Mohamed Hassan Saleh Mohamed El Razzaz 1, Gehan Fouad Kamel Youssif 2, Sherif Samir Wahba 3, Shimaa Ahmed Mohamed 4, Ahmed Moustafa Mohamed Mohamed 5
Authors affiliations:
Background& objective: Femoral Triangle Block (FTB) offers an efficient pain relief in total knee arthroplasty (TKA), except the anteromedial cutaneous region which may not be completely anesthetized by solely utilizing FTB. Therefore, adding the Anterior Femoral Cutaneous Nerve Block (AFCNB) to the FTB could provide complete pain relief. Adductor Canal Block (ACB) is a common technique to provide analgesia after total knee arthroplasty. In the current study, we assessed and contrasted the effectiveness of ultrasound (US) guided AFCNB plus FTB versus ACB regarding analgesia and early mobilization after TKA.
Methodology: Sixty patients who had total knee arthroplasty were randomly assigned into two equivalent groups; Group A which obtained AFCNB in Combination with FTB or Group B which received ACB before the beginning of the surgery. After completion of the desired block, spinal anesthesia was given under complete aseptic conditions. The primary outcome was comparison of the time to first request of the post-operative rescue pethidine in the case of visual analogue scale (VAS) score above 3. Secondary outcomes were the total amount of rescue pethidine used, VAS scores and time to ambulation. Immediate postoperative complications of the given nerve blocks and the adverse effects of the used drugs were recorded and managed accordingly.
Results: Sixty participants successfully finished the study. No significant statistical differences between both groups were noted at the time of request of the first post-operative rescue pethidine (P = 0.159). Additionally, there was no statistical difference concerning postoperative VAS between the two groups except at 8 hours and 20 hours where Group A showed a statistically significant lower VAS than Group B (P = 0.039 and 0.005 respectively). However, Group A consumed a statistically significant smaller total amount of pethidine than Group B (P = 0.030). Conversely, Group B showed a shorter duration than Group A regarding ‘Timed Up and Go’ test (TUG) at 12 hours and 24 hours post operatively with a high statistically significant difference between them (P< 0.001 in both). Incidence of complications and adverse effects of the used drugs was comparable between the two groups without significant difference.
Conclusion: We concluded that AFCNB in combination with FTB provided better analgesic and pethidine-sparing effects compared to ACB after TKA. However, ACB provided better preservation of motor function and provided early ambulation.
Abbreviations: ACB: Adductor canal block, AFCNB: Anterior Femoral Cutaneous Nerve Block, FTB: Femoral Triangle Block, TKA: Total knee arthroplasty, VAS: visual analogue pain scale
Keywords: Anterior Femoral Cutaneous Nerve Block; Femoral Triangle Block; Adductor Canal Block; Anesthesia; Total Knee Arthroplasty
Citation: Mohamed ElRazzaz MHS, Kamel Youssif GF, Wahba SS, Mohamed SA, Mohamed AM. Analgesic efficacy of ultrasound guided anterior femoral cutaneous nerve block (AFCNB) plus femoral triangle block (FTB) vs. adductor canal block (ACB) in total knee arthroplasty. Anaesth. pain intensive care 2025;29(2):232-241.
DOI: 10.35975/apic.v29i2.2709
Received: May 09, 2024; Reviewed: October 26, 2024; Accepted: January 01, 2025
Total knee arthroplasty (TKA) is a frequently carried out procedure aimed at alleviating joint discomfort in individuals suffering from rheumatic arthritis or end-stage osteoarthritis of the knee. Nevertheless, TKA is often accompanied by moderate to severe pain after surgery, which can hinder postoperative rehabilitation, lower patient satisfaction, and negatively impact overall outcomes.1
Multiple approaches have been utilized to enhance post-TKA pain. One of them is the femoral triangle block (FTB), which involves administering a local anesthetic injection near the adductor canal. The purpose is to numb the additional terminal branches of the femoral nerve to enhance pain relief following knee surgery. The disadvantage is the increased motor weakness of the quadriceps muscle.2
The medial parapatellar technique is the most employed surgical method for TKA, providing exposure to the majority of structures in the anteromedial region of the knee. The anterior femoral cutaneous nerve (AFCN) supplies sensation to the anteromedial cutaneous areas of the lower thigh and knee and is comprised of the intermediate and medial cutaneous nerves of the thigh.3 The FTB might not fully numb these nerves, so the AFCN block is included alongside FTB to help with postoperative pain control.4
The ultrasound guided adductor canal block (ACB) is a useful procedure for anterior knee pain relief that preserves motor function, offering sensory anesthesia while having little impact on quadriceps muscles strength. The local anesthetic is administered into the distal adductor canal to block the femoral nerve.5
The objective of this study was to evaluate and compare the analgesic efficacy of the anterior femoral cutaneous nerve block plus femoral triangle block with the adductor canal block in total knee arthroplasty. The main variables were the time to the first request for post-operative rescue pethidine, patient pain report on the visual analogue scale, total analgesic requirements, functional performance and ambulation.
This prospective, randomized comparative clinical trial was approved by the research ethics committee (REC) of the Faculty of Medicine, Ain Shams University, Cairo, Egypt (Approval number is FWA 000017585, FMASU MD 291/2022). Additionally, the study was registered with the Pan African Clinical Trial Registry (PACTR), with the ID. 202312753143536.
To calculate the sample size, G power software (version 3.1.9.4) was utilized, with a power level of 80%, an alpha error rate of 5%, and an anticipated medium effect size (0.3) for the difference in pain scores. The pain scores were determined by VAS in all patients. Based on that, a sample size of at least sixty patients undergoing TKA, with thirty patients in each group, was adequate to meet the objectives of the study.
The study was conducted at Ain Shams University Hospitals from December 2022 to July 2024 on sixty patients, ranging in age from 40 and 80 y, Physical Status of American Society of Anesthesiologists (ASA) I, II or III, planned for elective TKA under spinal anesthesia, voluntarily joined the study after giving written informed consent. Individuals who declined participation or had an ASA physical status IV were not included. Also, we excluded patients exhibiting infection at the injection site, bleeding disorders or coagulopathy, having multiple fractures, known allergies to local anesthetics, with previous neuropathy or myopathy, patients who received long-acting opioids preoperatively, refusal of spinal anesthesia or major spine deformities precluding spinal anesthesia, uncooperative patients with significant cognitive dysfunction or psychiatric illness.
2.1. Study procedure and anesthetic protocol
All patients underwent a preoperative assessment and were asked to observe an 8-hour fasting period. The enrolled sixty participants were randomly assigned into two equivalent groups; every group included thirty patients, utilizing computer-generated random number tables. Group A patients received AFCNB in combination with FTB. Whereas Group B patients received ACB. After completion of the desired block, spinal anesthesia was given to both groups under complete aseptic conditions.
