta seen on ultrasound.5 Similarly, placenta concreta and percreta can also be diagnosed with USG.
PLACENTAL ABRUPTION
Placental abruption during the 3rd trimester being less common complicates less than 1% of pregnancies but causes significant risk to mother and fetus when it does occur. It can be seen after trauma or maternal hypertension or drugs. Usually it is diagnosed clinically by typical findings of abdominal pain, tenderness, uterine hypertonicity and bleeding. USG shows extent of sub chorionic or retroplacental hematoma. Ultrasound is not so much sensitive for abruption because if the hematoma is lying close to the cervix at the placental margin it may be drained through vagina and no hematoma is detected on ultrasound. Such patients are still given the diagnosis of abruption at delivery based on clinical signs and symptoms and placental examination. However, if ultrasound does show subchorionic or retroplacental hematoma the positive predictive value for the abruption at delivery is high.6
RETAINED POC’SWhen on ultrasound endometrial thickness is < 15 mm with no evidence of retained POC’s complete miscarriage is diagnosed. In cases of distorted midline endometrial echo with heterogeneous tissue / sac lying within it, then it is suggestive of incomplete abortion and when sac diameter is more than 20 mm with no embryo or yolk sac detected it is diagnostic of blighted ovum or an embryonic pregnancy.ECTOPIC PREGNANCY
Ectopic pregnancy is an obstetrical emergency, with its rate steadily increasing owing to in vitro fertilization, embryo transfer, microsurgical techniques, and better early diagnosis.7
On ultrasound in cases of suspected ectopic pregnancy, we see endometrial thickening and sometimes pseudo-sac formation secondary to hormonal stimulation from the ectopic sac elsewhere. Fluid or a hematoma may be seen in the cul-de-sac from ruptured ectopic pregnancy. A simple or complex cyst in the adnexa may be seen carrying the possibility of ectopic gestation. However, on rare occasion a sac showing live embryo may be detected providing definitive diagnosis of ectopic pregnancy.
Ectopic locations may include ovaries, fallopian tubes, abdominal, cervical and others.
Figure 2: Gestational sac with live embryo within it at cervix, suggestive of ectopic cervical pregnancy
Figure 2 is an image of transabdominal sonography showing gestational sac with live embryo within it in the region of cervix, suggestive of ectopic cervical pregnancy.
Transvaginal sonography provides high resolution for detection of ectopic gestational sac as early as 1 week from a missed menstrual period. Ultrasound correlation with serum β-hCG levels is done using a discriminatory zone. The β-hCG discriminatory zone is the level above which it shows positive result for pregnancy. Ectopic pregnancy is strongly suggested when β-hCG concentration are above the discriminatory zone, and intrauterine sac is not seen. In high risk patients ultrasound alone has high sensitivity and specificity in diagnosis of ectopic pregnancy, so it is preferred modality in detecting complications of early pregnancy due to its higher resolution.8
In the ectopic pregnancy, transvaginal sonography shows complex adnexal cyst or mass or sometimes sac with live embryo itself, a hematoma caused by its rupture, or both. Although tubal location is most common, unusual locations of ectopic pregnancy are isthmic, cervical, ovarian, and abdominal. Ultrasound is the mainstay of diagnosis, but magnetic resonance imaging is helpful in unusual or complicated cases. Radiology also provides minimally invasive treatment for ectopic gestation via sonographically guided systemic methotrexate injections.9
POSTPARTUM HEMORRHAGE
Patients with retained products of conception (RPOC) present with postpartum hemorrhage after spontaneous or induced abortion and parturition. Patients usually have complaints of abdominal pain, bleeding and fever. On examination cervical external os is open. The diagnosis is based on ultrasound appearances showing hyper or hypoechoic material seen within any part of uterine cavity or thickened endometrium along with irregular interval between the endometrium and myometrium.9
Figure 3: Incomplete abortion with residual retained products of conception.The lower uterine segment in women with incomplete abortion my show residual retained products of conception on TAS imaging. Imaging usually shows thickened endometrium filled with echogenic material in lower uterine segment and indicates urgent dilatation and curettage (Figure 3).
