Ahmed Maamoun Soliman 1, Sameh S. Taha 2, Ashraf E. El Agamy 3, Mohamed I. El Seidy 4, Ahmed M. Youssef 5
Author affiliations:
ABSTRACT
Background & objective: The anesthetists have been experimenting with different modes of mechanical ventilation during general anesthesia. The objective of this study was to evaluate the efficacy of Pressure Controlled Ventilation-Volume Guaranteed (PCV-VG) mode in comparison to volume-controlled ventilation (VCV) mode in obese patients undergoing laparoscopic surgery in the Trendelenburg position, with a focus on their lung compliance and Oxygenation Index (OI).
Methodology: This randomized controlled clinical trial involved 64 obese patients of both sexes, with a Body Mass Index (BMI) of ≥30 kg/m², and classified as American Society of Anesthesiologists (ASA) class I or II. The participants were randomly assigned to one of the two groups: the study group (Group P) using PCV-VG and the control group (Group V) using VCV. Hemodynamic and respiratory parameters were monitored.
Results: The arterial oxygen partial pressure (PaO2) and lung compliance were significantly higher in Group P compared to Group V (P < 0.05). Conversely, the peak pressure (P peak) and plateau pressure (Pplat) along with the mean pressure (P mean) as well as the OI were significantly lower in Group P compared to Group V (P < 0.05).
Conclusion: PCV-VG significantly improves lung compliance and oxygenation while maintaining lower peak and plateau pressures, with comparable hemodynamic stability and PaCO2 levels.
Abbreviations: BMI: Body Mass Index, OI: Oxygenation Index, PCV-VG: Pressure Controlled Ventilation-Volume Guaranteed, PIP: Peak Inspiratory Pressure, PRVC- pressure-regulated volume-controlled, VT: tidal volume, VCV: volume-controlled ventilation
Keywords: Volume-Controlled Ventilation; Pressure-Controlled Ventilation Volume-Guaranteed; Trendelenburg Position; Obesity; Airway Pressures
Citation: Soliman AM, El Seidy MI, Taha SS, El Agamy AES, Youssef AM. Comparative study of the effects of volume-controlled ventilation vs. pressure-controlled volume guaranteed ventilation in patients with obesity during laparoscopic surgery. Anaesth. pain intensive care 2025;29(2):318-324. DOI: 10.35975/apic.v29i2.2722
Received: September 02, 2024; Reviewed: October 23, 2024; Accepted: January 01, 2025
Obesity is characterized by elevated resistance to airflow, difficulty in breathing, and reduced respiratory system compliance, with a Body Mass Index (BMI) exceeding 30 kg/m2.1
The combination of Carbon dioxide pneumoperitoneum with or without precipitous Trendelenburg positioning is typically necessary for assisted laparoscopic surgery to achieve an optimal surgical perspective. However, this approach can result in heightened airway pressure and adverse impacts on gas exchange. 2
Elevated atelectasis and cranial displacement of the diaphragm are consequences of carbon dioxide pneumoperitoneum in conjunction with steep Trendelenburg positioning. This condition leads to a reduction in total lung volume, decreased lung compliance, and decreased functional residual capacity. Therefore, the primary objectives of anesthetic management during laparoscopic-assisted surgery are to mitigate elevated airway pressures, enhance oxygenation, and facilitate the removal of carbon dioxide.3
In the context of laparoscopic assisted surgery, elevation of intraabdominal pressure due to CO2 pneumoperitoneum can lead to various complications. These complications may include deterioration in oxygenation, increase in airway pressure, reduction in lung volume and compliance, and elevated risk of atelectasis. Consequently, these factors can contribute to the development of hypercapnia, acidosis, and impaired oxygenation in patients.4
Volume-controlled ventilation (VCV) is the optimal method for general anesthesia administration. This mode of ventilation guarantees sufficient minute ventilation and delivers a target tidal volume (VT) through a constant flow. However, this approach can result in increased airway pressure in situations like laparoscopic assisted surgery.5
To obtain the optimal VT, the ventilator regulates the Peak Inspiratory Pressure (PIP) in Pressure-Controlled Ventilation Volume-Guaranteed (PCV-VG) mode. The ventilator parameters are consistently modified without altering the airway pressure to achieve the desired volume. Therefore, PCV-VG offers the benefits of both VCV and PCV in that it minimizes the occurrence of barotraumas while maintaining the target minute ventilation.6
PCV-VG is a type of controlled ventilation mode that integrates the characteristics of both Pressure Control Ventilation (PCV) and VCV. This mode functions as a pressure-regulated volume-controlled (PRVC) system employing autoflow ventilation. The design allows for a reduction in inspiratory pressure, which in turn, minimizes the risk of barotrauma.3
PCV-VG is a secure ventilation method without related deficiencies or even inferiority in maximal airway pressure, plateau pressure, and dynamic compliance, with the potential to offer advantages in terms of enhanced airway dynamics compared with VCV.7
Objective of the study
The study aimed to evaluate the efficacy of pressure-controlled ventilation volume-guaranteed (PCV-VG) and volume-controlled ventilation (VCV) modes in obese patients undergoing laparoscopic aided surgery in the Trendelenburg position with respect to lung compliance and Oxygenation Index (OI).
This investigation was registered in an investigational study with registration number NCT06117748 as a randomized controlled trial. We enrolled 64 obese patients, 21-60 years old of both sexes with BMI ≥ 30 kg/m2, ASA class I/ II and currently undergoing laparoscopic assisted surgery. The research was conducted over a span of one year following approval from our institutional ethics committee under reference number FMASU MD 280/2022. Written informed consent was obtained from all patients.
The criteria for exclusion were as follows: ASA III or IV, intraoperative hemodynamic instability, obese patients on home oxygen therapy, pneumoperitoneum with carbon dioxide with intra-abdominal pressure exceeding 14 mmHg, anti-Trendelenburg position, asthmatic patients, patients with advanced renal or liver disease, pulmonary hypertension and advanced malignancy. Pregnant ladies were also excluded.