Prior to the surgery, in the operation theatre, standard monitoring was done including SpO2, respiratory rate (breaths/min), pulse rate (beats per min), NIBP (mmHg) and ECG. Intravenous access was set up and an intravenous infusion of lactated Ringer's solution @ 5-10 mL/kg/h started. Midazolam 0.01-0.1 mg/kg was titrated as an anxiolytic.
Before administration of spinal anesthesia and under complete sterile conditions, nerve blocks were done with an echogenic B-bevel, 22-gauge, 80-mm nerve block needle (B. Braun, Melsungen, Germany) using a high-frequency linear array US transducer (6 to 13 MHz, M-Turbo, Sonosite, USA) to perform a dynamic scan of the anatomy of the intended nerve blocks. Patients were categorized at random to one of the two treatment groups based on the type of nerve block administered:
2.1.1. Anterior femoral cutaneous nerve block (AFCNB):
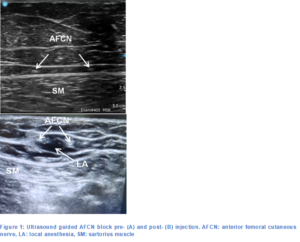
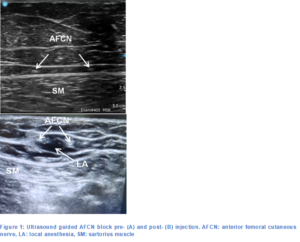
AFCNB was conducted by positioning the transducer along the upper to middle third of the thigh. Once the location of the superficial femoral artery under the sartorius muscle (SM) was pinpointed on the ultrasound image, the transducer was adjusted slightly upwards to determine the best position of the SFA underneath the medial edge of the SM in the ultrasound. Then the transducer was slid up and down the fascia above sartorius muscle to identify the best image of the AFCN.6 Post- delivering of 1−2 mL of 1% lidocaine to anesthetize the skin, an echogenic B-bevel needle was inserted from the lateral-to-medial direction employing an in-plane procedure and then the needle was preceded until the needle tip was superficial to the fascia lata above the sartorius muscle.7 Following this, 10 mL of 0.25% bupivacaine was gradually delivered after meticulous aspiration as the needle was carefully inserted just above the fascia lata enveloping the SM, until the local anesthetic encased the nerve8 (Figure1).
2.1.2. Femoral triangle block (FTB):
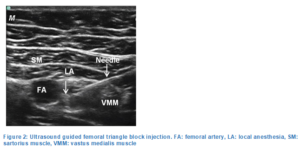
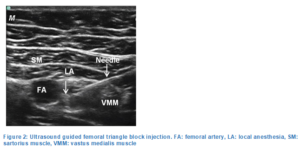
The femoral nerve was identified by ultrasound and was seen anterolateral and adjacent to the femoral artery in a short-axis view, approximately ten cm distal to the midpoint of the inguinal ligament inside the femoral triangle and deep to the sartorius muscle. The needle was positioned parallel to the ultrasound beam and threaded through the sartorius muscle. The end point of injection was peri-arterial spread of local anesthetic around the anterolateral part of the femoral artery to anesthetize the femoral nerve, the medial vastus muscle nerve, and the medial femoral cutaneous nerve. A 10 mL of 0.25% bupivacaine was injected slowly through the needle following a thorough aspiration. The solution was observed diffusing in a peri-arterial manner around the femoral artery9 (Figure 2).
2.1.3. Group B (ACB group):
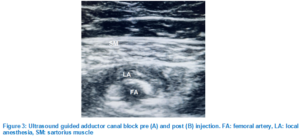
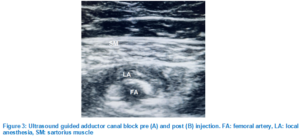
Adductor canal block (ACB) was performed while the patient was lying on their back with the knee slightly bent and externally rotated, the ultrasound probe was positioned longitudinally at the middle of the thighand femoral artery was visualized. The probe was subsequently shifted medially and distally to locate a spot between the distal and middle thirds of the thigh, where the artery is positioned deep beneath the sartorius muscle and just before the adductor hiatus. At this point, the femoral nerve was found anterolateral to the artery. The needle was positioned in-plane from the lateral side toward the medial direction until the tip was located just above the femoral artery. Following this, 20 mL of 0.25% bupivacaine was given7(Figure 3).
In both groups, a total volume of 20 mL of 0.25% bupivacaine hydrochloride as 2.5mg/mL was prepared by adding an equal volume (1:1) of normal saline (0.9%) to 0.5% bupivacaine taking into consideration not to exceed the total toxic dose (2.5mg/kg).
After completion of the desired block, spinal anesthesia was administered in a fully sterile environment using a 25G Quincke needle was inserted through the L3-L4 or L4-L5 intervertebral space. The procedure involved injecting 3.5 mL of 0.5% hyperbaric bupivacaine combined with 25 µg of fentanyl. Once the onset of the sensory block was verified, its level was recorded, and the surgeon was permitted to begin the procedure.
Hypotension (a drop in systolic blood pressure of 20% or more from the baseline) was treated with ephedrine 100 µg/kg intravenously, diluted in 10 mL of 0.9% normal saline. Bradycardia (HR < 60 BPM), if accompanied by hypotension or any signs of impaired perfusion, was treated with atropine 10 µg/kg. Supplemental oxygen was given by O2 mask 10 L/min to keep SpO2 > 92%.
Postoperative nausea and vomiting (PONV) required inj. ondansetron 4 mg in 10 mL of 0.9% normal saline, slow IV for 10 min.
In case of failure of spinal anesthesia, patient received general anesthesia and was excluded from the study.
2.2. Data collection
Demographic data, including age, sex, body mass index (BMI) in (kg/m2) and ASA, for every patient, were documented preoperatively.
Hemodynamic data; e.g., respiratory rate (RR), peripheral oxygen saturation (SpO2), heart rate (HR), and mean arterial blood pressure (MAP) were recorded before anesthesia, immediately after both blocks, every 30 min during surgery and each 4 h for the initial 24 h postoperative.
Postoperative pain was assessed and recorded at VAS at 0 hour, then after every 30 min for the first 2 h, then every 4 h for the initial 24 h. Rescue analgesia, inj pethidine 25 mg IV given in case of VAS >3. Time to first request for a pain-killer and the total amount of opioids used for each patient in each group, were recorded.
The ‘Timed Up and Go’ (TUG) test was recorded in seconds; Baseline (preoperative, performed independently), then at 12 and 24 h postoperative (done with the assistance of a walker). Patients were instructed to stand up from a chair, walk 3 m, return to the chair, and then sit again. The duration of this entire process, from beginning to end, was measured in seconds.
Duration of surgery and spinal anesthesia in minutes for every patient in each group were recorded. Immediate complications of the nerve blocks were recorded and managed accordingly e.g., hematomas formation etc. Adverse effects of the used drugs (bupivacaine, fentanyl, pethidine) were recorded and managed accordingly.
