Omar Al Misnid*
Author’s affiliation:
*Omar Al Misnid, Assistant Professor of Anesthesiology, Department of Emergency, Critical Care & Anesthesia, College of Medicine, Qassim University, Qassim, Saudi Arabia; Email: o.almisnid@qu.edu.sa; {ORCID:0000-0002-4147-9463}
Correspondence: Omar Al Misnid; Email: o.almisnid@qu.edu.sa
Regional blocks for the anterolateral chest wall are challenging in regard to the anatomical basics and innervation, the limitation of available evidence, lack of credible guidelines, and wide discrepancy in the existing practice among the health practitioners across the countries. Despite the challenges, recently new fascial plane blocks have been used more often as analgesic techniques. In very few occasions these techniques have been reported in literature as surgical blocks in certain cases where general anesthesia was not favorable or advisable. We present a challenging case in which the scheduled surgery had to be postponed due to high risk if done under general anesthesia, as she was concurrently suffering from multiple comorbidities and needed much status optimization. At the same time, her procedure was time sensitive to diagnose her medical illness and initiate the proper management.
Keywords: Regional Anesthesia; Pain Management; Fascia Plane Block; Nerve Block
Citation: Al Misnid O. Regional anesthesia for axillary lymph node excisional biopsy in a patient with anterior mediastinal mass. Anaesth. pain intensive care 2025;29(2):354-357. DOI: 10.35975/apic.v29i2.2729
Received: February 11, 2025; Reviewed: February 14, 2025; Accepted: February 16, 2025
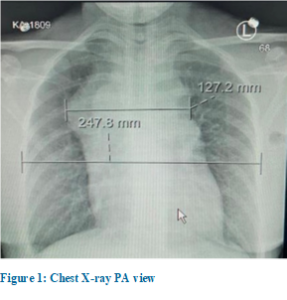
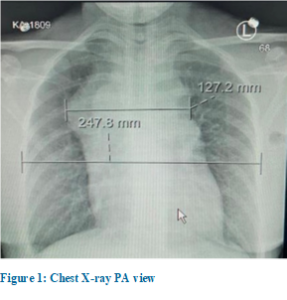
A 42-year-old female patient who was known to be medically fit and healthy, presented with multiple swellings in her upper body mainly in her neck and axillae for the last few months. She also suffered from night sweats, shortness of breath with cough, dysphagia, chocking at night and weight loss. The patient looked in distress, and upon examination she had generalized lymphadenopathy with compressive symptoms, fever, shortness of breath with productive cough, tachypnea and tachycardia. Initial work up was requested including laboratory work-up, chest X-ray (Figure 1), CT chest with contrast, echocardiography and lymph node biopsy.
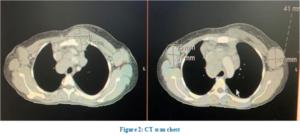
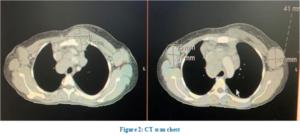
Laboratory investigations, including complete blood count, renal profile and liver function tests, were unremarkable, except for low hemoglobin, which was 96 g/L. CT chest with contrast showed multiple compartmental soft tissue masses involving the superior, anterior, and middle mediastinum. The largest mass measured 5.3 x 5.5 cm with mass effect on great thoracic vessels, the right side of pericardium, the anterior carina, and the right main stem bronchus (Figure 2). In addition, there was right lower lobe consolidation with mild bilateral pleural effusion, moderate pericardial effusion and bilateral axillary nodular masses, which suggested a diagnosis of lymphoma (Figure 2). The Echo showed moderate size pericardial effusion with elevated intrapericardial pressure without tamponade.