Transvaginal sonography is also done for detection of RPOC and shows retained placental tissue or fetal portion well and clear than seen on transabdominal sonography. An endometrial thickness of 13 mm or more, seen on transvaginal sonography, has the best diagnostic efficiency with the sensitivity and specificity for detecting retained products of conception approaching 85% and 64% respectively.10
Transabdominal sonography shows uterine disruption, nonvisualization of uterine wall, placental tear or hematoma formation in cases of uterine rupture.
IUGRIntra uterine growth retardation (IUGR) is a syndrome in which the fetus fails to achieve normal growth; it is characterized as a baby who is small for the corresponding gestational age.
It is associated with various complications including increased risk of meconium aspiration, respiratory distress syndrome, and asphyxia during delivery, still birth and developmental delay. Doppler ultrasound is very valuable in diagnosing fetal distress secondary to IUGR, baby / maternal comorbid conditions or oligohydramnios as it shows uteroplacental insufficiency with increased resistance in the umbilical cord arterial flow and increased blood flow to the fetal brain by showing high resistance flow in umbilical and uterine arteries and increase in the systolic/diastolic (S/D) ratios while fall in the resistance of middle cerebral artery with consequent fall in its S/D ratio for the corresponding gestational ages. As the gestational age advances the diastolic flow normally increases in the umbilical artery resulting in the low resistive waveform on the Doppler ultrasound of umbilical artery with lowering levels of S/D ratios while in cases of distress this waveform becomes high resistive with reduced diastolic component and it may show even absent diastolic flow or inversion during diastolic phase in cases of severe distress and hypoxia.11
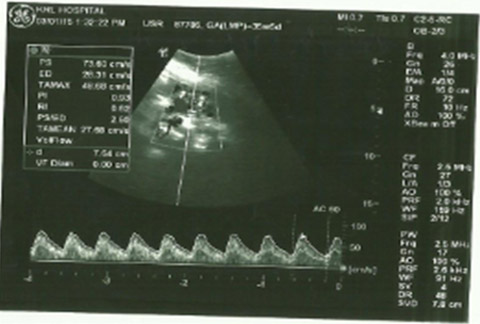
Figure 4: Ultrasound power Doppler image showing normal umbilical arterial Doppler waveform showing low resistance flow with normal S/D ratioDoppler ultrasound of fetal umbilical artery, middle cerebral artery and uterine arteries are valuable in assessing fetal distress, anaemia and hypoxia.
MCA Doppler is also valuable in the intrauterine growth restriction and twin twin transfusion syndrome.
Normally fetal MCA S: D ratio should always be higher than the umbilical arterial S:D ratio. In cases of fetal distress umbilical artery resistance increases and MCA resistance falls due to brain sparing effect of MCA and the ratio reverses.
In fetuses with suspected IUGR, abnormal MCA/UA S/D ratios are strongly predicting the low birth weight and prematurity at delivery. Abnormal MCA/UA S/D ratios are also indicative of need for immediate emergency delivery (Figure 5).11
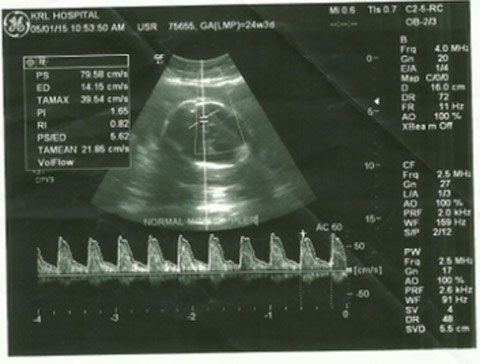
Figure 5: Doppler ultrasound from fetal middle cerebral artery showing normal high resistive waveform with decreased diastolic flow
Figure 6: Image of fetal middle cerebral artery doppler shows brain sparing effect of middle cerebral artery in case of fetal hypoxia showing abnormal low resistive waveform with high diastolic flow
Obstetric hemorrhage is the major issue with two third of cases of severe maternal morbidity being associated with obstetric hemorrhage.12
ROLE OF INTERVENTIONAL RADIOLOGY
Interventional radiology have impressive role in management of various obstetrical emergencies. Pelvic arterial embolization has added a new dimension in the management of obstetric hemorrhage. This technique has nowadays gained acceptance as a first line treatment option for controlling postpartum hemorrhage when the conservative measures fail. It is more commonly done to control bleeding in cases of uterine atony, though pelvic arterial embolization is also indicated in bleeding due to lacerations of female genital tract, abnormal placentation, arteriovenous malformations and postsurgical complications and uterine tears at the time of C-sectons.12
In common daily practice, in obstetric hemorrhage refractory to conservative treatment, obstetricians usually go for major surgery, leading to associated risk of general anaesthesia, laparotomy and loss of fertility when hysterectomy is done. Interventional radiology provides safe, minimally invasive and fertility preserving alternative to conventional surgery for the treatment of obstetrical hemorrhage, placental abnormalities, abortion and ectopic pregnancy.12
It is observed that obstetric emergencies may become fatal and need immediate involvement of gyne/obs specialists with pre and postoperative ICU care. In cases of emergencies in ICU especially in case of postpartum hemorrhage it is the duty of anesthetist and obstetricians to call a radiologist for immediate management and embolization of vessels to control the hemorrhage.
