Shipra Aggarwal, Neha Baduni, Aruna Jain
Department of Anesthesiology & Critical Care, LHMC & Associated Hospitals, New Delhi, (India) 110001
Correspondence: Dr. Neha Baduni, Department of Anesthesiology & Critical Care, LHMC & Associated Hospitals, New Delhi, (India) 110001; Tel: +91-9891224764; E-mail: baduni.neha@gmail.com
ABSTRACT
Background: Laryngoscopy and tracheal intubation increase blood pressure (BP) and heart rate (HR). The aim of the present study was to investigate the effect of gabapentin given before operation on the hemodynamic response to laryngoscopy and intubation in patients undergoing laparoscopic cholecystectomy.
Methodology: 90 ASA I and II patients undergoing elective laparoscopic cholecystectomy were randomly allocated to three groups of 30 each. Group C received placebo drug; group G6 received gabapentin 300 mg night before surgery and 300 mg at 6:00 AM on the day of surgery; group G9 received gabapentin 300 mg night before surgery and 600 mg at 6:00 AM on the day of surgery. Anesthesia was induced with inj. thiopentone and inj. rocuronium. Heart rate, systolic BP, diastolic BP and mean arterial pressure were recorded as baseline, after induction, at tracheal intubation (0 min.); and then at 1, 3, 5, 10, 15 min following tracheal intubation.
Results: MAP was significantly lower in G9 group as compared to the control group at 0, 1, 3, 5, 10 and 15 minutes. Heart rate did not differ amongst the three groups at any time interval.
Conclusions: Gabapentin, under present study design, attenuates the pressor response but not tachycardia associated with laryngoscopy and intubation.
Key words: Intubation; Laryngoscopy; Gabapentin
Citation: Aggarwal S, Baduni N, Jain A. Attenuation of pressor response to laryngoscopy and intubation – a comparative study between two doses of gabapentin in patients undergoing laparoscopic cholecystectomy. Anaesth Pain & Intensive Care 2015;19(1):33-36
INTRODUCTION
The pressor response of tachycardia and hypertension to laryngoscopy and intubation may increase perioperative mortality and morbidity, particularly for patients with cardiovascular and cerebral diseases. Several drugs have been tried in the past to attenuate the pressor response.1,2
The present study was designed as a double blind randomized control trial to investigate the effect of Gabapentin on changes in heart rate and blood pressure observed during laryngoscopy and tracheal intubation in patients undergoing laparoscopic cholecystectomy.
METHODOLOGY
After obtaining the approval of institutional ethical committee and written informed consent from the patients, 90 patients of ASA (Grade I & II) in the age group of 18-45 years were included in the study. Exclusion criteria were urgent surgical procedures, difficult intubation, any systemic illness, obesity, patients on any drug treatment or with history of allergy to any drug and pregnancy.
This study was a randomized control trial. The patients were randomly divided into three equal groups (30 each) according to computerized generated random number tables. Both the observer as well as the subject were unaware of the drug being administered. All patients were premedicated with tab diazepam (5 mg) the night before surgery and inj. pethidine (1mg/kg body weight) and inj. Phenergan (promethazine) (0.5 mg/kg body weight) intramuscularly one hour before surgery. In addition, they were also given gabapentin/placebo as per group allotted by an observer unaware of the study.
Group C: Cap placebo HS + Cap placebo at 6:00 AM on the day of surgery
Group G6: Cap gabapentin (300 mg) HS + cap gabapentin (300 mg) at 6:00 AM on the day of surgery
Group G9: Cap gabapentin (300 mg) HS + cap gabapentin (600 mg) at 6:00 AM on the day of surgery
In the operating room, routine monitoring included electrocardiogram, non-invasive blood pressure (NIBP), pulse oximetry and capnography. After recording baseline parameters anesthesia was induced with sleep dose of thiopentone sodium till the eyelash reflex was gone. Inj. rocuronium bromide (1 mg/kg body weight IV) was used to facilitate tracheal intubation. Patients were ventilated with 50:50 nitrous oxide and oxygen using Bain’s circuit. Laryngoscopy and intubation were performed 90 second after rocuronium administration. We used Macintosh laryngoscope blade No. 3. Endotracheal tubes of size 7.5 mm and 8 mm were passed in all female and all male patients respectively. After tracheal intubation, the lungs were ventilated with 60% nitrous oxide in oxygen and end tidal carbon dioxide was maintained between 30-35 mmHg. No surgical intervention was allowed till observations were completed.