The primary objective of the study was to evaluate and compare postoperative analgesia in both groups using the time of the first request for the rescue pethidine. Secondary outcomes were the total rescue pethidine consumption in 24 h postoperatively, VAS, time to ambulation (TUG test), immediate complications of the used nerve blocks and side effects of the used drugs during the first 24 h postoperatively.
End Point: 24 h postoperatively.
2.3. Statistical analysis and package
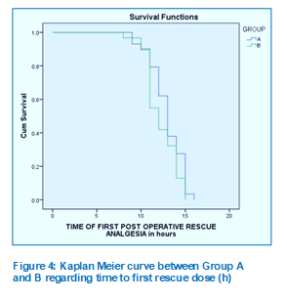
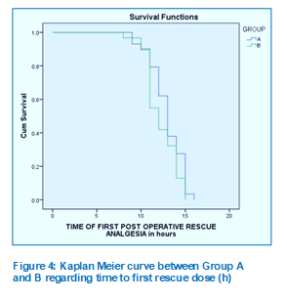
Data were collected, coded, tabulated, and then analyzed employing Statistical Package for Social Science (SPSS) software package (IBM SPSS Statistics for Windows, Version 22.0. Armonk, NY: IBM Corp., 2013). Numerical variables were presented as mean ± standard deviation (SD) or median (Q3-Q1), and categorical variables were presented as frequency and percentages (%). Comparisons of numerical variables were done using t-test or Mann-Whitney test as appropriate, while comparisons of categorical variables were done using chi-square test. The interval until the initial rescue analgesia was assessed through Kaplan-Meier Survival analysis and the log-Rank test (Figure 4). With a 95% confidence interval, a P < 0.05 indicates statistical significance, while a P <0.001 was deemed highly significant.
Seventy-four patients were assessed for eligibility, and sixty-four patients were included in the study. Final analysis of sixty patients was done as four patients were lost to follow up.
Regarding age, sex, ASA physical status, and BMI in (kg/m2), there was no statistically significant difference among the two groups. The time of spinal anesthesia was less in Group A than Group B and the difference was statistically significant (P = 0.008). Similarly, the duration of surgery was shorter in the Group A than Group B. The difference was statistically not significant (P = 0.143) (Table I).
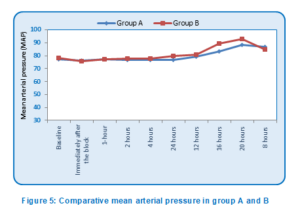
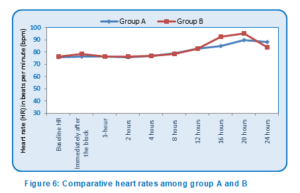
At the baseline, there was no statistical difference among both groups regarding MAP, immediately after the block and at 1, 2, 4, 12 and 24 h post-operatively. However, Group A showed a statistically significant lower MAP than Group B at 8 (P = 0.006), 16 h (P = 0.006) and 20 h(P = 0.005) postoperatively (Figure5). Regarding HR, there was no statistical difference among both groups at the baseline, immediately after the block and at 1, 2, 4, 8, and 12 h post-operatively. However, Group A showed a statistically significant lower HR than Group B at 16 h, 20 h and 24 h postoperatively (P = 0.005, 0.005 and 0.018, respectively) (Figure 6).
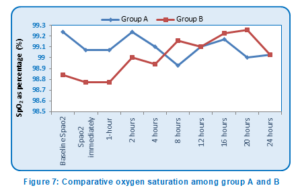
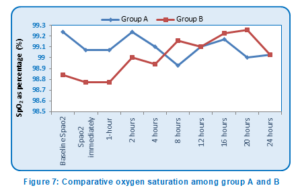
Both groups were comparable regarding SpO2 at baseline, immediately after the block and at 1, 2, 4, 8, 12, 16, 20 and 24 h post-operatively with no statistical differences between them (Figure 7).
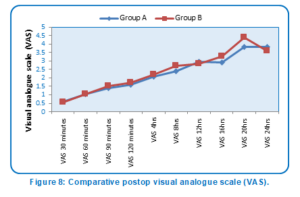
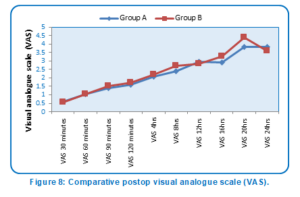
There was no statistical difference in the VAS scores among the two groups, at 30, 60, 90, 120 min and at 4, 12, and 16 h postoperatively. However, Group A showed a statistically significant lower postoperative VAS scores than Group B at 8 h and 20 h (P = 0.039 and 0.005, respectively) (Table 2; Figure 8).
Both groups were comparable as regards baseline TUG test with no significant difference. However, Group B showed a shorter duration than Group A regarding TUG test at 12 h and 24 h postoperatively with significant difference (P < 0.001 in both) (Table 3).
There was no significant difference among Group A and B as regards time to first request for rescue pethidine (P = 0.159) (Table 4). Group A consumed a significantly smaller total amount of pethidine than Group B (P = 0.030) (Table 4).
Both groups were statistically equivalent regarding the incidence of hematoma formation, itching due to fentanyl and nausea and vomiting due to pethidine (Table 5).
In thisrandomized prospective comparative clinical study, although we found that the difference in time of request of the first post-surgery rescue pethidine was longer in Group A (mean 12.93h) than Group B (mean 12.26 h) the result was statistically non-significant (P = 0.159).We found also that Group A had superior postoperative analgesic effect with a statistically significant lower postoperative VAS score than Group B only at 8 h and 20 h in the first 24h (P = 0.039 and 0.005, respectively). However, there was a statistically significant difference regarding the amount of pethidine consumption, as Group A consumed less pethidine than Group B.