So it is a team work of radiology department with obs/gyne and anesthesia departments and ICU staff to deal with obstetric emergencies. This serves to reduce the complications associated with obstetric practice and significantly reduces the perinatal morbidity and mortality.
REFERENCES- Elsayes KM, Trout AT, Friedkin AM, Liu PS, Bude RO, Platt JF. Imaging of the placenta: a multimodality pictorial review. Radiographics. 2009 Sep-Oct;29(5):1371-91. [PubMed] [Free full text] doi:10.1148/rg.295085242.
- Zemlyn S. The effect of urinary bladder in obstetrical ultrasound. Radiology 1987;128(1):169-175. [PubMed] [Free full text]
- Townsend RR, Laing FC, Nyberg DA, Jeffrey RB, Wing VW. Technical factors responsible for ‘Placental migration’: Sonographic assessment. Radiology. 1986 Jul;160(1):105-8. [PubMed] [Free full text]
- Hertzberg BS, Bowie JD, Carroll BA, Kliewer MA, Weber TM. Diagnosis of placenta previa during the third trimester: role of Transperineal sonography. AJR Am J Roentgenol. 1992 Jul;159(1):83-7. [PubMed] [Free full text]
- Comstock CH. Antenatal diagnosis of placenta accreta: a review. Ultrasound Obstet Gynecol. 2005 Jul;26(1):89-96. [PubMed] [Free full text]
- Glantz C, Purnell L. Clinical utility of sonography in the diagnosis and treatment of placental abruption. J Ultrasound Med. 2002 Aug;21(8):837-40. [PubMed] [Free full text]
- Dialani V, Levine D. Ectopic Pregnancy: A Review. Ultrasound Q. 2004 Sept;20(3):105-117. [PubMed]
- Barnhart KT, Simhan H, Kamelle SA. Diagnostic accuracy of ultrasound above and below the beta-hCG discriminatory zone. Obstet Gynecol. 1999 Oct;94(4):583-7. [PubMed]
- Sadan O, Golan A, Girtler O, Lurie S, Debby A, Sagiv R, et al. Role of sonography in the diagnosis of retained products of conception. J Ultrasound Med. 2004 Mar;23(3):371-4. [PubMed] [Free full text]
- Ustunyurt E, Kaymak O, Iskender C, Ustunyurt OB, Celik C, Danisman N. Role of transvaginal sonography in the diagnosis of retained products of conception. Arch Gynecol Obstet. 2008 Feb;277(2):151-4. [PubMed]
- Sterne G, Shields LE, Dubinsky TJ. Abnormal fetal cerebral and umbilical doppler measurements in fetuses with intrauterine growth restriction predicts the severity of perinatal morbidity. J Clin Ultrasound 2001;29(3):146–151. [PubMed]
- Gonsalves M, Belli A. The role of interventional radiology in obstetric hemorrhage. Cardiovasc Intervent Radiol 2010;33:887-895. [PubMed]