Parameters were recorded before induction (baseline), after induction, immediately at tracheal intubation (0 min), and at 1, 3, 5, 10 and 15 min after intubation. Patients were also observed for hypoxemia and ECG changes.
Statistical analysis
Demographic data were compared in the three groups using ANOVA test. The duration of laryngoscopy and intubation was compared using Kruskal Wallis test. Systolic (SBP) and Diastolic blood pressure (DBP), mean arterial pressure (MAP) and heart rate (HR) were analyzed using t-test.
RESULTS
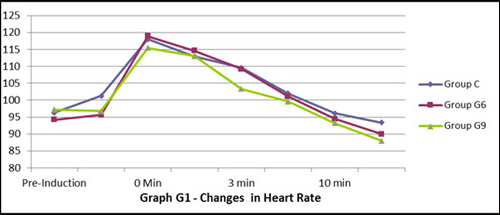
All patients were comparable with respect to age, sex and weight (Table 1). The duration of laryngoscopy and intubation was also comparable. The heart rate increased immediately after laryngoscopy and intubation in all the three groups (Figure 1). It remained high for longer period (5 min) in Group C as compared to Group G6 and G9 (3 min and 1 min respectively) though it was insignificant statistically. This shows Gabapentin (600 and 900 mg) was not able to attenuate tachycardia following laryngoscopy and intubation. But duration of stress response was shortest with 900 mg Gabapentin and longest in control group.
Table 1: Patient Characteristic and duration of Laryngoscopy and Intubation
| Parameters |
Group C |
Group G6 |
Group G9 |
p-value |
| Age (Yrs) |
37.07 |
36.43 |
36.23 |
0.94 |
| Weight (KG) |
53.83 |
54.33 |
56.7 |
0.58 |
| Sex F:M |
26:4 |
24:6 |
25:5 |
0.78 |
| Duration of Laryngoscopy and Intubation (Sec) |
20.5 ± 6.06 |
19.63 ± 4.87 |
S |
0.772 |
Figure 1: Changes in heart rate in three groups
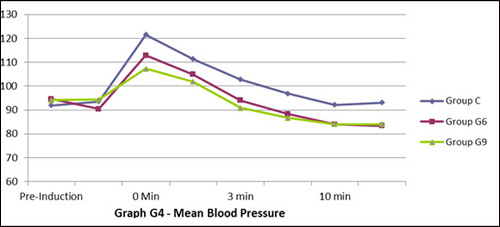
Baseline SBP, DBP and MAP were comparable in all three groups. The trend of change in SBP, DBP and MAP followed almost the same pattern in all three groups with regard to time (Figures 2, 3, 4).
Figure 2: Systolic blood pressure
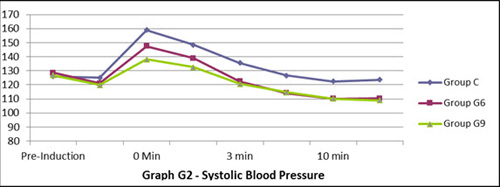
A highly significant rise in MAP was observed at laryngoscopy and intubation in all the three groups. It remained significantly high till 3 minutes in control group where as only for 1 minute in Groups G6 and G9. MAP didn’t touch baseline value even after 15 min in control group. On the contrary, a statistically highly significant (p < .05) but clinically acceptable fall in MAP was observed at 5, 10 and 15 min in Groups G6 and G9. Inter group comparison showed that MAP was significantly high (p < .05) in control group as compared to Group G9 and insignificantly high (p > .05) as compared to Group G6 at the time of intubation. This shows that attenuation of pressor response was better and shortest with Group G9 as compared to control and 600 mg gabapentin. There was no incidence of hypoxemia, arrhythmia or ST segment changes in ECG throughout the study period.