The patient was booked for left axillary lymph node excisional biopsy with high-risk consent for general anesthesia and intensive care bed standby for postoperative care. On the day of surgery, the primary anesthesiologist reviewed the patient carefully with a probability to postpone the procedure due to unavailability of intensive care bed and the risk of mass effect and active pneumonia. A detailed discussion took place among the patient, the surgeon, the anesthesiologist, and the primary team about the risks, the benefits, and the alternative approaches. The patient and the medical team agreed with the primary anesthesiologist plan to do the case with ultrasound guided pectoralis block (PECS) as the patient needed a definitive diagnosis to start the proper medical management. A previous needle biopsy had suggested lymphoma but the diagnosis was not conclusive.

In the operating room, the patient was placed in the supine position with slight back up to ensure patient comfort and cooperation during the regional block. The standard monitors were applied, which included pulse oximetry, non-invasive blood pressure, and ECG with two peripheral intravenous cannulas secured. Left sided ultrasound guided in-plane approach and 22G* 50 mm Sonoplex probe was used to perform PECS II under aseptic technique (Figure 3). A mixture of lidocaine 1% and ropivacaine 0.25% was used for the blocks. A total of 10 mL was injected between the pectoralis major and minor, and another 20 mL was injected below the pectoralis minor. Post injections, the patient's position was changed to Trendelenburg position with right side up for about 15 min with continuous communication and reassurance to the patient. The patient's position was adjusted for surgical exposure, and just before skin incision the surgical area was tested for pain with surgical forceps to ensure that the patient was pain free. A skin incision of 6 cm was carried out over left axilla with a huge lymph node under the incision measuring 5x3x4 cm, which was dissected with good hemostasis and no complication. Throughout the procedure the patient’s pain score was 0 out of 10 and vital signs showed no changes. The surgery was done without the use of sedation or local infiltration and the patient remained pain free and fully awake throughout the procedure. Afterwards, the patient was transferred to the post-anesthesia care unit (PACU), fully awake and vitally stable; she was monitored for two hours and remained hemodynamically stable with zero pain score. After 2 hours PACU monitoring, the patient was transferred to the oncology ward in a stable condition.
In certain cases, avoiding general anesthesia could be advisable for the patient safety. Our patient had a few reasons for us to avoid general anesthesia if feasible. Anesthesia for awake surgeries involving the axillary area can be very challenging and requires collaborative teamwork. In addition, such cases are particularly challenging to be done with a single injection regional block, although local anesthesia infiltration is a well-known technique, no described regional anesthesia block or technique s been identified to be ideal or superior for such surgeries and only very few case reports are found in the literatures. While some data recommends against the use of any regional techniques due to the anatomical challenges in the axilla and no technique could reliably provide sufficient analgesia to the axillary region.1 The innervation of axillary area consists of multiple contributions from nerves and groups of nerves. The intercostobrachial nerve (ICBN) is responsible for most of the cutaneous supply of the axilla, with contribution from the brachial plexus (BP) by providing additional cutaneous innervation from medial brachial cutaneous nerve (MBCN) and deep somatic innervation within the axilla mainly through the lateral and medial pectoral nerves.2 Other nerves arising from brachial plexus contributing to the anterolateral chest wall are, the thoracodorsal nerve, and the long thoracic nerve, which innervate latissimus dorsi, and serratus anterior muscles, respectively.3 The axilla is also innervated by the other lateral cutaneous branches of the thoracic intercostal nerve (LCNs) in addition to the ICBN (T2).