The patients were divided into two equal categories: Group P (PCV-VG), representing the study group; and Group V (VCV), representing the control group. The use of a random number table and a closed envelope technique were implemented to randomly assign patients to one of the two categories.
Prior to surgery, a thorough medical history was obtained from each patient, followed by a comprehensive clinical examination. All pertinent investigations were reviewed, including complete blood count (CBC), coagulation profile, liver enzymes, kidney function tests, electrocardiogram (ECG), echocardiography (ECHO), pulmonary function tests, and arterial blood gas analysis (ABG). Subsequently, each patient was administered premedication ondansetron 8 mg and famotidine 20 mg intravenously. Monitoring included ECG, noninvasive blood pressure monitoring, and pulse oximetry. Following preoxygenation for 3-5 min, anesthesia was administered via fentanyl 1-2 µg/kg and propofol 2 mg/kg IV over a duration of 15 sec, and atracurium 0.5 mg/kg IV. Tracheal intubation was subsequently performed using a direct laryngoscopy. After confirming the endotracheal tube position through capnography, an arterial line was successfully inserted into the left radial artery using a 3-Fr Vygon catheter, after the performance of a modified Allen test.
The respiratory parameters were established as follows: VT 8 mL/kg body weight, respiratory rate 12 breaths/min, PEEP 5 mmHg, oxygen flow 4 L/min, inspired oxygen (FiO2) 0.6 %, and I:E ratio of 1:2. Anesthesia was maintained using 1.5-2.5 vol% end-tidal sevoflurane to regulate hemodynamic responses during the surgical procedure, keeping them within a 20% range of the preoperative values. The respiratory parameters were consistently monitored and maintained at a stable level with end-tidal carbon dioxide (EtCO2) kept below 45 mmHg. The patient was positioned supine, pneumoperitoneum was executed with carbon dioxide at an intraabdominal pressure of 14 mmHg, and then inclined to achieve a 30° Trendelenburg position. Lactated Ringer’s solution was administered continuously at a rate of 6-8 mL/kg/h throughout the study period.
Data collection
Mean arterial blood pressure (MAP) and heart rate (HR) were monitored for 10 min prior to anesthesia administration (T0), immediately after the onset of pneumoperitoneum, after every 10 min during the initial hour, and at the conclusion of surgery. The ABG’s were recorded at T0 and every 10 min during the initial hour to assess metabolic and respiratory changes. Peak airway pressure (P peak), plateau pressure (Pplat), mean airway pressure (P mean), and compliance of the respiratory system were recorded at T0 and at every 10 min in the initial hour.
Primary outcome was the Oxygenation Index (computed as mean airway pressure × FiO2 × 100/ PaO2). Secondary outcomes were MAP, HR, SpO2, PaCO2, and lung compliance.
Sample size calculation
A sample of least 32 cases per category (a total of 64 cases) achieves a power of 80% to detect an effect size of 0.3 within as well as between the groups using Repeated measures ANOVA with in-between factor with level of significance of 0.05. A correlation of at the most 0.5 was assumed between the repeated measures and 20% excess cases were added to compensate for the potential of drop-outs.8
Statistical analysis
All statistical analyses were performed using SPSS v26 (IBM Inc., Chicago, IL, USA). The mean and standard deviation (SD) of quantitative variables are presented. and contrasted between the two groups using an unpaired Student’s t-test. Frequencies and percentages (%) are employed to represent qualitative variables. and analyzed using the Chi-square test. Statistical significance is characterized by a two-tailed P-value <0.05.
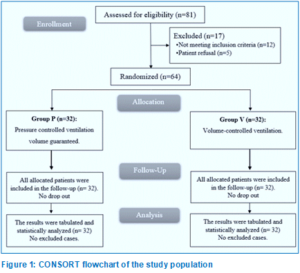
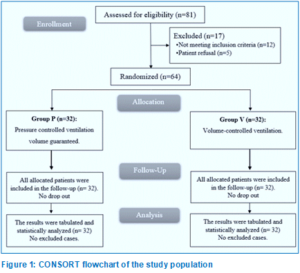
In this investigation, eligibility assessment was conducted for 81 patients, 12 patients did not satisfy the criteria, and 5 patients declined to participate in the investigation. The remaining patients were randomly assigned into one of the two equal groups (32 patients in each). The statistical analyses and follow-up of all allocated patients were conducted (Figure 1).
There were no significant differences between the two groups with respect to demographic data and duration of surgery (Table 1).
There was no significant difference in the values of mean HR, and MAP before induction, immediately after pneumoperitoneum, at 10 min after intubation, and at 10 min intervals between both groups (Table 2).
PaO2 at 20, 30, 40, 50 and 60 min was significantly increased in Group P than in Group V (P < 0.05). P peak at (20, 30, 40, 50 and 60 min and end of surgery) was significantly lower in Group P than in Group V (P < 0.05) (Table 3).
Pplat at T0 and 10 min, Pmean after intubation, lung compliance after intubation, and OI (after intubation, at 10 min and end of surgery) were not significantly different between both groups (Table 4).
Lung compliance at 10, 20, 30, 40, 50 and 60 min and at the end of surgery were significantly higher in Group P than in Group V (P < 0.05).
Pplat at 20, 30, 40, 50 and at 60 min and at the end of surgery, Pmean at 10, 20, 30, 40, 50 and 60 min and OI at (20, 30, 40, 50 and 60 min, were significantly lower in Group P than in Group V (P < 0.05) (Table 4).
