Wesameldin A. Sultan 1, Ahmed Abdelraouf Metwally 2, Hadeer G. Shiha 3, Amany Saeed 4
Author affiliations:
Background: Recruitment maneuvers are standard practice for mitigating aeration disturbances. The literature has described a variety of recruitment techniques. In order to evaluate the efficacy of various lung recruitment maneuvers on the incidence of atelectasis in adults undergoing laparoscopic cholecystectomy surgery with lung ultrasound, the present trail was conducted.
Methodology: A randomized controlled trial was conducted on 93 patients, divided equally into three groups: Control group: The parameters were maintained throughout the procedure without any modifications. Sustained inflation group: After abdominal deflation, sustained inflation was applied by adjusting the APL valve to 40 cmH2O on spontaneous mode and holding the bag for 30 sec. Stepwise PEEP increasing group: The PEEP was gradually increased by 2 cmH2O every 5 breathing cycles until it reached 12 cmH2O, and it was maintained until extubation, with a maximum airway pressure of 40 cmH2O.
Results: There was a statistically significant increase in the incidence of atelectasis after abdominal deflation with significantly reduced after application of recruitment maneuver. The sustained inflation group showed more significant improvement than the stepwise PEEP increasing group.
Conclusion: lung recruitment maneuvers can reduce the incidence of atelectasis in adults undergoing laparoscopic cholecystectomy surgery. The sustained inflation group was associated with better results.
Keywords: Atelectasis; Cholecystectomy; Laparoscopic; Recruitment Maneuver
Citation: Sultan WA, Metwally AA, Shiha HG, Saeed A. Effect of lung recruitment on atelectasis in lung-healthy patients undergoing laparoscopic cholecystectomy. Anaesth. pain intensive care 2025;29(2):202-209. DOI: 10.35975/apic.v29i2.2704
Received: October 16, 2024; Reviewed: October 26, 2024; Accepted: December 25, 2024
Atelectasis is one of the most prevalent postoperative pulmonary complications (PPCs) of general anesthesia, which can be occurred in all types of surgery and patients of all ages.1
Pneumoperitoneum during laparoscopic surgery exacerbates atelectasis in the perioperative period.2,3 Consequently, anesthesiologists face a significant challenge in preventing atelectasis during the perioperative period.4
Recent research indicates that the lung recruitment maneuver (LRM) can effectively reduce postoperative atelectasis in adults.5 There are numerous approaches to LRM, such as sustained inflation (SI), stepwise LRM through incremental PEEP, and postural LRM. However, the optimal method and recruitment pressure remain uncertain.6
Lung ultrasound (LUS) is a straightforward imaging technique that can be performed at the patient's bedside. For the clinical diagnosis of atelectasis, it is the gold standard. particularly in situations where mobility is restricted.7,8
Postoperative atelectasis varies among different studies, and there is no consensus on whether it is worth promoting.9
1.1. Objectives of the study
The primary outcome of this trial was the incidence of postoperative atelectasis in patients who underwent laparoscopic cholecystectomy following the application of various LRM techniques. Oxygen saturation, LUS score, and incidence of complications were the secondary outcomes.
After receiving ethical approval from the Menoufia University Research Committee under IRB number (7/2023ANET14), this prospective, controlled, double-blind, randomized trial, was conducted. It was prospectively registered in the Clinical Trials.gov ID (NCT06221449) and performed as per the principles of the Helsinki Declaration. Each participant provided written informed consent. Adult patients of either sex who were scheduled for laparoscopic cholecystectomy under general anesthesia at Menoufia University Hospitals, Menoufia Governorate, Egypt, between June 2023 and December 2023 were included in the current study.