In addition to pure local anesthetic infiltration, such surgeries could be performed with various regional techniques, keeping in mind the essential coverage of ICBN, BP contribution mainly by medial and lateral pectoral nerves (MPN and LPN) and LCNs. For ICBN block, there are several reliable regional blocks that could cover this nerve like; targeting ICBN itself, high thoracic paravertebral, PECS II, or serratus anterior blocks. While MPN and LPN could be blocked if we do PECS I, PECS II (two pectoral fascial compartments) or supraclavicular BP block. While the LCNs will be blocked in case of paravertebral, PECS II or serratus anterior block are performed. In our case, PECS II was done as the primary anesthesia with no sedation, ideally the PECS II should block the MPN and LPN, the ICBN, the thoracodorsal, the long thoracic, and LCNs.3
In literature, regional block was used in few cases as the primary anesthesia for different procedures in the chest wall and axilla like; breast surgery, axillary dissection, transthoracic arteriovenous graft repair and cardiovascular implantable electronic device with or without sedation. In one case report, the author described a case of axillary clearance under regional blocks (supraclavicular BP and ICBN blocks).2 In another case, breast conserving surgery with axillary dissection was done using PECS II, with sedation in the form of dexmedetomidine infusion.4 While in another case PECS II was used as the sole anesthetic for removal of a large axillary tumor.5 A combination of PECS I, serratus anterior plane (SAP), and parasternal intercostal plane blocks with sedation in the form of propofol infusion was used for modified radical mastectomy and axillary lymph node dissection.6 Viewing such literature reinforces the limit of evidence, lack of guidelines, and wide discrepancy in the practice among anesthesiologists toward regional block preferences and opinions for surgeries involving the anterolateral chest wall and specifically the axilla.
Fascial plane blocks, in general, are still one of the new evolving debatable topics regarding their value, reliability and effectiveness. There is wide discrepancy in literature regarding effectiveness and reliability of fascial plane blocks, particularly about PECS block. However, most recent data favors development of such techniques.7 On the other hand, some studies show no benefit or even an increase in the reported pain scores after PECS group.7 In addition to the numerous factors which could affect the fascial plane blocks, Elsharkawy et al. described the basics of facial plane, and how many factors could influence the effectiveness, the quality and the spread of the block.8 Site of injection, volume of local anesthesia used, biomechanical properties of fascia, types of fascia and fascial layers and many other factors could influence the dermatomal spread and quality of the block.8 Raising the question of how well we understand and do the fascial plane block? To better understand the value of these factors, for example the site of injection in PECS II, injecting lateral to thoracoacromial branch and close to anterior axillary line for the superficial injection and injecting between the level of third and fourth rib over the anterior axillary line for the deeper one will result in more reliable block.3,9
In this case report, we not only suggest the potential of PECS block to reduce the intraoperative and postoperative opioid consumption and lower the pain scores, but also see a potential to be used as the primary anesthesia for selected surgeries. In addition to the factors which influence the success of facial plane block, carefully choosing which block to perform for a specific procedure is crucial to ensure a total pain free experience. For example, PECS II block is a great block in certain chest wall surgeries; however, it is a pure somatic block and doesn’t provide visceral block. So, for cases where visceral coverage is also needed, one should think of other blocks, e.g., erector spinae plane block or midpoint transverse process to pleura block.3
An efficient perioperative care of a patient starts with carful preoperative assessment and discussion with all involved medical teams, and of course the patient to formulate the best possible plan of care. Fascial plane blocks have potential to provide not only sensory block but also surgical block, when we understand and apply them for the right procedures and the right patients. Even in the axilla with its complex innervation, fascial plane blocks can offer a complete surgical anesthesia, perhaps with fewer side effects and complications in high risk patients.
4. Ethical considerations
Written permission from the patient was obtained to publish her case report and pictures, with the condition of concealing her identity.
5. Authors contribution
Omar Al Misnid was the sole author of this case report.
Author’s affiliation:
*Omar Al Misnid, Assistant Professor of Anesthesiology, Department of Emergency, Critical Care & Anesthesia, College of Medicine, Qassim University, Qassim, Saudi Arabia; Email: o.almisnid@qu.edu.sa; {ORCID:0000-0002-4147-9463}
Correspondence: Omar Al Misnid; Email: o.almisnid@qu.edu.sa
ABSTRACT
Regional blocks for the anterolateral chest wall are challenging in regard to the anatomical basics and innervation, the limitation of available evidence, lack of credible guidelines, and wide discrepancy in the existing practice among the health practitioners across the countries. Despite the challenges, recently new fascial plane blocks have been used more often as analgesic techniques. In very few occasions these techniques have been reported in literature as surgical blocks in certain cases where general anesthesia was not favorable or advisable. We present a challenging case in which the scheduled surgery had to be postponed due to high risk if done under general anesthesia, as she was concurrently suffering from multiple comorbidities and needed much status optimization. At the same time, her procedure was time sensitive to diagnose her medical illness and initiate the proper management.