CO2 pneumoperitoneum is frequently used in conjunction with the Trendelenburg position during laparoscopic interventions to ensure appropriate surgical viewing and space.9
These methods significantly affect cardiovascular and pulmonary systems. These conditions lead to increased mean arterial pressure, higher P peak, reduced pulmonary compliance, and increased risk of barotrauma or atelectasis.15
The objective minute ventilation can be ensured through the application of VCV in anesthesia; Nevertheless, a constant flow rate may lead to a greater PIP, which can exacerbate the risk of barotrauma and cause an imbalanced distribution of pulmonary gases.6
In our study, the MAP was not significantly different at all time points between both groups. Consistent with our results, Civraz et al. exhibited that there was no significant difference in MAP between VCV and PCV-VG in patients undergoing laparoscopic cholecystectomy.10
In the present study, PaO2 was statistically equivalent at 10 min and at the end of surgery between both groups and was significantly higher at 20, 30, 40, 50, and 60 min in Group P than in Group V (P < 0.05). Nevertheless, Civraz et al. showed no significant difference between VCV and PCV-VG in cases undergoing laparoscopic cholecystectomy regarding PaO2 at all measurement points. This finding may be attributable to the positional disparity and the time frame of the arterial blood gas analysis in the two investigations.10 Toker et al. found a significantly greater PaO2 in the PCV-VG mode employed in the Trendelenburg position in obese patients.5
In the current investigation, the P peak was insignificantly different after intubation and at 10 min between both groups and was significantly lower at 20, 30, 40, 50, and 60 min and the at the end of surgery in Group P than in Group V (P < 0.05). Ahmed et al. showed that there was a significantly higher P peak in the VCV group in contrast to PCV-VG at T1 (prior to pneumoperitoneum), T2 (15 min following pneumoperitoneum), and T3 (5 min following desufflation).11
In our study, Pplat was insignificantly different at T0 and at 10 min between the two groups and was significantly lower at all other time points of measurement in the Group P than in Group V (P < 0.001). In this context, Civraz et al. demonstrated that the Pplat results were significantly higher in the VCV group than in the PCV-VG group in patients undergoing laparoscopic cholecystectomy.10
In our study, lung compliance was insignificantly different after intubation between the two groups and was significantly higher at all other time points of measurement in Group P than in Group V (P < 0.05). Consistent with our findings, Civraz et al. found that compliance measures were significantly lower. in the VCV group than in the PCV-VG group (p < 0.05).10 Recently, a meta-analysis by Schick et al. comparing VCV and PCV-VG showed higher dynamic compliance of the lung in PCV-VG mode.12
In our study, the OI was insignificantly different after intubation, at 10 min, and at the end of surgery between both groups and was significantly lower at 20, 30, 40, 50, and 60 min in Group P than in Group V (P < 0.05). In line with our results, Toker et al. compared the VCV and PCV-VG modes in laparoscopic gynecologic surgery. In his study, he observed an increase in oxygenation in addition to the PCV-VG ventilation parameters.5 Some studies have noted a significantly high oxygenation (high PaO2) as well as improved ventilation with PCV mode; in contrast, other researchers did not observe any significant difference in relation to oxygenation and ventilation.13,14
The limitations of this investigation were the relatively small sample size and the single-center investigation.
PCV-VG is a superior strategy for ventilation compared with VCV in obese patients who undergo laparoscopic surgery in the Trendelenburg position. PCV-VG significantly enhances lung compliance and oxygenation while maintaining lower peak and plateau pressures with comparable hemodynamic stability and PaCO2.
7. Data availability
The numerical data generated during this research is available with the authors, and can be requested
8. Funding
The study utilized the hospital resources only, and no external or industry funding was involved.
9. Conflict of interest
All authors declare that there was no conflict of interests in the conduct of this study.
10. Authors’ contribution
AMS: Conduction of the study work
MES: Manuscript editing
SST, AMY: Literature search
AEG: Statistical analysis and review
Author affiliations:
- Ahmed Maamoun Soliman, Assistant Lecturer, Department of Anesthesia, ICU & Pain Faculty of Medicine Ain Shams University, Cairo, Egypt; Email: ahmedmaamounmaamoun2013@gmail.com, {ORCID:0000-0002-4402-9118}
- Mohamed Ismail El Seidy, Professor, Department of Anesthesia, ICU & Pain, Faculty of Medicine, Ain Shams University, Cairo, Egypt; Email: drmohamed_abdelfatah@med.asu.edu.eg, {ORCID:0009-0001-9010-3710}
- Sameh Salem Taha, Professor, Department of Anesthesia, ICU & Pain, Faculty of Medicine, Ain Shams University, Cairo, Egypt; Email:
drsamehtaha@med.asu.edu.eg, {ORCID:0000-0002-4761-0530} - Ashraf El Sayed El Agamy, Professor, Department of Anesthesia, ICU & Pain, Faculty of Medicine, Ain Shams University, Cairo, Egypt; Email: elagamy_ashraf@yahoo.com, {ORCID:0000-0001-6896-7662}
- Ahmed Monier Youssef, Lecturer, Department of Anesthesia, ICU & Pain, Faculty of Medicine, Ain Shams University, Cairo, Egypt; Email: ahmedmonier@med.asu.edu.eg, {ORCID:0000-0002-1354-4854}
ABSTRACT
Background & objective: The anesthetists have been experimenting with different modes of mechanical ventilation during general anesthesia. The objective of this study was to evaluate the efficacy of Pressure Controlled Ventilation-Volume Guaranteed (PCV-VG) mode in comparison to volume-controlled ventilation (VCV) mode in obese patients undergoing laparoscopic surgery in the Trendelenburg position, with a focus on their lung compliance and Oxygenation Index (OI).
Methodology: This randomized controlled clinical trial involved 64 obese patients of both sexes, with a Body Mass Index (BMI) of ≥30 kg/m², and classified as American Society of Anesthesiologists (ASA) class I or II. The participants were randomly assigned to one of the two groups: the study group (Group P) using PCV-VG and the control group (Group V) using VCV. Hemodynamic and respiratory parameters were monitored.
Results: The arterial oxygen partial pressure (PaO2) and lung compliance were significantly higher in Group P compared to Group V (P < 0.05). Conversely, the peak pressure (P peak) and plateau pressure (Pplat) along with the mean pressure (P mean) as well as the OI were significantly lower in Group P compared to Group V (P < 0.05).
Conclusion: PCV-VG significantly improves lung compliance and oxygenation while maintaining lower peak and plateau pressures, with comparable hemodynamic stability and PaCO2 levels.