Also, the study done by Kampitak et al. demonstrating the pain-relieving effectiveness of combining AFCNB with FTB in TKA showed similar outcomes conceding with our study. The addition of AFCNB in FTB led to lower postoperative pain scores at 6 and 24 h in comparison to femoral triangle block Group (P < 0.001and 0.014, respectively). It also provided cutaneous anesthesia around the surgical incision site and the medial side of the knee post-TKA, while FTB alone failed to achieve this effect.10
Furthermore, in a study done by De Arzuaga et al., they used single injection nerve blocks for TKA; FNB versus FTB versus ACB with comparable results to our study. There was no significant difference regarding pain scores and morphine usage among FNB group and FTB group. Conversely, patients in the FNB group exhibited considerably less pain at rest in relation to those in the ACB group, both at the 6-hour and 24-hour marks (P = 0.02 and 0.005, respectively). Also, the opioids requirement in ACB was significantly higher at 6 h and 24 h (P = 0.001 and 0.01, respectively).11
Additionally, according to research conducted by Song et al., they compared the ultrasound-guided single injection femoral triangle block without the AFCN block versus ACBfor analgesia after TKA. The FTB group demonstrated notably reduced pain levels both at rest and while movement 12 and 24 h after TKA compared to the adductor canal group (P = 0.008 and 0.005, respectively).12
Also, our results were compatible with a study done by Bjørn et al., in which they similarly added the AFCNB to the FTB which provided superior analgesia than FTB alone with coverage of the surgical aspect.4
In our study, we found that Group B showed better ambulation evaluated by the ‘Timed Up and Go’ test (TUG) than Group A during the first 12 and 24 h. The findings were comparable to those from the study by Wang et al., which compared the ACB with the FTB in the TKA. In that study, the ACB group demonstrated greater quadriceps strength than the FTB group at 4, 8, and 24 h postoperatively(P<0.05). However, they stated that ACB provided more effective analgesia than FTB group (P = 0.013).2
Opposite to our study, Jæger et al. concluded in their comparative study between the ACB versus FNB for analgesia after TKA that ACB provided similar analgesia and morphine consumption in comparison to femoral nerve block but with more quadriceps muscle power preservation.13 Additionally, Li et al. concluded in their study on the analgesic efficacy and their effect on the quadriceps strength of ACB versus FNB following TKA that ACB group was similarly exhibited better quadriceps strength than femoral nerve block but without significant differences in pain score during rest or activity and opioid usage among the two groups.14 Also, Wang et al., concluded in their comparative study between ACB and FTB impact on postoperative pain following TKA that ACB provided more effective analgesia and quadriceps strength than FTB alone during the first 24 h (P = 0.013 and 0.001 respectively).2
Incidentally, the duration of spinal anesthesia in our study was shorter in Group A than Group B and this difference being statistically significant (P = 0.008). On the other hand, while the duration of surgery was also shorter in Group A than Group B, yet this difference was not statistically significant (P = 0.143)
Finally, our study blocks were safe regarding the occurrence of postoperative complications and adverse effects as hematoma, itching due to fentanyl, nausea and vomiting due to pethidine where there was an overall lower incidence of each without significant difference between both groups.
First, it was a single-center study, and additional research is necessary to determine whether our findings from a single center can be generalized. Second, surgeons were not the same in all cases with variable skills and speed. Third, we did not implement a multimodal approach to pain management, which may have resulted in inadequate analgesia. Finally, all preoperative block procedures were conducted by an experienced anaesthetist who knew about the study groups, which may have introduced bias in the execution of the blocks and interpretation of the results.
Ultrasound guided anterior femoral cutaneous nerve block in combination with femoral triangle block may be a valid alternative to ultrasound guided adductor canal block as the regional analgesic technique within a multimodal pain management regimen for total knee arthroplasty patients. Combination of anterior femoral cutaneous nerve block and femoral triangle block provide superior analgesia and pethidine sparing effects when compared to adductor canal block. However, adductor canal block provided better preservation of motor function and allowed early ambulation.
7. Data availability
The numerical data generated during this research is available with the authors.
8. Funding
We gratefully thank Faculty of Medicine, Ain Shams University, Cairo, Egypt for providing us an opportunity to complete this research..
9. Conflict of interest
The authors did not disclose any possible conflicts of interest.
10. Authors’ contribution
MH: Conduct of the study work.
GF: Manuscript editing.
SS, SA: Literature search.
AM: Statistical analysis and review.
Authors affiliations:
- Mohamed Hassan Saleh Mohamed ElRazzaz,Assistant Lecturer of Anesthesia, Intensive Care & Pain Management, Faculty of Medicine, Ain Shams University, Cairo, Egypt; Email: mohamed.h.saleh@med.asu.edu.eg
- Gehan Fouad Kamel Youssif, Professor of Anesthesia, Intensive Care & Pain Management, Faculty of Medicine, Ain Shams University, Cairo, Egypt; Email: Drgehan_youssif@med.asu.edu.eg
- Sherif Samir Wahba, Professor of Anesthesia, Intensive Care & Pain Management, Faculty of Medicine, Ain Shams University, Cairo, Egypt; Email: sherifwahba2012@yahoo.com
- Shimaa Ahmed Mohamed, Lecturer of Anesthesia, Intensive Care & Pain Management, Faculty of Medicine, Ain Shams University, Cairo, Egypt; Email: Shimaaahmed_2011@yahoo.com
- Ahmed Moustafa Mohamed Mohamed,Lecturer of Anesthesia, Intensive Care & Pain Management, Faculty of Medicine, Ain Shams University, Cairo, Egypt; Email: drahmed.mostafa.mohamed@med.asu.edu.eg
ABSTRACT
Background& objective: Femoral Triangle Block (FTB) offers an efficient pain relief in total knee arthroplasty (TKA), except the anteromedial cutaneous region which may not be completely anesthetized by solely utilizing FTB. Therefore, adding the Anterior Femoral Cutaneous Nerve Block (AFCNB) to the FTB could provide complete pain relief. Adductor Canal Block (ACB) is a common technique to provide analgesia after total knee arthroplasty. In the current study, we assessed and contrasted the effectiveness of ultrasound (US) guided AFCNB plus FTB versus ACB regarding analgesia and early mobilization after TKA.
Methodology: Sixty patients who had total knee arthroplasty were randomly assigned into two equivalent groups; Group A which obtained AFCNB in Combination with FTB or Group B which received ACB before the beginning of the surgery. After completion of the desired block, spinal anesthesia was given under complete aseptic conditions. The primary outcome was comparison of the time to first request of the post-operative rescue pethidine in the case of visual analogue scale (VAS) score above 3. Secondary outcomes were the total amount of rescue pethidine used, VAS scores and time to ambulation. Immediate postoperative complications of the given nerve blocks and the adverse effects of the used drugs were recorded and managed accordingly.
Results: Sixty participants successfully finished the study. No significant statistical differences between both groups were noted at the time of request of the first post-operative rescue pethidine (P = 0.159). Additionally, there was no statistical difference concerning postoperative VAS between the two groups except at 8 hours and 20 hours where Group A showed a statistically significant lower VAS than Group B (P = 0.039 and 0.005 respectively). However, Group A consumed a statistically significant smaller total amount of pethidine than Group B (P = 0.030). Conversely, Group B showed a shorter duration than Group A regarding ‘Timed Up and Go’ test (TUG) at 12 hours and 24 hours post operatively with a high statistically significant difference between them (P< 0.001 in both). Incidence of complications and adverse effects of the used drugs was comparable between the two groups without significant difference.
Conclusion: We concluded that AFCNB in combination with FTB provided better analgesic and pethidine-sparing effects compared to ACB after TKA. However, ACB provided better preservation of motor function and provided early ambulation.