Keywords: Regional Anesthesia; Pain Management; Fascia Plane Block; Nerve Block
Citation: Al Misnid O. Regional anesthesia for axillary lymph node excisional biopsy in a patient with anterior mediastinal mass. Anaesth. pain intensive care 2025;29(2):354-357. DOI: 10.35975/apic.v29i2.2729
Received: February 11, 2025; Reviewed: February 14, 2025; Accepted: February 16, 2025
1. CASE REPORT
A 42-year-old female patient who was known to be medically fit and healthy, presented with multiple swellings in her upper body mainly in her neck and axillae for the last few months. She also suffered from night sweats, shortness of breath with cough, dysphagia, chocking at night and weight loss. The patient looked in distress, and upon examination she had generalized lymphadenopathy with compressive symptoms, fever, shortness of breath with productive cough, tachypnea and tachycardia. Initial work up was requested including laboratory work-up, chest X-ray (Figure 1), CT chest with contrast, echocardiography and lymph node biopsy.
Laboratory investigations, including complete blood count, renal profile and liver function tests, were unremarkable, except for low hemoglobin, which was 96 g/L. CT chest with contrast showed multiple compartmental soft tissue masses involving the superior, anterior, and middle mediastinum. The largest mass measured 5.3 x 5.5 cm with mass effect on great thoracic vessels, the right side of pericardium, the anterior carina, and the right main stem bronchus (Figure 2). In addition, there was right lower lobe consolidation with mild bilateral pleural effusion, moderate pericardial effusion and bilateral axillary nodular masses, which suggested a diagnosis of lymphoma (Figure 2). The Echo showed moderate size pericardial effusion with elevated intrapericardial pressure without tamponade.
The patient was booked for left axillary lymph node excisional biopsy with high-risk consent for general anesthesia and intensive care bed standby for postoperative care. On the day of surgery, the primary anesthesiologist reviewed the patient carefully with a probability to postpone the procedure due to unavailability of intensive care bed and the risk of mass effect and active pneumonia. A detailed discussion took place among the patient, the surgeon, the anesthesiologist, and the primary team about the risks, the benefits, and the alternative approaches. The patient and the medical team agreed with the primary anesthesiologist plan to do the case with ultrasound guided pectoralis block (PECS) as the patient needed a definitive diagnosis to start the proper medical management. A previous needle biopsy had suggested lymphoma but the diagnosis was not conclusive.

In the operating room, the patient was placed in the supine position with slight back up to ensure patient comfort and cooperation during the regional block. The standard monitors were applied, which included pulse oximetry, non-invasive blood pressure, and ECG with two peripheral intravenous cannulas secured. Left sided ultrasound guided in-plane approach and 22G* 50 mm Sonoplex probe was used to perform PECS II under aseptic technique (Figure 3). A mixture of lidocaine 1% and ropivacaine 0.25% was used for the blocks. A total of 10 mL was injected between the pectoralis major and minor, and another 20 mL was injected below the pectoralis minor. Post injections, the patient's position was changed to Trendelenburg position with right side up for about 15 min with continuous communication and reassurance to the patient. The patient's position was adjusted for surgical exposure, and just before skin incision the surgical area was tested for pain with surgical forceps to ensure that the patient was pain free. A skin incision of 6 cm was carried out over left axilla with a huge lymph node under the incision measuring 5x3x4 cm, which was dissected with good hemostasis and no complication. Throughout the procedure the patient’s pain score was 0 out of 10 and vital signs showed no changes. The surgery was done without the use of sedation or local infiltration and the patient remained pain free and fully awake throughout the procedure. Afterwards, the patient was transferred to the post-anesthesia care unit (PACU), fully awake and vitally stable; she was monitored for two hours and remained hemodynamically stable with zero pain score. After 2 hours PACU monitoring, the patient was transferred to the oncology ward in a stable condition.