Eligible patients for the trial were those with a body mass index (BMI) of 30 kg/m2 or less, ASA grades I-II, and the 18 to 65 y old. A comprehensive systemic examination and preoperative work-up was conducted on all patients. Patients who were pregnant, had mild respiratory tract infections, had undergone previous thoracic procedures, smokers, or were unwilling to participate in the trial, were excluded. Additionally, patients who had preoperative ultrasound evidence of pulmonary atelectasis with LUS > zero, and patients who underwent a conversion from laparoscopic to open surgery were excluded.
Data was collected by a blinded operator, and the patients were unaware of the procedure. The patients were randomly assigned to one of three groups using a closed envelope technique. The envelopes were sequentially numbered and opaque, and they were opened by an anesthesiologist who was not involved in the study.
2.1. Lung ultrasound technique
USG was conducted by a high frequency linear probe (FUJIFILM SonoSite M-Turbo TM 6-13 MHz, Bothell, WA, USA). Each hemithorax was divided into 6 quadrants: anterior, lateral, and posterior zones which were separated by the anterior and posterior axillary lines. The probe was positioned upright to the costal space, while in the posterior regions, it was positioned parallel to the intercostal space.
An independent investigator assessed the LUS score and ranked it on a four-point scale. The scoring ranges from 0 to 3, as follows:
The standard general anesthetic protocol was implemented to all patients. This consisted of ECG, NIBP, and oximetry standard monitoring, followed by mask ventilation with 0.5 FiO2 at 5 L/min for 3 min. General anesthesia was induced by intravenous fentanyl 2 µg/kg, propofol 2 mg/kg, and rocuronium 0.6 mg/kg, then a cuffed endotracheal tube of appropriate size was used to secure the airway. The neuromuscular blockade was monitored by acceleromyograph using train of four ratio (TOF-R). The anesthesia was maintained by administering 1 MAC of isoflurane in 50% oxygen and air, with intravenous rocuronium at a dose of 0.1 to 0.2 mg/kg, if necessary, in the event of prolonged surgery.
The parameters of volume-controlled mechanical ventilation after intubation were; tidal volume 6 mL/kg of ideal body weight, PEEP 6 cmH2O, FiO2 0.5, respiratory rate 12/min, and I.E. ratio 1:2. The ventilator was configured to maintain an end-tidal carbon dioxide pressure of 35 to 40 mmHg. Intra-abdominal insufflation was initiated using a CO2 insufflator, with an intra-abdominal pressure of 10-12 mmHg. Throughout the procedure, the patients were maintained in the anti-trendelenburg position with the right side facing upwards at a 30° angle. After deflation of the abdomen with neutral supine position, patients were divided into three groups as follow:
Control group: Maintain the parameters throughout the procedure without any modifications.
Sustained inflation group (SI): After abdominal deflation, the APL valve was adjusted to 40 cmH2O in spontaneous mode and the bag was held for 30 sec to achieve sustained inflation.
Stepwise PEEP: Stepwise PEEP was applied after abdominal deflation and increased by 2 cmH2O every 5 breathing cycles until it reached 12 cmH2O. This pressure was maintained until extubation, with a maximum airway pressure of 40 cmH2O.
The patient was extubated after meeting the global and respiratory criteria for extubation with TOF ratio of ≥ 0.9, following the reversal of the residual neuromuscular block with sugammadex (2 mg/kg) at the conclusion of the surgery. The patient was subsequently transferred to the PACU.
LUS was recorded at 3 definite times:
A review of prior literature was employed to estimate the sample size.4 The minimum sample size, which is 28 participants per group, is determined using statistics and sample size pro. To prevent a 10% dropout rate, the sample size is increased to 31 participants. Consequently, the total sample size is 93 participants, which are divided into three groups. The study's confidence level is 95%, and its power factor is 80%.
2.3. Statistical analysis
The IBM SPSS 26 software package was employed to conduct statistical analysis of the data under the Windows 8.1 operating system. Numbers and percentages were employed to describe qualitative data. The qualitative data was compared using the Chi-Square test (X2). The quantitative data was compared using the student's t-test. In the context of quantitative variable comparisons among more than two groups of non-normally distributed data, the Kruskal-Wallis test is a post-hoc test that is employed to determine significance. The statistical significance of three or more means (parametric quantitative data) was determined using the analysis of variance (ANOVA) test.