Abbreviations: ACB: Adductor canal block, AFCNB: Anterior Femoral Cutaneous Nerve Block, FTB: Femoral Triangle Block, TKA: Total knee arthroplasty, VAS: visual analogue pain scale
Keywords: Anterior Femoral Cutaneous Nerve Block; Femoral Triangle Block; Adductor Canal Block; Anesthesia; Total Knee Arthroplasty
Citation: Mohamed ElRazzaz MHS, Kamel Youssif GF, Wahba SS, Mohamed SA, Mohamed AM. Analgesic efficacy of ultrasound guided anterior femoral cutaneous nerve block (AFCNB) plus femoral triangle block (FTB) vs. adductor canal block (ACB) in total knee arthroplasty. Anaesth. pain intensive care 2025;29(2):232-241.
DOI: 10.35975/apic.v29i2.2709
Received: May 09, 2024; Reviewed: October 26, 2024; Accepted: January 01, 2025
1. INTRODUCTION
Total knee arthroplasty (TKA) is a frequently carried out procedure aimed at alleviating joint discomfort in individuals suffering from rheumatic arthritis or end-stage osteoarthritis of the knee. Nevertheless, TKA is often accompanied by moderate to severe pain after surgery, which can hinder postoperative rehabilitation, lower patient satisfaction, and negatively impact overall outcomes.1
Multiple approaches have been utilized to enhance post-TKA pain. One of them is the femoral triangle block (FTB), which involves administering a local anesthetic injection near the adductor canal. The purpose is to numb the additional terminal branches of the femoral nerve to enhance pain relief following knee surgery. The disadvantage is the increased motor weakness of the quadriceps muscle.2
The medial parapatellar technique is the most employed surgical method for TKA, providing exposure to the majority of structures in the anteromedial region of the knee. The anterior femoral cutaneous nerve (AFCN) supplies sensation to the anteromedial cutaneous areas of the lower thigh and knee and is comprised of the intermediate and medial cutaneous nerves of the thigh.3 The FTB might not fully numb these nerves, so the AFCN block is included alongside FTB to help with postoperative pain control.4
The ultrasound guided adductor canal block (ACB) is a useful procedure for anterior knee pain relief that preserves motor function, offering sensory anesthesia while having little impact on quadriceps muscles strength. The local anesthetic is administered into the distal adductor canal to block the femoral nerve.5
The objective of this study was to evaluate and compare the analgesic efficacy of the anterior femoral cutaneous nerve block plus femoral triangle block with the adductor canal block in total knee arthroplasty. The main variables were the time to the first request for post-operative rescue pethidine, patient pain report on the visual analogue scale, total analgesic requirements, functional performance and ambulation.
2. METHODOLOGY
This prospective, randomized comparative clinical trial was approved by the research ethics committee (REC) of the Faculty of Medicine, Ain Shams University, Cairo, Egypt (Approval number is FWA 000017585, FMASU MD 291/2022). Additionally, the study was registered with the Pan African Clinical Trial Registry (PACTR), with the ID. 202312753143536.
To calculate the sample size, G power software (version 3.1.9.4) was utilized, with a power level of 80%, an alpha error rate of 5%, and an anticipated medium effect size (0.3) for the difference in pain scores. The pain scores were determined by VAS in all patients. Based on that, a sample size of at least sixty patients undergoing TKA, with thirty patients in each group, was adequate to meet the objectives of the study.
The study was conducted at Ain Shams University Hospitals from December 2022 to July 2024 on sixty patients, ranging in age from 40 and 80 y, Physical Status of American Society of Anesthesiologists (ASA) I, II or III, planned for elective TKA under spinal anesthesia, voluntarily joined the study after giving written informed consent. Individuals who declined participation or had an ASA physical status IV were not included. Also, we excluded patients exhibiting infection at the injection site, bleeding disorders or coagulopathy, having multiple fractures, known allergies to local anesthetics, with previous neuropathy or myopathy, patients who received long-acting opioids preoperatively, refusal of spinal anesthesia or major spine deformities precluding spinal anesthesia, uncooperative patients with significant cognitive dysfunction or psychiatric illness.
2.1. Study procedure and anesthetic protocol
All patients underwent a preoperative assessment and were asked to observe an 8-hour fasting period. The enrolled sixty participants were randomly assigned into two equivalent groups; every group included thirty patients, utilizing computer-generated random number tables. Group A patients received AFCNB in combination with FTB. Whereas Group B patients received ACB. After completion of the desired block, spinal anesthesia was given to both groups under complete aseptic conditions.
Prior to the surgery, in the operation theatre, standard monitoring was done including SpO2, respiratory rate (breaths/min), pulse rate (beats per min), NIBP (mmHg) and ECG. Intravenous access was set up and an intravenous infusion of lactated Ringer's solution @ 5-10 mL/kg/h started. Midazolam 0.01-0.1 mg/kg was titrated as an anxiolytic.
Before administration of spinal anesthesia and under complete sterile conditions, nerve blocks were done with an echogenic B-bevel, 22-gauge, 80-mm nerve block needle (B. Braun, Melsungen, Germany) using a high-frequency linear array US transducer (6 to 13 MHz, M-Turbo, Sonosite, USA) to perform a dynamic scan of the anatomy of the intended nerve blocks. Patients were categorized at random to one of the two treatment groups based on the type of nerve block administered:
2.1.1. Anterior femoral cutaneous nerve block (AFCNB):
AFCNB was conducted by positioning the transducer along the upper to middle third of the thigh. Once the location of the superficial femoral artery under the sartorius muscle (SM) was pinpointed on the ultrasound image, the transducer was adjusted slightly upwards to determine the best position of the SFA underneath the medial edge of the SM in the ultrasound. Then the transducer was slid up and down the fascia above sartorius muscle to identify the best image of the AFCN.6 Post- delivering of 1−2 mL of 1% lidocaine to anesthetize the skin, an echogenic B-bevel needle was inserted from the lateral-to-medial direction employing an in-plane procedure and then the needle was preceded until the needle tip was superficial to the fascia lata above the sartorius muscle.7 Following this, 10 mL of 0.25% bupivacaine was gradually delivered after meticulous aspiration as the needle was carefully inserted just above the fascia lata enveloping the SM, until the local anesthetic encased the nerve8 (Figure1).
2.1.2. Femoral triangle block (FTB):
The femoral nerve was identified by ultrasound and was seen anterolateral and adjacent to the femoral artery in a short-axis view, approximately ten cm distal to the midpoint of the inguinal ligament inside the femoral triangle and deep to the sartorius muscle. The needle was positioned parallel to the ultrasound beam and threaded through the sartorius muscle. The end point of injection was peri-arterial spread of local anesthetic around the anterolateral part of the femoral artery to anesthetize the femoral nerve, the medial vastus muscle nerve, and the medial femoral cutaneous nerve. A 10 mL of 0.25% bupivacaine was injected slowly through the needle following a thorough aspiration. The solution was observed diffusing in a peri-arterial manner around the femoral artery9 (Figure 2).