Abbreviations: BMI: Body Mass Index, OI: Oxygenation Index, PCV-VG: Pressure Controlled Ventilation-Volume Guaranteed, PIP: Peak Inspiratory Pressure, PRVC- pressure-regulated volume-controlled, VT: tidal volume, VCV: volume-controlled ventilation
Keywords: Volume-Controlled Ventilation; Pressure-Controlled Ventilation Volume-Guaranteed; Trendelenburg Position; Obesity; Airway Pressures
Citation: Soliman AM, El Seidy MI, Taha SS, El Agamy AES, Youssef AM. Comparative study of the effects of volume-controlled ventilation vs. pressure-controlled volume guaranteed ventilation in patients with obesity during laparoscopic surgery. Anaesth. pain intensive care 2025;29(2):318-324. DOI: 10.35975/apic.v29i2.2722
Received: September 02, 2024; Reviewed: October 23, 2024; Accepted: January 01, 2025
1. INTRODUCTION
Obesity is characterized by elevated resistance to airflow, difficulty in breathing, and reduced respiratory system compliance, with a Body Mass Index (BMI) exceeding 30 kg/m2.1
The combination of Carbon dioxide pneumoperitoneum with or without precipitous Trendelenburg positioning is typically necessary for assisted laparoscopic surgery to achieve an optimal surgical perspective. However, this approach can result in heightened airway pressure and adverse impacts on gas exchange. 2
Elevated atelectasis and cranial displacement of the diaphragm are consequences of carbon dioxide pneumoperitoneum in conjunction with steep Trendelenburg positioning. This condition leads to a reduction in total lung volume, decreased lung compliance, and decreased functional residual capacity. Therefore, the primary objectives of anesthetic management during laparoscopic-assisted surgery are to mitigate elevated airway pressures, enhance oxygenation, and facilitate the removal of carbon dioxide.3
In the context of laparoscopic assisted surgery, elevation of intraabdominal pressure due to CO2 pneumoperitoneum can lead to various complications. These complications may include deterioration in oxygenation, increase in airway pressure, reduction in lung volume and compliance, and elevated risk of atelectasis. Consequently, these factors can contribute to the development of hypercapnia, acidosis, and impaired oxygenation in patients.4
Volume-controlled ventilation (VCV) is the optimal method for general anesthesia administration. This mode of ventilation guarantees sufficient minute ventilation and delivers a target tidal volume (VT) through a constant flow. However, this approach can result in increased airway pressure in situations like laparoscopic assisted surgery.5
To obtain the optimal VT, the ventilator regulates the Peak Inspiratory Pressure (PIP) in Pressure-Controlled Ventilation Volume-Guaranteed (PCV-VG) mode. The ventilator parameters are consistently modified without altering the airway pressure to achieve the desired volume. Therefore, PCV-VG offers the benefits of both VCV and PCV in that it minimizes the occurrence of barotraumas while maintaining the target minute ventilation.6
PCV-VG is a type of controlled ventilation mode that integrates the characteristics of both Pressure Control Ventilation (PCV) and VCV. This mode functions as a pressure-regulated volume-controlled (PRVC) system employing autoflow ventilation. The design allows for a reduction in inspiratory pressure, which in turn, minimizes the risk of barotrauma.3
PCV-VG is a secure ventilation method without related deficiencies or even inferiority in maximal airway pressure, plateau pressure, and dynamic compliance, with the potential to offer advantages in terms of enhanced airway dynamics compared with VCV.7
Objective of the study
The study aimed to evaluate the efficacy of pressure-controlled ventilation volume-guaranteed (PCV-VG) and volume-controlled ventilation (VCV) modes in obese patients undergoing laparoscopic aided surgery in the Trendelenburg position with respect to lung compliance and Oxygenation Index (OI).
2. METHODOLOGY
This investigation was registered in an investigational study with registration number NCT06117748 as a randomized controlled trial. We enrolled 64 obese patients, 21-60 years old of both sexes with BMI ≥ 30 kg/m2, ASA class I/ II and currently undergoing laparoscopic assisted surgery. The research was conducted over a span of one year following approval from our institutional ethics committee under reference number FMASU MD 280/2022. Written informed consent was obtained from all patients.
The criteria for exclusion were as follows: ASA III or IV, intraoperative hemodynamic instability, obese patients on home oxygen therapy, pneumoperitoneum with carbon dioxide with intra-abdominal pressure exceeding 14 mmHg, anti-Trendelenburg position, asthmatic patients, patients with advanced renal or liver disease, pulmonary hypertension and advanced malignancy. Pregnant ladies were also excluded.
The patients were divided into two equal categories: Group P (PCV-VG), representing the study group; and Group V (VCV), representing the control group. The use of a random number table and a closed envelope technique were implemented to randomly assign patients to one of the two categories.
Prior to surgery, a thorough medical history was obtained from each patient, followed by a comprehensive clinical examination. All pertinent investigations were reviewed, including complete blood count (CBC), coagulation profile, liver enzymes, kidney function tests, electrocardiogram (ECG), echocardiography (ECHO), pulmonary function tests, and arterial blood gas analysis (ABG). Subsequently, each patient was administered premedication ondansetron 8 mg and famotidine 20 mg intravenously. Monitoring included ECG, noninvasive blood pressure monitoring, and pulse oximetry. Following preoxygenation for 3-5 min, anesthesia was administered via fentanyl 1-2 µg/kg and propofol 2 mg/kg IV over a duration of 15 sec, and atracurium 0.5 mg/kg IV. Tracheal intubation was subsequently performed using a direct laryngoscopy. After confirming the endotracheal tube position through capnography, an arterial line was successfully inserted into the left radial artery using a 3-Fr Vygon catheter, after the performance of a modified Allen test.