3. DISCUSSION
In certain cases, avoiding general anesthesia could be advisable for the patient safety. Our patient had a few reasons for us to avoid general anesthesia if feasible. Anesthesia for awake surgeries involving the axillary area can be very challenging and requires collaborative teamwork. In addition, such cases are particularly challenging to be done with a single injection regional block, although local anesthesia infiltration is a well-known technique, no described regional anesthesia block or technique s been identified to be ideal or superior for such surgeries and only very few case reports are found in the literatures. While some data recommends against the use of any regional techniques due to the anatomical challenges in the axilla and no technique could reliably provide sufficient analgesia to the axillary region.1 The innervation of axillary area consists of multiple contributions from nerves and groups of nerves. The intercostobrachial nerve (ICBN) is responsible for most of the cutaneous supply of the axilla, with contribution from the brachial plexus (BP) by providing additional cutaneous innervation from medial brachial cutaneous nerve (MBCN) and deep somatic innervation within the axilla mainly through the lateral and medial pectoral nerves.2 Other nerves arising from brachial plexus contributing to the anterolateral chest wall are, the thoracodorsal nerve, and the long thoracic nerve, which innervate latissimus dorsi, and serratus anterior muscles, respectively.3 The axilla is also innervated by the other lateral cutaneous branches of the thoracic intercostal nerve (LCNs) in addition to the ICBN (T2).
In addition to pure local anesthetic infiltration, such surgeries could be performed with various regional techniques, keeping in mind the essential coverage of ICBN, BP contribution mainly by medial and lateral pectoral nerves (MPN and LPN) and LCNs. For ICBN block, there are several reliable regional blocks that could cover this nerve like; targeting ICBN itself, high thoracic paravertebral, PECS II, or serratus anterior blocks. While MPN and LPN could be blocked if we do PECS I, PECS II (two pectoral fascial compartments) or supraclavicular BP block. While the LCNs will be blocked in case of paravertebral, PECS II or serratus anterior block are performed. In our case, PECS II was done as the primary anesthesia with no sedation, ideally the PECS II should block the MPN and LPN, the ICBN, the thoracodorsal, the long thoracic, and LCNs.3
In literature, regional block was used in few cases as the primary anesthesia for different procedures in the chest wall and axilla like; breast surgery, axillary dissection, transthoracic arteriovenous graft repair and cardiovascular implantable electronic device with or without sedation. In one case report, the author described a case of axillary clearance under regional blocks (supraclavicular BP and ICBN blocks).2 In another case, breast conserving surgery with axillary dissection was done using PECS II, with sedation in the form of dexmedetomidine infusion.4 While in another case PECS II was used as the sole anesthetic for removal of a large axillary tumor.5 A combination of PECS I, serratus anterior plane (SAP), and parasternal intercostal plane blocks with sedation in the form of propofol infusion was used for modified radical mastectomy and axillary lymph node dissection.6 Viewing such literature reinforces the limit of evidence, lack of guidelines, and wide discrepancy in the practice among anesthesiologists toward regional block preferences and opinions for surgeries involving the anterolateral chest wall and specifically the axilla.