2.1.3. Group B (ACB group):
Adductor canal block (ACB) was performed while the patient was lying on their back with the knee slightly bent and externally rotated, the ultrasound probe was positioned longitudinally at the middle of the thighand femoral artery was visualized. The probe was subsequently shifted medially and distally to locate a spot between the distal and middle thirds of the thigh, where the artery is positioned deep beneath the sartorius muscle and just before the adductor hiatus. At this point, the femoral nerve was found anterolateral to the artery. The needle was positioned in-plane from the lateral side toward the medial direction until the tip was located just above the femoral artery. Following this, 20 mL of 0.25% bupivacaine was given7(Figure 3).
In both groups, a total volume of 20 mL of 0.25% bupivacaine hydrochloride as 2.5mg/mL was prepared by adding an equal volume (1:1) of normal saline (0.9%) to 0.5% bupivacaine taking into consideration not to exceed the total toxic dose (2.5mg/kg).
After completion of the desired block, spinal anesthesia was administered in a fully sterile environment using a 25G Quincke needle was inserted through the L3-L4 or L4-L5 intervertebral space. The procedure involved injecting 3.5 mL of 0.5% hyperbaric bupivacaine combined with 25 µg of fentanyl. Once the onset of the sensory block was verified, its level was recorded, and the surgeon was permitted to begin the procedure.
Hypotension (a drop in systolic blood pressure of 20% or more from the baseline) was treated with ephedrine 100 µg/kg intravenously, diluted in 10 mL of 0.9% normal saline. Bradycardia (HR < 60 BPM), if accompanied by hypotension or any signs of impaired perfusion, was treated with atropine 10 µg/kg. Supplemental oxygen was given by O2 mask 10 L/min to keep SpO2 > 92%.
Postoperative nausea and vomiting (PONV) required inj. ondansetron 4 mg in 10 mL of 0.9% normal saline, slow IV for 10 min.
In case of failure of spinal anesthesia, patient received general anesthesia and was excluded from the study.
2.2. Data collection
Demographic data, including age, sex, body mass index (BMI) in (kg/m2) and ASA, for every patient, were documented preoperatively.
Hemodynamic data; e.g., respiratory rate (RR), peripheral oxygen saturation (SpO2), heart rate (HR), and mean arterial blood pressure (MAP) were recorded before anesthesia, immediately after both blocks, every 30 min during surgery and each 4 h for the initial 24 h postoperative.
Postoperative pain was assessed and recorded at VAS at 0 hour, then after every 30 min for the first 2 h, then every 4 h for the initial 24 h. Rescue analgesia, inj pethidine 25 mg IV given in case of VAS >3. Time to first request for a pain-killer and the total amount of opioids used for each patient in each group, were recorded.
The ‘Timed Up and Go’ (TUG) test was recorded in seconds; Baseline (preoperative, performed independently), then at 12 and 24 h postoperative (done with the assistance of a walker). Patients were instructed to stand up from a chair, walk 3 m, return to the chair, and then sit again. The duration of this entire process, from beginning to end, was measured in seconds.
Duration of surgery and spinal anesthesia in minutes for every patient in each group were recorded. Immediate complications of the nerve blocks were recorded and managed accordingly e.g., hematomas formation etc. Adverse effects of the used drugs (bupivacaine, fentanyl, pethidine) were recorded and managed accordingly.
The primary objective of the study was to evaluate and compare postoperative analgesia in both groups using the time of the first request for the rescue pethidine. Secondary outcomes were the total rescue pethidine consumption in 24 h postoperatively, VAS, time to ambulation (TUG test), immediate complications of the used nerve blocks and side effects of the used drugs during the first 24 h postoperatively.
End Point: 24 h postoperatively.
2.3. Statistical analysis and package
Data were collected, coded, tabulated, and then analyzed employing Statistical Package for Social Science (SPSS) software package (IBM SPSS Statistics for Windows, Version 22.0. Armonk, NY: IBM Corp., 2013). Numerical variables were presented as mean ± standard deviation (SD) or median (Q3-Q1), and categorical variables were presented as frequency and percentages (%). Comparisons of numerical variables were done using t-test or Mann-Whitney test as appropriate, while comparisons of categorical variables were done using chi-square test. The interval until the initial rescue analgesia was assessed through Kaplan-Meier Survival analysis and the log-Rank test (Figure 4). With a 95% confidence interval, a P < 0.05 indicates statistical significance, while a P <0.001 was deemed highly significant.
3. RESULTS
Seventy-four patients were assessed for eligibility, and sixty-four patients were included in the study. Final analysis of sixty patients was done as four patients were lost to follow up.
Regarding age, sex, ASA physical status, and BMI in (kg/m2), there was no statistically significant difference among the two groups. The time of spinal anesthesia was less in Group A than Group B and the difference was statistically significant (P = 0.008). Similarly, the duration of surgery was shorter in the Group A than Group B. The difference was statistically not significant (P = 0.143) (Table I).
| Table I: Comparative demographic data, duration of spinal anesthesia and surgery (min) | ||||
| Demographic data | Group A
(n = 30) |
Group B
(n = 30) |
P-value | |
| Age in years | 64.72 ± 6.290 | 65.39 ± 4.660 | 0.643 | |
| Sex | Female | 14 (46.7) | 14 (46.7) | 0.802 |
| Male | 16 (53.3) | 16 (53.3) | ||
| Body mass index in kg/m2 | 29.48 ± 3.934 | 30.42 ± 4.064 | 0.369 | |
| ASA | I | 5 (16.6) | 4 (13.33) | 0.804 |
| II | 20 (66.6) | 22 (73.34) | ||
| III | 5 (16.6) | 4 (13.33) | ||
| Duration of spinal anesthesia | 124.07 ± 7.846 | 129.84 ± 8.315 | 0.008 | |
| Duration of surgery | 100.10 ± 9.120 | 103.48 ± 8.520 | 0.143 | |
| T-independent sample t-test for mean ± SD; ꭓ2: Chi-square test for number (%) or Fisher’s exact test when appropriate; P <0.05 considered as significant | ||||
| Table 2: Comparative postop visual analogue scale (VAS) score | |||
| Time | Visual Analogue Scale (VAS) score | P-value | |
| Group A
(n = 30) |
Group B
(n = 30) |
||
| 30 min post-operative | 0.62 ± 0.494 | 0.55 ± 0.506 | 0.578 |
| 60 min post-operative | 1.03 ± 0.421 | 1.06 ± 0.680 | 0.839 |
| 90 min post-operative | 1.38 ± 0.622 | 1.52 ± 0.570 | 0.378 |
| 120 min post-operative | 1.59 ± 0.628 | 1.71 ± 0.643 | 0.455 |
| 4 h post-operative | 2.07 ± 0.458 | 2.19 ± 0.543 | 0.342 |
| 8 h post-operative | 2.38 ± 0.561 | 2.71 ± 0.643 | 0.039 |
| 12 h post-operative | 2.97 ± 0.981 | 2.84 ± 0.735 | 0.572 |
| 16 h post-operative | 2.93 ± 0.998 | 3.29 ± 0.902 | 0.148 |
| 20 h post-operative | 3.83 ± 0.805 | 4.39 ± 0.667 | 0.005 |
| 24 h post-operative | 3.83 ± 0.759 | 3.58 ± 0.720 | 0.201 |
| Employing: U = Mann-Whitney test for non-parametric data; Data showa mean ± SD; P <0.05 considered as significant | |||
| Table 3: Timed Up and Go (TUG) test (sec) | |||
| Time | Group A
(n = 30) |
Group B
(n = 30) |
p-value |
| Baseline TUG test (sec) | 25.69 ± 3.892 | 24.58 ± 3.294 | 0.237 |