The respiratory parameters were established as follows: VT 8 mL/kg body weight, respiratory rate 12 breaths/min, PEEP 5 mmHg, oxygen flow 4 L/min, inspired oxygen (FiO2) 0.6 %, and I:E ratio of 1:2. Anesthesia was maintained using 1.5-2.5 vol% end-tidal sevoflurane to regulate hemodynamic responses during the surgical procedure, keeping them within a 20% range of the preoperative values. The respiratory parameters were consistently monitored and maintained at a stable level with end-tidal carbon dioxide (EtCO2) kept below 45 mmHg. The patient was positioned supine, pneumoperitoneum was executed with carbon dioxide at an intraabdominal pressure of 14 mmHg, and then inclined to achieve a 30° Trendelenburg position. Lactated Ringer’s solution was administered continuously at a rate of 6-8 mL/kg/h throughout the study period.
Data collection
Mean arterial blood pressure (MAP) and heart rate (HR) were monitored for 10 min prior to anesthesia administration (T0), immediately after the onset of pneumoperitoneum, after every 10 min during the initial hour, and at the conclusion of surgery. The ABG’s were recorded at T0 and every 10 min during the initial hour to assess metabolic and respiratory changes. Peak airway pressure (P peak), plateau pressure (Pplat), mean airway pressure (P mean), and compliance of the respiratory system were recorded at T0 and at every 10 min in the initial hour.
Primary outcome was the Oxygenation Index (computed as mean airway pressure × FiO2 × 100/ PaO2). Secondary outcomes were MAP, HR, SpO2, PaCO2, and lung compliance.
Sample size calculation
A sample of least 32 cases per category (a total of 64 cases) achieves a power of 80% to detect an effect size of 0.3 within as well as between the groups using Repeated measures ANOVA with in-between factor with level of significance of 0.05. A correlation of at the most 0.5 was assumed between the repeated measures and 20% excess cases were added to compensate for the potential of drop-outs.8
Statistical analysis
All statistical analyses were performed using SPSS v26 (IBM Inc., Chicago, IL, USA). The mean and standard deviation (SD) of quantitative variables are presented. and contrasted between the two groups using an unpaired Student’s t-test. Frequencies and percentages (%) are employed to represent qualitative variables. and analyzed using the Chi-square test. Statistical significance is characterized by a two-tailed P-value <0.05.
3. RESULTS
In this investigation, eligibility assessment was conducted for 81 patients, 12 patients did not satisfy the criteria, and 5 patients declined to participate in the investigation. The remaining patients were randomly assigned into one of the two equal groups (32 patients in each). The statistical analyses and follow-up of all allocated patients were conducted (Figure 1).
There were no significant differences between the two groups with respect to demographic data and duration of surgery (Table 1).
There was no significant difference in the values of mean HR, and MAP before induction, immediately after pneumoperitoneum, at 10 min after intubation, and at 10 min intervals between both groups (Table 2).
PaO2 at 20, 30, 40, 50 and 60 min was significantly increased in Group P than in Group V (P < 0.05). P peak at (20, 30, 40, 50 and 60 min and end of surgery) was significantly lower in Group P than in Group V (P < 0.05) (Table 3).
| Table 1: Comparative demographic data and surgery duration in the groups | ||||
| Parameter | Group P
(n = 32) |
Group V
(n = 32) |
P value | |
| Age (years) | 42.38 ± 10.64 | 45.5 ± 11.29 | 0.259 | |
| Sex | Male | 15 (46.88%) | 11 (34.38%) | 0.309 |
| Female | 17 (53.13%) | 21 (65.63%) | ||
| Weight (kg) | 98.97 ± 14.63 | 104.09 ± 10.6 | 0.114 | |
| Height (cm) | 164.34 ± 6.3 | 166.97 ± 5.23 | 0.074 | |
| BMI (kg/m2) | 36.65 ± 5.1 | 37.47 ± 4.7 | 0.508 | |
| ASA physical status | I | 20 (62.5%) | 22 (68.75%) | 0.599 |
| II | 12 (37.5%) | 10 (31.25%) | ||
| Duration of surgery (min) | 55.31 ± 16.99 | 59.69 ± 16.65 | 0.302 | |
| Data presented as mean ± SD or frequency (%). BMI: Body mass index | ||||
| Table 2: Comparative hemodynamic data of the studied groups | ||||
| Parameter | Time | Group P
(n = 32) |
Group V
(n = 32) |
P value |
| HR (bpm) | Before induction (T0) | 77.09 ± 9.72 | 79.38 ± 8.54 | 0.323 |
| After pneumoperitoneum | 74.63 ± 9.69 | 77.72 ± 9.09 | 0.193 | |
| 10 min | 75.03 ± 9.65 | 77.91 ± 8.61 | 0.213 | |
| 20 min | 73.69 ± 9.82 | 76.81 ± 8.62 | 0.181 | |
| 30 min | 71.81 ± 9.78 | 75.34 ± 8.63 | 0.131 | |
| 40 min | 73.59 ± 10.03 | 72.66 ± 8.83 | 0.693 | |
| 50 min | 71.47 ± 9.76 | 75.44 ± 8.56 | 0.089 | |
| 60 min | 70.66 ± 9.48 | 74.31 ± 8.48 | 0.109 | |
| End of surgery | 72.56 ± 9.64 | 75.78 ± 8.85 | 0.169 | |
| MAP (mmHg) | Before induction (T0) | 93.5 ± 12.33 | 93.78 ± 10.96 | 0.923 |
| After pneumoperitoneum | 89.19 ± 12.24 | 92.03 ± 11.61 | 0.344 | |
| 10 min | 89.34 ± 12.49 | 92.13 ± 10.92 | 0.347 | |
| 20 min | 87.97 ± 12.28 | 91.41 ± 10.81 | 0.239 | |
| 30 min | 89.44 ± 12.39 | 87.66 ± 11.09 | 0.547 | |
| 40 min | 86.13 ± 12.44 | 89.41 ± 11.07 | 0.269 | |
| 50 min | 86.44 ± 12.91 | 89.78 ± 10.91 | 0.267 | |
| 60 min | 84.94 ± 12.46 | 88.66 ± 10.81 | 0.207 | |
| End of surgery | 87.19 ± 12.12 | 90.25 ± 11.33 | 0.300 | |
| Data are presented as mean ± SD; *Significant as P ≤ 0.05.