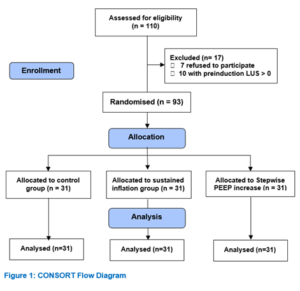
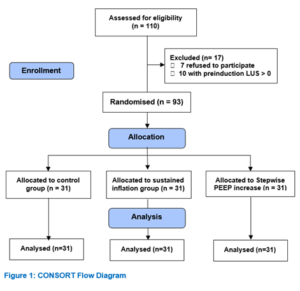
One hundred and ten patients were enrolled in this randomized controlled trial, seven patients refused to participate in the study, and ten patients were excluded as their preinduction LUS were more than zero (Figure 1). The remaining 93 patients were allocated randomly into three equal groups. All patients were included until the conclusion of the study. Demographic characteristics showed similarity with no significance among the studied groups (Table 1). The pre-induction LUS was zero for all patients in the three groups as they were screened, and any patient showed LUS > zero was excluded immediately from the study.
The mean incidence of atelectasis in all groups after abdominal deflation was 92.51 %. It was 90.42 %, 93.57 %, and 93.54 % in control group, SI group, and Stepwise PEEP group respectively (Table 2).
LUS was assessed postoperatively after application of recruitment maneuver and it showed statistically significant improvement of atelectasis in SI group and Stepwise PEEP compared to the control group and the atelectasis incidence was 9.7 %, 16.12 %, and 90.34 %, respectively with p value of 0.004. Moreover, we found that the recruitment maneuver by sustained inflation showed significant improvement of atelectasis compared to Stepwise PEEP group with p1 value of 0.042 (Table 3).
Oxygen saturation showed no significant differences throughout the procedure in all recorded time (Table 4).There was non-significant difference among the studied groups as regard to complications incidence of recruitment maneuver. One patient in SI group developed bradycardia and one patient in Stepwise PEEP as well. In addition to 4 patients in SI group and 2 patients in Stepwise PEEP developed hypotension. All those patients were followed and improved spontaneously without any pharmacological intervention (Table 5).
Regardless of whether intravenous or inhalational anesthetics are employed, atelectasis is observed in approximately 90% of all GA patients during both spontaneous breathing and muscle paralysis. Atelectasis is considered the main cause of postoperative pulmonary complications.11-14
The purpose of our trial was to evaluate the efficacy of various lung recruitment maneuvers on the prevalence of atelectasis in adults who underwent laparoscopic cholecystectomy surgery with the aid of lung ultrasound.
In the current study, after abdominal deflation all patients showed significant occurrence of atelectasis with mean incidence of 92.51 %. Postoperatively, there was a statistically significant difference in lung ultrasound score, after lung recruitment application in SI group and stepwise PEEP compared to control group, and we found that SI group improved significantly than stepwise PEEP group. Hedenstierna et al.15 investigated the mechanism of atelectasis that arises during the perioperative period and reported a 90 % incidence. The incidence of atelectasis in the postoperative period was also 80 %. Lee et al.2 evaluated perioperative atelectasis using various ventilation methods. The total LUS was significantly higher in T2 (4.20) and T3 (1.77) than in T1 (0.63).
Liu et al.8 investigated the impact of an ultrasound-guided lung recruitment maneuver on atelectasis during laparoscopic surgery. At the T2 and T3 periods, the control group exhibited an atelectasis incidence of 76 % and 81 %, respectively. Furthermore, they conducted lung ultrasounds 24 hours following the surgery, which resulted in a 57 % reduction in the incidence. Despite the development of atelectasis, their research indicates that it does not persist.