| TUG test 12 h postoperative (sec) | 82.28 ± 7.015 | 71.39 ± 7.636 | <0.001 |
| TUG test 24 h postoperative (sec) | 70.62 ± 6.826 | 60.10 ± 7.630 | <0.001 |
| Using unpaired student-t test for mean ± SD; P <0.05 considered as significant | |||
| Table 4: Time to first request for the rescue analgesia (h) and total amount of rescue pethidine | |||
| Time | Group A
(n = 30) |
Group B
(n = 30) |
P-value |
| Time of request of the first postoperative rescue pethidine (h) | 12.93 ± 1.870 | 12.26 ± 1.788 | 0.159 |
| Total amount of postoperative rescue pethidine (mg) | 78.45 ± 17.326 | 89.61 ± 21.126 | 0.03 |
| Unpaired student-t test for mean ± SD; P <0.05 considered as significant | |||
| Table 5: Comparative incidence of complications | |||
| Complications | Group A
(n = 30) |
Group B (n = 30) |
P-value |
| Hematoma formation | 1 (3.3) | 1 (3.3) | 1.000 |
| Itching due to Fentanyl | 1 (3.3) | 1 (3.3) | 1.000 |
| Nausea and vomiting due to Pethidine | 2 (6.67) | 2 (6.67) | 1.000 |
| ꭓ2: Chi-square test for number (%) or Fisher’s exact test when appropriate; P <0.05 considered as significant | |||
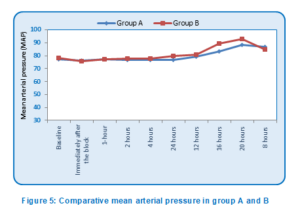
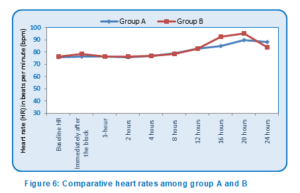
At the baseline, there was no statistical difference among both groups regarding MAP, immediately after the block and at 1, 2, 4, 12 and 24 h post-operatively. However, Group A showed a statistically significant lower MAP than Group B at 8 (P = 0.006), 16 h (P = 0.006) and 20 h(P = 0.005) postoperatively (Figure5). Regarding HR, there was no statistical difference among both groups at the baseline, immediately after the block and at 1, 2, 4, 8, and 12 h post-operatively. However, Group A showed a statistically significant lower HR than Group B at 16 h, 20 h and 24 h postoperatively (P = 0.005, 0.005 and 0.018, respectively) (Figure 6).
Both groups were comparable regarding SpO2 at baseline, immediately after the block and at 1, 2, 4, 8, 12, 16, 20 and 24 h post-operatively with no statistical differences between them (Figure 7).
There was no statistical difference in the VAS scores among the two groups, at 30, 60, 90, 120 min and at 4, 12, and 16 h postoperatively. However, Group A showed a statistically significant lower postoperative VAS scores than Group B at 8 h and 20 h (P = 0.039 and 0.005, respectively) (Table 2; Figure 8).
Both groups were comparable as regards baseline TUG test with no significant difference. However, Group B showed a shorter duration than Group A regarding TUG test at 12 h and 24 h postoperatively with significant difference (P < 0.001 in both) (Table 3).
There was no significant difference among Group A and B as regards time to first request for rescue pethidine (P = 0.159) (Table 4). Group A consumed a significantly smaller total amount of pethidine than Group B (P = 0.030) (Table 4).
Both groups were statistically equivalent regarding the incidence of hematoma formation, itching due to fentanyl and nausea and vomiting due to pethidine (Table 5).
4. DISCUSSION
In thisrandomized prospective comparative clinical study, although we found that the difference in time of request of the first post-surgery rescue pethidine was longer in Group A (mean 12.93h) than Group B (mean 12.26 h) the result was statistically non-significant (P = 0.159).We found also that Group A had superior postoperative analgesic effect with a statistically significant lower postoperative VAS score than Group B only at 8 h and 20 h in the first 24h (P = 0.039 and 0.005, respectively). However, there was a statistically significant difference regarding the amount of pethidine consumption, as Group A consumed less pethidine than Group B.
Also, the study done by Kampitak et al. demonstrating the pain-relieving effectiveness of combining AFCNB with FTB in TKA showed similar outcomes conceding with our study. The addition of AFCNB in FTB led to lower postoperative pain scores at 6 and 24 h in comparison to femoral triangle block Group (P < 0.001and 0.014, respectively). It also provided cutaneous anesthesia around the surgical incision site and the medial side of the knee post-TKA, while FTB alone failed to achieve this effect.10
Furthermore, in a study done by De Arzuaga et al., they used single injection nerve blocks for TKA; FNB versus FTB versus ACB with comparable results to our study. There was no significant difference regarding pain scores and morphine usage among FNB group and FTB group. Conversely, patients in the FNB group exhibited considerably less pain at rest in relation to those in the ACB group, both at the 6-hour and 24-hour marks (P = 0.02 and 0.005, respectively). Also, the opioids requirement in ACB was significantly higher at 6 h and 24 h (P = 0.001 and 0.01, respectively).11
Additionally, according to research conducted by Song et al., they compared the ultrasound-guided single injection femoral triangle block without the AFCN block versus ACBfor analgesia after TKA. The FTB group demonstrated notably reduced pain levels both at rest and while movement 12 and 24 h after TKA compared to the adductor canal group (P = 0.008 and 0.005, respectively).12
Also, our results were compatible with a study done by Bjørn et al., in which they similarly added the AFCNB to the FTB which provided superior analgesia than FTB alone with coverage of the surgical aspect.4
In our study, we found that Group B showed better ambulation evaluated by the ‘Timed Up and Go’ test (TUG) than Group A during the first 12 and 24 h. The findings were comparable to those from the study by Wang et al., which compared the ACB with the FTB in the TKA. In that study, the ACB group demonstrated greater quadriceps strength than the FTB group at 4, 8, and 24 h postoperatively(P<0.05). However, they stated that ACB provided more effective analgesia than FTB group (P = 0.013).2
Opposite to our study, Jæger et al. concluded in their comparative study between the ACB versus FNB for analgesia after TKA that ACB provided similar analgesia and morphine consumption in comparison to femoral nerve block but with more quadriceps muscle power preservation.13 Additionally, Li et al. concluded in their study on the analgesic efficacy and their effect on the quadriceps strength of ACB versus FNB following TKA that ACB group was similarly exhibited better quadriceps strength than femoral nerve block but without significant differences in pain score during rest or activity and opioid usage among the two groups.14 Also, Wang et al., concluded in their comparative study between ACB and FTB impact on postoperative pain following TKA that ACB provided more effective analgesia and quadriceps strength than FTB alone during the first 24 h (P = 0.013 and 0.001 respectively).2
Incidentally, the duration of spinal anesthesia in our study was shorter in Group A than Group B and this difference being statistically significant (P = 0.008). On the other hand, while the duration of surgery was also shorter in Group A than Group B, yet this difference was not statistically significant (P = 0.143)
Finally, our study blocks were safe regarding the occurrence of postoperative complications and adverse effects as hematoma, itching due to fentanyl, nausea and vomiting due to pethidine where there was an overall lower incidence of each without significant difference between both groups.