MAP: Mean arterial blood pressure. HR: heart rate |
||||
Pplat at T0 and 10 min, Pmean after intubation, lung compliance after intubation, and OI (after intubation, at 10 min and end of surgery) were not significantly different between both groups (Table 4).
| Table 3: Comparative PaO2, PaCO2 and Ppeak of the studied groups | ||||
| Parameter | Time | Group P
(n = 32) |
Group V
(n = 32) |
P value |
| PaO2 (mmHg) | 10 min | 181.75 ± 18.44 | 177.13 ± 18.92 | 0.326 |
| 20 min | 181.25 ± 18.66 | 166 ± 19.28 | 0.002* | |
| 30 min | 176.59 ± 18.97 | 163.75 ± 19.87 | 0.010* | |
| 40 min | 173.28 ± 18.82 | 160.47 ± 20.2 | 0.011* | |
| 50 min | 177.88 ± 18.41 | 168.09 ± 18.89 | 0.040* | |
| 60 min | 181.13 ± 18.56 | 170.81 ± 19.16 | 0.033* | |
| End of surgery | 182.06 ± 18.64 | 174.28 ± 19.62 | 0.109 | |
| PaCO2 (mmHg) | 10 min | 35.84 ± 4.33 | 36.69 ± 4.43 | 0.444 |
| 20 min | 35.88 ± 4.27 | 36.59 ± 4.32 | 0.506 | |
| 30 min | 35.03 ± 4.45 | 36.03 ± 4.4 | 0.369 | |
| 40 min | 36.78 ± 4.3 | 37.91 ± 4.28 | 0.298 | |
| 50 min | 37.28 ± 4.56 | 38 ± 4.43 | 0.525 | |
| 60 min | 38.31 ± 4.23 | 39.97 ± 4.75 | 0.146 | |
| End of surgery | 39.19 ± 4.4 | 40.31 ± 4.34 | 0.307 | |
| Ppeak (cmH2O) | After intubation(T0) | 15.38 ± 3.52 | 16.91 ± 4.31 | 0.124 |
| 10 min | 17.72 ± 3.4 | 18.84 ± 4.3 | 0.250 | |
| 20 min | 21.63 ± 4.01 | 24.56 ± 4.13 | 0.005* | |
| 30 min | 23.84 ± 4.21 | 27.06 ± 4.6 | 0.005* | |
| 40 min | 24.91 ± 3.4 | 28.13 ± 4.34 | 0.002* | |
| 50 min | 24.28 ± 3.67 | 27.56 ± 4.34 | 0.002* | |
| 60 min | 24.75 ± 3.95 | 29.06 ± 4.92 | < 0.001* | |
| End of surgery | 23.59 ± 3.26 | 26.81 ± 4.5 | 0.002* | |
| Data are presented as mean ± SD, PaO2: partial oxygen pressure. MAP: Mean arterial blood pressure. HR: heart rate *Significant as P ≤ 0.05. | ||||
Lung compliance at 10, 20, 30, 40, 50 and 60 min and at the end of surgery were significantly higher in Group P than in Group V (P < 0.05).
Pplat at 20, 30, 40, 50 and at 60 min and at the end of surgery, Pmean at 10, 20, 30, 40, 50 and 60 min and OI at (20, 30, 40, 50 and 60 min, were significantly lower in Group P than in Group V (P < 0.05) (Table 4).
4. DISCUSSION
CO2 pneumoperitoneum is frequently used in conjunction with the Trendelenburg position during laparoscopic interventions to ensure appropriate surgical viewing and space.9
These methods significantly affect cardiovascular and pulmonary systems. These conditions lead to increased mean arterial pressure, higher P peak, reduced pulmonary compliance, and increased risk of barotrauma or atelectasis.15
The objective minute ventilation can be ensured through the application of VCV in anesthesia; Nevertheless, a constant flow rate may lead to a greater PIP, which can exacerbate the risk of barotrauma and cause an imbalanced distribution of pulmonary gases.6
In our study, the MAP was not significantly different at all time points between both groups. Consistent with our results, Civraz et al. exhibited that there was no significant difference in MAP between VCV and PCV-VG in patients undergoing laparoscopic cholecystectomy.10
In the present study, PaO2 was statistically equivalent at 10 min and at the end of surgery between both groups and was significantly higher at 20, 30, 40, 50, and 60 min in Group P than in Group V (P < 0.05). Nevertheless, Civraz et al. showed no significant difference between VCV and PCV-VG in cases undergoing laparoscopic cholecystectomy regarding PaO2 at all measurement points. This finding may be attributable to the positional disparity and the time frame of the arterial blood gas analysis in the two investigations.10 Toker et al. found a significantly greater PaO2 in the PCV-VG mode employed in the Trendelenburg position in obese patients.5
In the current investigation, the P peak was insignificantly different after intubation and at 10 min between both groups and was significantly lower at 20, 30, 40, 50, and 60 min and the at the end of surgery in Group P than in Group V (P < 0.05). Ahmed et al. showed that there was a significantly higher P peak in the VCV group in contrast to PCV-VG at T1 (prior to pneumoperitoneum), T2 (15 min following pneumoperitoneum), and T3 (5 min following desufflation).11
| Table 4: Comparative ventilation and oxygenation indices | ||||
| Parameter | Time | Group P
(n = 32) |
Group V
(n = 32) |
P value |
| P plateau (cmH2O) | After intubation(T0) | 15.25 ± 3.39 | 13.91 ± 4.31 | 0.170 |
| 10 min | 17.53 ± 3.41 | 15.84 ± 4.3 | 0.087 | |
| 20 min | 21.38 ± 4 | 23.56 ± 4.13 | 0.035* | |
| 30 min | 23.72 ± 3.98 | 26.06 ± 4.6 | 0.033* | |
| 40 min | 24.88 ± 3.46 | 27.16 ± 5.02 | 0.038* | |