Based on electrical impedance tomography (EIT), Karsten et al.16 demonstrated that the combination of the RM and PEEP ensured homogeneity in the local ventilation during laparoscopic surgery and improved oxygenation and lung compliance. De Jong et al.17 observed that mechanical ventilation in conjunction with PEEP at 5–10 cmH2O was associated with a reduction in postoperative respiratory complications and a reduction in hospital stays in major abdominal surgery in a trial of 10,978 patients.
In the current trial, we applied fixed PEEP of 6 cmH2O in all studied groups throughout the operation until abdominal deflation. Then PEEP was increased gradually in stepwise PEEP group up to 12 cmH2O. It was accompanied by improved incidence of atelectasis but still inferior to SI group. It might need to be increased more to achieve comparable improvement.
The total time of surgery was not significantly different among the studied groups, which is consistent with the findings of Pang et al.13, who found no difference in operation time. Supposedly, the incidence of atelectasis will increase with prolonged operative time.
Ramezani et al.18 observed no change in oxygen saturations in all patients at various time periods, which was consistent with the non-significant difference among our studied groups in all recorded time. Pang et al.13 discovered that intraoperative oxygenation was enhanced following CO2 pneumoperitoneum during laparoscopic cholecystectomy through the implementation of an alveolar recruitment strategy (ARS). Conversely, this variation in oxygenation in comparison to the control group did not persist in the postoperative period. These findings agree with those of comparable investigations.19,20
In the Stepwise PEEP increasing group, one patient developed bradycardia (3.22 %) and two patients experienced hypotension (6.45 %) while, in the SI group, one patient exhibited bradycardia (3.22 %) and four patients experienced hypotension (12.9 %). Conversely, Cylwik and Buda4, did not observe any significant clinical complications resulting from alveolar recruitment.
In the literature that is currently available, there are reports that do not confirm the efficacy of recruitment maneuvers in the context of reducing the risk of postoperative complications21,22. However, these studies were not conducted using ultrasound monitoring.
In this study, we used LUS successfully to assess the degree of atelectasis intraoperatively. In another trial done by Monastesse et al.,23 concluded that LUS facilitates tracking and diagnosis of atelectasis and other respiratory complications. Wu et al.,9 and Park et al.5 emphasized the usefulness of using LUS in diagnosis and prognosis of perioperative respiratory complications.
Initially, we enrolled healthy patients who were undergoing relatively short procedures and possessed a normal lung function. Consequently, the generalizability of our findings is restricted to healthy patients necessitating additional research in high-risk patients or in high-risk surgical settings.
The second limitation is that the practical application of lung ultrasound-guided recruitment maneuvers may be restricted due to the difficulty of applying the ultrasound probe to the posterior region of the body, particularly during surgery.
Third, the trial was conducted at a single center and involved a brief procedure, consequently, prolonged procedures may be linked to varying outcomes.
Lung recruitment maneuver can reduce the incidence of atelectasis in adults undergoing laparoscopic cholecystectomy surgery. In comparison to the Stepwise PEEP group, the recruitment maneuver by SI demonstrated significant improvements in atelectasis. Additional research is necessary to establish the function of ultrasound-guided recruitment maneuvers in different surgical environments.
7. Data availability
The numerical data is available with the authors, and can be provided on a reasonable request upon request.
8. Conflict of interest
There was no conflict of interest among all of the authors.
9. Funding
The trial used the institutional resources only, and no industry or sponsor funding was availed in the conduct of this study.