Figure 3: Diastolic blood pressure
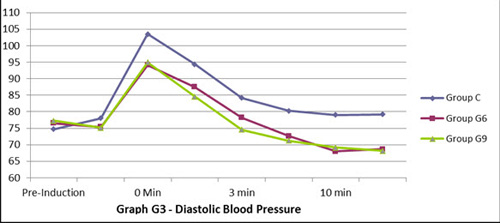
Figure 4: Mean blood pressure
DISCUSSION
Gabapentin, a structural analogue of gamma amino butyric acid, is used primarily for the treatment of seizures, neuropathic pain, and hot flushes. Recently, it has been found to be effective in reducing the noxious stimuli to laryngoscopy and intubation, thereby attenuating the hemodynamic response.3
Gabapentin acts by decreasing the synthesis of neurotransmitter glutamate and by binding to voltage dependant calcium channel. Action similar to calcium channel blockers may be responsible for blunting the hemodynamic response to laryngoscopy and intubation. Memis et al reported that inhibition of calcium efflux from muscle cell with a consequent smooth muscle relaxation might explain the effectiveness of gabapentin in attenuating stress response.
Laryngoscopy and tracheal intubation may induce a profound alteration in the hemodynamics of a patient. In response to these procedures, the plasma concentrations of catecholamines is increased and this may even provoke myocardial ischemia and cerebral hemorrhage.4
In the present study we evaluated the effect of two different doses of oral gabapentin on hemodynamic variables during laryngoscopy and intubation. Analysis revealed that 900mg of gabapentin effectively prevented the rise in blood pressure following intubation.
Fassoulaki et al used a much higher dose of Gabapentin i.e.1600 mg (400 mg at 6 hour interval started a day before surgery) and showed that it attenuated the rise in blood pressure but not tachycardia associated with laryngoscopy and intubation. Similarly, other workers have showed that pre-treatment with 800 mg of Gabapentin 2 hour before surgery effectively suppresses the increase in intra-ocular pressure secondary to endotracheal intubation and attenuated the increase in MAP but not heart rate response associated with laryngoscopy and intubation.5,6 The results of present study are similar to these workers.
Slightly different observations have been made by some workers recently. Ayatollahi et al showed that 800 mg of gabapentin 90 minutes before a procedure attenuated the rise of diastolic pressure and mean arterial pressure with no effect on systolic blood pressure and heart rate.7.Ifthekahar et al assessed the effect of 800 mg oral gabapentin given one hour before surgery. They found that it decreased only mean arterial pressure after laryngoscopy.8 But both these workers concluded that gabapentin was ineffective in preventing tachycardia following laryngoscopy.
The effect of gabapentin and dexamethasone given together or separately one hour before surgery on laryngoscopy and intubation has been compared and it has been found that all three treatments attenuated the heart rate and pressor response, but was significantly greater with combination than with either drug alone.9 Ali and Gohary et al in 2009 observed that 1200 mg Gabapentin given two hour before surgeryattenuated the increase in MAP and heart rate response to tracheal intubation in adults but thedrug did not attenuate the catecholamine response to intubation and even augmented the increaseof norepinephrine levels.10
The difference between the result of these workers and present study may be because of difference in anesthesia technique used by them. Arterial baroreflex function is known to be significantly depressed during propofol and sevofulurane with Nitrous oxide anesthesia.11
We didn’t measure stress mediators such as plasma catecholamine levels. This can be considered
as limitation of our study. Barak and colleagues did not find any correlation between hemodynamic changes to laryngoscopy and intubation and catecholamine levels.12
Other authors have investigated the effect and safety of 600mg of gabapentin given two hours before induction, esmolol, or their combination on hemodynamic response to laryngoscopy and intubation. They revealed that a combination of esmolol and gabapentin effectively suppressed any rise in blood pressure as well as heart rate following laryngoscopy.13
Montazeri et al compared the efficacy of oral gabapentin and clonidine premedication for controlling the hemodynamic responses to laryngoscopy and intubation and found both to be equally effective in preventing any rise in blood pressure.14
CONCLUSION
To conclude, gabapentin effectively prevents rise in blood pressure after laryngoscopy. But these data are not yet sufficient to establish the optimum dose of gabapentin. Further investigations are needed to focus on timing and dose response relationship, so that we can utilize gabapentin efficiently as an adjuvant to anesthesia. Moreover, more work is needed on the effect of gabapentin in combination with other drugs on the rise in blood pressure and heart rate during laryngoscopy.