| 50 min | 24.13 ± 3.37 | 26.91 ± 4.79 | 0.009* | |
| 60 min | 24.56 ± 3.96 | 28.06 ± 4.63 | 0.002* | |
| End of surgery | 23.41 ± 3.39 | 25.94 ± 4.89 | 0.019* | |
| PMean (cmH2O) | After intubation(T0) | 8.19 ± 1.38 | 8.91 ± 2.1 | 0.111 |
| 10 min | 8.56 ± 1.54 | 10.47 ± 2.24 | < 0.001* | |
| 20 min | 9.81 ± 1.57 | 11.53 ± 2.26 | 0.001* | |
| 30 min | 9.69 ± 1.49 | 11.22 ± 2.2 | 0.002* | |
| 40 min | 9.78 ± 1.5 | 11.28 ± 2.26 | 0.003* | |
| 50 min | 9.63 ± 1.45 | 11.38 ± 2.12 | < 0.001* | |
| 60minP | 9.97 ± 1.67 | 11.78 ± 2.14 | < 0.001* | |
| End of surgery | 10.69 ± 1.35 | 12.53 ± 2.08 | < 0.001* | |
| Lung Compliance
(mL/cmH2O) |
After intubation(T0) | 42.72 ± 6.69 | 40.5 ± 8.2 | 0.240 |
| 10 min | 37.75 ± 7.22 | 30.75 ± 8.61 | 0.001* | |
| 20 min | 32.22 ± 7.16 | 27.53 ± 8.89 | 0.023* | |
| 30 min | 27.69 ± 6.78 | 23.69 ± 8.71 | 0.045* | |
| 40 min | 25.84 ± 6.65 | 21.94 ± 8.31 | 0.042* | |
| 50 min | 24.41 ± 6.63 | 17.16 ± 8.25 | < 0.001* | |
| 60 min | 22.06 ± 7.09 | 17.38 ± 8.51 | 0.020* | |
| End of surgery | 21.38 ± 7.38 | 17 ± 8.46 | 0.031* | |
| Oxygenation index
(OI) |
After intubation(T0) | 18.16 ± 1.27 | 18.38 ± 1.52 | 0.535 |
| 10 min | 13.31 ± 3.27 | 14.69 ± 2.9 | 0.080 | |
| 20 min | 13.66 ± 2.77 | 15.38 ± 2.54 | 0.012* | |
| 30 min | 12.94 ± 2.56 | 14.94 ± 2.65 | 0.003* | |
| 40 min | 13 ± 2.49 | 14.94 ± 2.35 | 0.002* | |
| 50 min | 13.13 ± 2.18 | 14.59 ± 2.84 | 0.024* | |
| 60 min | 13.81 ± 2.64 | 15.38 ± 2.46 | 0.017* | |
| End of surgery | 13.81 ± 2.68 | 15.06 ± 2.71 | 0.068 | |
| Data are presented as mean ± SD, *Significant as P ≤ 0.05. | ||||
In our study, Pplat was insignificantly different at T0 and at 10 min between the two groups and was significantly lower at all other time points of measurement in the Group P than in Group V (P < 0.001). In this context, Civraz et al. demonstrated that the Pplat results were significantly higher in the VCV group than in the PCV-VG group in patients undergoing laparoscopic cholecystectomy.10
In our study, lung compliance was insignificantly different after intubation between the two groups and was significantly higher at all other time points of measurement in Group P than in Group V (P < 0.05). Consistent with our findings, Civraz et al. found that compliance measures were significantly lower. in the VCV group than in the PCV-VG group (p < 0.05).10 Recently, a meta-analysis by Schick et al. comparing VCV and PCV-VG showed higher dynamic compliance of the lung in PCV-VG mode.12
In our study, the OI was insignificantly different after intubation, at 10 min, and at the end of surgery between both groups and was significantly lower at 20, 30, 40, 50, and 60 min in Group P than in Group V (P < 0.05). In line with our results, Toker et al. compared the VCV and PCV-VG modes in laparoscopic gynecologic surgery. In his study, he observed an increase in oxygenation in addition to the PCV-VG ventilation parameters.5 Some studies have noted a significantly high oxygenation (high PaO2) as well as improved ventilation with PCV mode; in contrast, other researchers did not observe any significant difference in relation to oxygenation and ventilation.13,14
| Table 5: Factors associated with time to full recovery of neuromuscular function | ||||
| Variables | n (%)
(n = 59) |
Time to reach TOF ratio ≥ 0.9 | P-value | |
| Sugammadex dose (mg/kg) | 4 | 37 (62.7) | 4.2 ± 1.8 | 0.255 |
| 2 | 22 (37.4) | 3.7 ± 1.8 | ||
| BMI (kg/cm2) | < 18.5 | 9 (15.3) | 4.8 ± 1.9 | 0.491 |
| 18.5 – 22.99 | 29 (49.2) | 4.0 ± 1.9 | ||
| 23 – 24.99 | 11 (18.6) | 3.7 ± 2.1 | ||
| ≥ 25 | 10 (16.9) | 3.6 ± 1.4 | ||
| ASA classification | I | 6 (10.2) | 3.0 ± 1.2 | 0.042 |
| II | 44 (74.6) | 3.9 ± 1.6 | ||
| III | 9 (15.3) | 5.3 ± 2.8 | ||
| Age (y) | < 65 | 36 (61) | 3.4 ± 1.3 | < 0.001 |
| ≥ 65 | 23 (39) | 4.9 ± 2.2 | ||
| Gender | Male | 32 (54.2) | 4.25 ± 2.2 | 0.291 |
| Female | 27 (45.8) | 3.74 ± 1.3 | ||
| Time between the last administration of rocuronium and the administration of sugammadex (min) | < 42 | 37 (62.7) | 4.0 ±1.6 | 0.743 |
| ≥ 42 | 22 (37.3) | 4.1 ± 2.3 | ||
| Duration of anesthesia (min) | < 120 | 6 (10.2) | 5.0 ± 2.2 | 0.327 |
| 120 – 180 | 15 (25.4) | 3.7 ± 1.6 | ||
| >180 | 38 (64.4) | 4.0 ± 1.8 | ||
| Total rocuronium used (mg) | < 83 | 33 (55.9) | 4.1 ± 1.6 | 0.832 |
| ≥ 83 | 26 (44.1) | 4.0 ± 2.1 | ||
| Total fentanyl used (µg) | < 218 | 40 (67.8) | 3.9 ± 1.7 | 0.397 |
| ≥ 218 | 19 (32.2) | 4.3 ± 2.0 | ||
| Values are given as frequency (percentage) or mean ± SD | ||||
5. LIMITATIONS
The limitations of this investigation were the relatively small sample size and the single-center investigation.