10. Authors contribution
WS: concept, manuscript editing, corresponding, approval,
AA: manuscript editing, approval,
HS, AS: clinical conduction, preparation of manuscript,
Author affiliations:
- Wesameldin A. Sultan, Assistant Professor, Department of Anesthesia & Intensive Care, Faculty of Medicine, Menoufia University, Menoufia, Egypt; Email: wesamsultan@med.menofia.edu.eg
- Ahmed Abdelraouf Metwally, Professor, Department of Anesthesia & Intensive Care, Faculty of Medicine, Menoufia University, Menoufia, Egypt; Email: drahmedabdelraouf@med.menofia.edu.eg
- Hadeer G. Shiha, Demonstrator, Department of Anesthesia & Intensive Care, Faculty of Medicine, Menoufia University, Menoufia, Egypt; Email: hadeer101287@gmail.com
- Amany Saeed, Lecturer, Department of Anesthesia & Intensive Care, Faculty of Medicine, Menoufia University, Menoufia, Egypt; Email: amany.saeed.12@med.menofia.edu.eg
ABSTRACT
Background: Recruitment maneuvers are standard practice for mitigating aeration disturbances. The literature has described a variety of recruitment techniques. In order to evaluate the efficacy of various lung recruitment maneuvers on the incidence of atelectasis in adults undergoing laparoscopic cholecystectomy surgery with lung ultrasound, the present trail was conducted.
Methodology: A randomized controlled trial was conducted on 93 patients, divided equally into three groups: Control group: The parameters were maintained throughout the procedure without any modifications. Sustained inflation group: After abdominal deflation, sustained inflation was applied by adjusting the APL valve to 40 cmH2O on spontaneous mode and holding the bag for 30 sec. Stepwise PEEP increasing group: The PEEP was gradually increased by 2 cmH2O every 5 breathing cycles until it reached 12 cmH2O, and it was maintained until extubation, with a maximum airway pressure of 40 cmH2O.
Results: There was a statistically significant increase in the incidence of atelectasis after abdominal deflation with significantly reduced after application of recruitment maneuver. The sustained inflation group showed more significant improvement than the stepwise PEEP increasing group.
Conclusion: lung recruitment maneuvers can reduce the incidence of atelectasis in adults undergoing laparoscopic cholecystectomy surgery. The sustained inflation group was associated with better results.
Keywords: Atelectasis; Cholecystectomy; Laparoscopic; Recruitment Maneuver
Citation: Sultan WA, Metwally AA, Shiha HG, Saeed A. Effect of lung recruitment on atelectasis in lung-healthy patients undergoing laparoscopic cholecystectomy. Anaesth. pain intensive care 2025;29(2):202-209. DOI: 10.35975/apic.v29i2.2704
Received: October 16, 2024; Reviewed: October 26, 2024; Accepted: December 25, 2024
1. INTRODUCTION
Atelectasis is one of the most prevalent postoperative pulmonary complications (PPCs) of general anesthesia, which can be occurred in all types of surgery and patients of all ages.1
Pneumoperitoneum during laparoscopic surgery exacerbates atelectasis in the perioperative period.2,3 Consequently, anesthesiologists face a significant challenge in preventing atelectasis during the perioperative period.4
Recent research indicates that the lung recruitment maneuver (LRM) can effectively reduce postoperative atelectasis in adults.5 There are numerous approaches to LRM, such as sustained inflation (SI), stepwise LRM through incremental PEEP, and postural LRM. However, the optimal method and recruitment pressure remain uncertain.6
Lung ultrasound (LUS) is a straightforward imaging technique that can be performed at the patient's bedside. For the clinical diagnosis of atelectasis, it is the gold standard. particularly in situations where mobility is restricted.7,8
Postoperative atelectasis varies among different studies, and there is no consensus on whether it is worth promoting.9
1.1. Objectives of the study
The primary outcome of this trial was the incidence of postoperative atelectasis in patients who underwent laparoscopic cholecystectomy following the application of various LRM techniques. Oxygen saturation, LUS score, and incidence of complications were the secondary outcomes.
2. METHODOLOGY
After receiving ethical approval from the Menoufia University Research Committee under IRB number (7/2023ANET14), this prospective, controlled, double-blind, randomized trial, was conducted. It was prospectively registered in the Clinical Trials.gov ID (NCT06221449) and performed as per the principles of the Helsinki Declaration. Each participant provided written informed consent. Adult patients of either sex who were scheduled for laparoscopic cholecystectomy under general anesthesia at Menoufia University Hospitals, Menoufia Governorate, Egypt, between June 2023 and December 2023 were included in the current study.