Fascial plane blocks, in general, are still one of the new evolving debatable topics regarding their value, reliability and effectiveness. There is wide discrepancy in literature regarding effectiveness and reliability of fascial plane blocks, particularly about PECS block. However, most recent data favors development of such techniques.7 On the other hand, some studies show no benefit or even an increase in the reported pain scores after PECS group.7 In addition to the numerous factors which could affect the fascial plane blocks, Elsharkawy et al. described the basics of facial plane, and how many factors could influence the effectiveness, the quality and the spread of the block.8 Site of injection, volume of local anesthesia used, biomechanical properties of fascia, types of fascia and fascial layers and many other factors could influence the dermatomal spread and quality of the block.8 Raising the question of how well we understand and do the fascial plane block? To better understand the value of these factors, for example the site of injection in PECS II, injecting lateral to thoracoacromial branch and close to anterior axillary line for the superficial injection and injecting between the level of third and fourth rib over the anterior axillary line for the deeper one will result in more reliable block.3,9
In this case report, we not only suggest the potential of PECS block to reduce the intraoperative and postoperative opioid consumption and lower the pain scores, but also see a potential to be used as the primary anesthesia for selected surgeries. In addition to the factors which influence the success of facial plane block, carefully choosing which block to perform for a specific procedure is crucial to ensure a total pain free experience. For example, PECS II block is a great block in certain chest wall surgeries; however, it is a pure somatic block and doesn’t provide visceral block. So, for cases where visceral coverage is also needed, one should think of other blocks, e.g., erector spinae plane block or midpoint transverse process to pleura block.3
3. CONCLUSION
An efficient perioperative care of a patient starts with carful preoperative assessment and discussion with all involved medical teams, and of course the patient to formulate the best possible plan of care. Fascial plane blocks have potential to provide not only sensory block but also surgical block, when we understand and apply them for the right procedures and the right patients. Even in the axilla with its complex innervation, fascial plane blocks can offer a complete surgical anesthesia, perhaps with fewer side effects and complications in high risk patients.
4. Ethical considerations
Written permission from the patient was obtained to publish her case report and pictures, with the condition of concealing her identity.
5. Authors contribution
Omar Al Misnid was the sole author of this case report.
6. REFERENCES
- Jacobs A, Lemoine A, Joshi GP, Van de Velde M, Bonnet F, et al. PROSPECT guideline for oncological breast surgery: a systematic review and procedure specific postoperative pain management recommendations. Anaesthesia. 2020;75:664-73. [PubMed] DOI: 1111/anae.14964
- Munasinghe BM, Subramaniam N, Nimalan S, Sivamayuran P. Ultrasound to the rescue: axillary clearance under complete regional blockade. Case Rep Anesthesiol. 2021;2021:6655930. [PubMed] DOI: 1155/2021/6655930
- Chin KJ, Versyck B, Elsharkawy H, Rojas Gomez MF, Sala-Blanch X, Reina MA. Anatomical basis of fascial plane blocks. Reg Anesth Pain Med. 2021;46(7):581-99. [PubMed] DOI: 1136/rapm-2021-102506
- Moon EJ, Kim SB, Chung JY, Song JY, Yi JW. Pectoral nerve block (Pecs block) with sedation for breast conserving surgery without general anesthesia. Ann Surg Treat Res. 2017;93(3):166-9. [PubMed] DOI: 4174/astr.2017.93.3.166
- Van de Putte P, Blockmans D, De Rop C, Versyck B. Pectoral nerve block type II as the sole anesthetic for removal of a large axillary tumor: a case report. A A Pract. 2020;14(6):e01201. [PubMed] DOI: 1213/XAA.0000000000001201
- Bhakta P, Mac Sweeney K, O’Donnell BD. Chest wall regional anesthesia for modified radical mastectomy and axillary lymph node dissection: a case report. A A Pract. 2021;15(6):e01482. [PubMed] DOI: 1213/XAA.0000000000001482
- Bin Ghali K, AlKharraz N, Almisnid O, Alqarni A, Alyamani OA. The pectoral (PECS) regional block: a scoping review. Cureus. 2023;15(10):e46594. [PubMed] DOI: 7759/cureus.46594
- Elsharkawy H, Pawa A, Mariano ER. Interfascial plane blocks: back to basics. Reg Anesth Pain Med. 2018;43(4):341-6. [PubMed] DOI: 1097/AAP.0000000000000750
- Versyck B, Groen G, van Geffen GJ, Van Houwe P, Bleys RL. The pecs anesthetic blockade: a correlation between magnetic resonance imaging, ultrasound imaging, reconstructed cross-sectional anatomy and cross-sectional histology. Clin Anat. 2019;32(3):421-9. [PubMed] DOI: 1002/ca.23333