5. LIMITATIONS
First, it was a single-center study, and additional research is necessary to determine whether our findings from a single center can be generalized. Second, surgeons were not the same in all cases with variable skills and speed. Third, we did not implement a multimodal approach to pain management, which may have resulted in inadequate analgesia. Finally, all preoperative block procedures were conducted by an experienced anaesthetist who knew about the study groups, which may have introduced bias in the execution of the blocks and interpretation of the results.
6. CONCLUSION
Ultrasound guided anterior femoral cutaneous nerve block in combination with femoral triangle block may be a valid alternative to ultrasound guided adductor canal block as the regional analgesic technique within a multimodal pain management regimen for total knee arthroplasty patients. Combination of anterior femoral cutaneous nerve block and femoral triangle block provide superior analgesia and pethidine sparing effects when compared to adductor canal block. However, adductor canal block provided better preservation of motor function and allowed early ambulation.
7. Data availability
The numerical data generated during this research is available with the authors.
8. Funding
We gratefully thank Faculty of Medicine, Ain Shams University, Cairo, Egypt for providing us an opportunity to complete this research..
9. Conflict of interest
The authors did not disclose any possible conflicts of interest.
10. Authors’ contribution
MH: Conduct of the study work.
GF: Manuscript editing.
SS, SA: Literature search.
AM: Statistical analysis and review.
11. REFERENCES
- Li JW, Ma YS, Xiao LK. Postoperative pain management in total knee arthroplasty. Orthop Surg. 2019;11(5):755-61. [PubMed] DOI: 1111/os.12535
- Wang CG, Ding YL, Wang YY, Liu JY, Zhang Q. Comparison of adductor canal block and femoral triangle block for total knee arthroplasty. Clin J Pain. 2020;36(7):558-61. [PubMed] DOI: 1097/AJP.0000000000000833
- Danninger T, Opperer M, Memtsoudis SG. Perioperative pain control after total knee arthroplasty: an evidence-based review of the role of peripheral nerve blocks. World J Orthop. 2014;5(3):225-32. [PubMed] DOI: 5312/wjo.v5.i3.225
- Bjørn S, Nielsen TD, Moriggl B, Hoermann R, Bendtsen TF. Anesthesia of the anterior femoral cutaneous nerves for total knee arthroplasty incision: randomized volunteer trial. Reg Anesth Pain Med. 2019;44(12):1-7. [PubMed] DOI: 1136/rapm-2019-100904
- Manickam B, Perlas A, Duggan E, Brull R, Chan VW, Ramlogan R. Feasibility and efficacy of ultrasound-guided block of the saphenous nerve in the adductor canal. Reg Anesth Pain Med. 2009;34(6):578-80. [PubMed] DOI: 1097/aap.0b013e3181bfbf84
- Abdallah FW, Mejia J, Prasad GA, Moga R, Chahal J, Theodoropulos J, et al. Opioid- and motor-sparing with proximal, mid-, and distal locations for adductor canal block in anterior cruciate ligament reconstruction: a randomized clinical trial. Anesthesiology. 2019;131(3):619-29. [PubMed] DOI: 1097/ALN.0000000000002817
- Sogbein OA, Sondekoppam RV, Bryant D, Johnston DF, Vasarhelyi EM, MacDonald S, et al. Ultrasound-guided motor-sparing knee blocks for postoperative analgesia following total knee arthroplasty: a randomized blinded study. J Bone Joint Surg Am. 2017;99(15):1274-81. [PubMed] DOI: 2106/JBJS.16.01266
- Johnston DF, Sondekoppam RV, Uppal V, Howard JL, Ganapathy S. Hybrid blocks for total knee arthroplasty: a technical description. Clin J Pain. 2018;34(3):222-30. [PubMed] DOI: 1097/AJP.0000000000000516
- Runge C, Børglum J, Jensen JM, Kobborg T, Pedersen A, Sandberg J, Bendtsen TF. The analgesic effect of obturator nerve block added to a femoral triangle block after total knee arthroplasty: a randomized controlled trial. Reg Anesth Pain Med. 2016;41(4):445-51. [PubMed] DOI: 1097/AAP.0000000000000406
- Kampitak W, Tanavalee A, Tansatit T, Ngarmukos S, Songborassamee N, Vichainarong C. The analgesic efficacy of anterior femoral cutaneous nerve block in combination with femoral triangle block in total knee arthroplasty: a randomized controlled trial. Korean J Anesthesiol. 2021;74(6):496-505. [PubMed] DOI: 4097/kja.21120
- De Arzuaga CIS, Miguel M, Biarnés A, García M, Naya J, Khoudeir A, et al. Single-injection nerve blocks for total knee arthroplasty: femoral nerve block versus femoral triangle block versus adductor canal block—a randomized controlled double-blinded trial. Arch Orthop Trauma Surg. 2023;143(11):6763-71. [PubMed] DOI: 1007/s00402-023-04960-5
- Song L, Li Y, Xu Z, Geng ZY, Wang DX. Comparison of the ultrasound-guided single-injection femoral triangle block versus adductor canal block for analgesia following total knee arthroplasty: a randomized, double-blind trial. J Anesth. 2020;34(5):702-11. [PubMed] DOI: 1007/s00540-020-02813-8
- Jæger P, Zaric D, Fomsgaard JS, Hilsted KL, Bjerregaard J, Gyrn J, et al. Adductor canal block versus femoral nerve block for analgesia after total knee arthroplasty: a randomized, double-blind study. Reg Anesth Pain Med. 2013;38(6):526-32. [PubMed] DOI: 1097/AAP.0000000000000015
- Li D, Ma GG. Analgesic efficacy and quadriceps strength of adductor canal block versus femoral nerve block following total knee arthroplasty. Knee Surg Sports Traumatol Arthrosc. 2016;24(8):2614-9. [PubMed] DOI: 1007/s00167-015-3874-3