Eligible patients for the trial were those with a body mass index (BMI) of 30 kg/m2 or less, ASA grades I-II, and the 18 to 65 y old. A comprehensive systemic examination and preoperative work-up was conducted on all patients. Patients who were pregnant, had mild respiratory tract infections, had undergone previous thoracic procedures, smokers, or were unwilling to participate in the trial, were excluded. Additionally, patients who had preoperative ultrasound evidence of pulmonary atelectasis with LUS > zero, and patients who underwent a conversion from laparoscopic to open surgery were excluded.
Data was collected by a blinded operator, and the patients were unaware of the procedure. The patients were randomly assigned to one of three groups using a closed envelope technique. The envelopes were sequentially numbered and opaque, and they were opened by an anesthesiologist who was not involved in the study.
2.1. Lung ultrasound technique
USG was conducted by a high frequency linear probe (FUJIFILM SonoSite M-Turbo TM 6-13 MHz, Bothell, WA, USA). Each hemithorax was divided into 6 quadrants: anterior, lateral, and posterior zones which were separated by the anterior and posterior axillary lines. The probe was positioned upright to the costal space, while in the posterior regions, it was positioned parallel to the intercostal space.
An independent investigator assessed the LUS score and ranked it on a four-point scale. The scoring ranges from 0 to 3, as follows:
- = Normal aeration
- = Mild loss of aeration. (≥ 3 B lines)
- = Moderate loss of aeration. (Multiple coalescent B lines)
- = Severe loss of aeration. (Consolidation)
The standard general anesthetic protocol was implemented to all patients. This consisted of ECG, NIBP, and oximetry standard monitoring, followed by mask ventilation with 0.5 FiO2 at 5 L/min for 3 min. General anesthesia was induced by intravenous fentanyl 2 µg/kg, propofol 2 mg/kg, and rocuronium 0.6 mg/kg, then a cuffed endotracheal tube of appropriate size was used to secure the airway. The neuromuscular blockade was monitored by acceleromyograph using train of four ratio (TOF-R). The anesthesia was maintained by administering 1 MAC of isoflurane in 50% oxygen and air, with intravenous rocuronium at a dose of 0.1 to 0.2 mg/kg, if necessary, in the event of prolonged surgery.
The parameters of volume-controlled mechanical ventilation after intubation were; tidal volume 6 mL/kg of ideal body weight, PEEP 6 cmH2O, FiO2 0.5, respiratory rate 12/min, and I.E. ratio 1:2. The ventilator was configured to maintain an end-tidal carbon dioxide pressure of 35 to 40 mmHg. Intra-abdominal insufflation was initiated using a CO2 insufflator, with an intra-abdominal pressure of 10-12 mmHg. Throughout the procedure, the patients were maintained in the anti-trendelenburg position with the right side facing upwards at a 30° angle. After deflation of the abdomen with neutral supine position, patients were divided into three groups as follow:
Control group: Maintain the parameters throughout the procedure without any modifications.
Sustained inflation group (SI): After abdominal deflation, the APL valve was adjusted to 40 cmH2O in spontaneous mode and the bag was held for 30 sec to achieve sustained inflation.
Stepwise PEEP: Stepwise PEEP was applied after abdominal deflation and increased by 2 cmH2O every 5 breathing cycles until it reached 12 cmH2O. This pressure was maintained until extubation, with a maximum airway pressure of 40 cmH2O.
The patient was extubated after meeting the global and respiratory criteria for extubation with TOF ratio of ≥ 0.9, following the reversal of the residual neuromuscular block with sugammadex (2 mg/kg) at the conclusion of the surgery. The patient was subsequently transferred to the PACU.