6. CONCLUSION
PCV-VG is a superior strategy for ventilation compared with VCV in obese patients who undergo laparoscopic surgery in the Trendelenburg position. PCV-VG significantly enhances lung compliance and oxygenation while maintaining lower peak and plateau pressures with comparable hemodynamic stability and PaCO2.
7. Data availability
The numerical data generated during this research is available with the authors, and can be requested
8. Funding
The study utilized the hospital resources only, and no external or industry funding was involved.
9. Conflict of interest
All authors declare that there was no conflict of interests in the conduct of this study.
10. Authors’ contribution
AMS: Conduction of the study work
MES: Manuscript editing
SST, AMY: Literature search
AEG: Statistical analysis and review
11. REFERENCES
- Shah U, Wong J, Wong DT, Chung F. Preoxygenation and intraoperative ventilation strategies in obese patients: a comprehensive review. Curr Opin Anaesthesiol. 2016;29:109-18. [PubMed] DOI: 1097/ACO.0000000000000267
- Choi EM, Na S, Choi SH, An J, Rha KH, Oh YJ. Comparison of volume-controlled and pressure-controlled ventilation in the Trendelenburg position for robot-assisted laparoscopic radical prostatectomy. J Clin Anesth. 2011;23:183-8. [PubMed] DOI: 1016/j.jclinane.2010.08.006
- Kim MS, Bai SJ, Lee JR, Choi YD, Kim YJ, Choi SH. Increase in intracranial pressure during carbon dioxide pneumoperitoneum with steep Trendelenburg positioning as proven by ultrasonographic measurement of the optic nerve sheath diameter. J Endourol. 2014;28:801-6. [PubMed] DOI: 1089/end.2014.0019
- Kim WH, Hahm TS, Kim JA, Sim WS, Choi DH, Lee EK, et al. Prolonged inspiratory time improves gas exchange in patients undergoing laparoscopic surgery: a randomized trial. Acta Anaesthesiol Scand. 2013;57:613-22. [PubMed] DOI: 1111/aas.12104
- Toker MK, Altıparmak B, Uysal A, Demirbilek SG. Comparison of pressure-controlled volume-guaranteed ventilation and volume-controlled ventilation in obese patients during gynecologic laparoscopic surgery in the Trendelenburg position. Braz J Anesthesiol. 2019;69:553-60. [PubMed] DOI: 1016/j.bjan.2019.09.003
- Pu J, Liu Z, Yang L, Wang Y, Jiang J. Application of pressure-controlled ventilation volume during one-lung ventilation in thoracic surgery. Int J Clin Exp Med. 2014;7:1094-8. [PubMed]
- Schick V, Dusse F, Eckardt R, Kerkhoff S, Commotio S, Hinkelbein J, et al. Comparison of volume-guaranteed vs targeted pressure-controlled ventilation with volume-controlled ventilation during elective surgery: a systematic review and meta-analysis. J Clin Med. 2021;10:1276. [PubMed] DOI: 3390/jcm10061276
- Faul F, Erdfelder E, Lang AG, Buchner A. G*Power III: a flexible statistical power analysis program for the social, behavioral, and biomedical sciences. Behav Res Methods. 2007;39:175-91. [PubMed] DOI: 3758/bf03193146
- Li J, Ma S, Chang X, Ju S, Zhang M, Yu D, et al. Effect of pressure-controlled ventilation-volume guaranteed mode combined with individualized positive end-expiratory pressure on respiratory mechanics, oxygenation, and lung injury in patients undergoing laparoscopic surgery in Trendelenburg position. J Clin Monit Comput. 2022;36:1155-64. [PubMed] DOI: 1007/s10877-021-00750-9
- Turan Civraz AZ, Saracoglu A, Saracoglu KT. Evaluation of the effect of pressure-controlled ventilation-volume guaranteed mode vs volume-controlled ventilation on atelectasis in patients undergoing laparoscopic surgery: a randomized controlled clinical trial. Medicina (Kaunas). 2023;59. [PubMed] DOI: 3390/medicina59101783
- Ahmed MH, Ismael MM, Salem AM. Effect of volume, pressure, and pressure control-volume guaranteed ventilation on cardiovascular parameters and pulmonary mechanics in obese patients undergoing laparoscopic sleeve gastrectomy. Al-Azhar Intern Med J. 2022;51:1199-208.
- Schick V, Dusse F, Eckardt R, Kerkhoff S, Commotio S, Hinkelbein J, et al. Comparison of volume-guaranteed versus targeted pressure-controlled ventilation during elective surgery: a systematic review and meta-analysis. J Clin Med. 2021;10. [PubMed] DOI: 3390/jcm10061276
- Gupta SD, Kundu SB, Ghose T, Maji S, Mitra K, Mukherjee M, et al. A comparison between volume-controlled ventilation and pressure-controlled ventilation for providing better oxygenation in obese patients undergoing laparoscopic cholecystectomy. Indian J Anaesth. 2012;56:276-82. [PubMed] DOI: 4103/0019-5049.98777
- Movassagi R, Montazer M, Mahmoodpoor A, Fattahi V, Iranpour A, Sanaie S. Comparison of pressure vs volume controlled ventilation on oxygenation parameters of obese patients undergoing laparoscopic cholecystectomy. Pak J Med Sci. 2017;33:1117-22. [PubMed] DOI: 12669/pjms.335.13316
- Arvizo C, Mehta ST, Yunker A. Adverse events related to Trendelenburg position during laparoscopic surgery: recommendations and review of the literature. Curr Opin Obstet Gynecol. 2018;30:272-8. [PubMed] DOI: 1097/GCO.0000000000000471