REFERENCES
- Abou Madi M, Hugo K, Yacoub O. A method for prevention of cardiovascular reactions to laryngoscopy and intubation. Can Anaesth Soc J. 1975 May;22(3):316-29. [PubMed]
- Stoelting RK. Blood pressure and heart rate changes during short duration laryngoscopy and tracheal intubation, influence of viscous or IV lignocaine. Anesth Analg. 1978;57(2):197-9. [PubMed]
- Ashgan Raouf A, El Gohary M, Salah El-din Ashwani H, El- Kerdawy HM, Essa HH. Efficacy of preoperative oral gabapentin in attenuation of neuro-endocrine response to laryngoscopy and endotracheal intubation. J Med Sci. 2009;9:24-9. DOI: 10.3923/jms.2009.24.29
- Marashi SM, Ghafari MH, Saliminia A. Attenuation of haemodynamic responses following laryngoscopy and tracheal intubation-comparative assessment of clonidine and gabapentin premedication. Middle East J Anesthesiol. 2009;20(2):233-37. [PubMed]
- Kaya FN, Yavascaoglu B, Baykara M. Altun GT, Gülhan N, Ata F. Effect of oral gabapentin on intraocular pressure and haemodynamic responses induced by tracheal intubation. Acta Anaesthesiol Scand. 2008 Sep;52(8):1076-80. doi: 10.1111/j.1399-6576.2008.01627.x. [PubMed]
- Memis D, Turan A, Karamanlioglu B, Seker S, Türe M. Gabapentin reduces cardiovascular responses to laryngoscopy and tracheal intubation. Eur J Anaesthesiol. 2006;23(8):686-690. [PubMed]
- Ayatollahi V, Mirshamsi P, Behad S, Amirdosara M, Vaziribozorg S. Effect of oral gabapentin on haemodynamic variables during microlaryngeal surgery. Anesthesiol Intensive Ther. 2014;46(1):17-22. [PubMed] [Free full text] doi: 10.5603/AIT.2014.0004.
- Ifthikar T, Taqi A, Sibtain A, Anjum S, Awan I. Oral gabapentin reduces haemodynamic responses to direct laryngoscopy and tracheal intubation. Anaesth Pain & Intensive Care. 2011;15(1):17-20. [Free full text]
- Fassoulaki A, Melemeni A, Paraskeva A, Petropoulos G. Gabapentin attenuates the pressor response to direct laryngoscopy and tracheal intubation. Br J Anaesth. 2006 Jun;96(6):769-73. [PubMed][Free full text]
- Singhal SK, Kaur K, Arora P. Oral clonidine versus gabapentin as premedicant for obtunding hemodynamic response to laryngoscopy and tracheal intubation. Saudi J Anaesth. 2014 Apr;8(2):172-7. [PubMed] [Free full text] doi: 10.4103/1658-354X.130692.
- Tanaka M, Nishikawa T. Arterial baroreflex function in humans anaesthetized with sevoflurane. Br J Anaesth 1999;82(3):350-4. [PubMed]
- Barak M, Ziser A, Greenberg A, Lischinsky S, Rosenberg B. Haemodynamic and catecholamine response to tracheal intubation and direct laryngoscopy compared with fibreoptic intubation. J Clin Anesth 2003;15(2):132-6. [PubMed]
- Shrestha G, Marhatta M, Amatya R. Use of gabapentin, esmolol or their combination to attenuate haemodynamic response to laryngoscopy and intubation. Kathmandu Univ Med J (KUMJ). 2011 Oct-Dec;9(36):238-43. [PubMed]
- Montazeri K, Kashefi P, Honarmand A, Safavi M, Hirmanpour A. Attenuation of pressor response to direct layngoscopy and tracheal intubation: oral clonidine vs oral gabapentin premedication. J Res Med Sci. 2011; 16 Suppl 1:S377-86. [PubMed] [Free full text]