LUS was recorded at 3 definite times:
- T1: Pre induction
- T2: After abdominal deflation
- T3: Postoperative after 20 min in PACU
A review of prior literature was employed to estimate the sample size.4 The minimum sample size, which is 28 participants per group, is determined using statistics and sample size pro. To prevent a 10% dropout rate, the sample size is increased to 31 participants. Consequently, the total sample size is 93 participants, which are divided into three groups. The study's confidence level is 95%, and its power factor is 80%.
2.3. Statistical analysis
The IBM SPSS 26 software package was employed to conduct statistical analysis of the data under the Windows 8.1 operating system. Numbers and percentages were employed to describe qualitative data. The qualitative data was compared using the Chi-Square test (X2). The quantitative data was compared using the student's t-test. In the context of quantitative variable comparisons among more than two groups of non-normally distributed data, the Kruskal-Wallis test is a post-hoc test that is employed to determine significance. The statistical significance of three or more means (parametric quantitative data) was determined using the analysis of variance (ANOVA) test.
3. RESULTS
One hundred and ten patients were enrolled in this randomized controlled trial, seven patients refused to participate in the study, and ten patients were excluded as their preinduction LUS were more than zero (Figure 1). The remaining 93 patients were allocated randomly into three equal groups. All patients were included until the conclusion of the study. Demographic characteristics showed similarity with no significance among the studied groups (Table 1). The pre-induction LUS was zero for all patients in the three groups as they were screened, and any patient showed LUS > zero was excluded immediately from the study.
| Table 1: Demographic Data | |||||
| Variable
|
Groups | Chi-Square | |||
| Control group | Sustained inflation group | Stepwise PEEP increasing | X2 | P | |
| Gender [n (%)] | |||||
| Male | 15 (48.38) | 16 (51.61) | 12 (38.70) | 1.6 | 0.449 |
| Female | 16 (51.61) | 15 (48.38) | 19 (61.29) | ||
| Age (y) | 36.67 ± 7.840 | 38.51 ± 7.003 | 43.51 ± 4.043 | 0.007 | 0.996 |
| BMI (kg/m2) | 25.45 ± 2.52 | 23.06 ± 2.12 | 24.93 ± 2.11 | 0.145 | 0.836 |
| Total time of surgery (min) | 50.51 ± 6.08 | 54.38 ± 5.69 | 52.54 ± 6.11 | 0.086 | 0.742 |
| Total anesthetic time (min) | 66.51 ± 12.0 | 68.83 ± 12.0 | 64.77 ± 12.0 | 0.258 | 0.524 |
| Recovery Time (min) | 15.38 ± 6.0 | 14.19 ± 6.0 | 14.93 ± 6 | 0.147 | 0.832 |
| Data presented as n (%) or Mean ± SD; P < 0.05 considered as significant | |||||
| Table 2: Lung ultrasound Score distribution of the studied subjects after abdominal deflation | |||||
| Lung ultrasound Score | Groups | Chi-Square | |||
| Control group | Sustained inflation group | Stepwise PEEP increasing | X2 | P | |
| 0 | 3 (9.7) | 2 (6.45) | 2 (6.45) | 3.142 | 0.153 |
| 1 | 23 (74.2) | 26 (83.87) | 25 (80.64) | ||
| 2 | 5 (16.22) | 3 (9.7) | 4 (12.9) | ||
| 3 | 0 (0) | 0 (0) | 0 (0) | ||
| (1-2) | 90.42% | 93.57% | 93.54% | 2.953 | 0.052 |
| Data presented as n (%); Incidence of atelectasis: LUS ˃ 0, χ2: Chi-squared test; P < 0.05 is significant | |||||
| Table 3: Lung ultrasound Scores in the studied subjects post-operation | ||||||
| Lung ultrasound
Score |
Control group | Sustained inflation
group |
Stepwise PEEP
increasing group |
Chi-Square | ||
| X2 | P | P1 | ||||
| 0 | 3 (9.7) | 28 (90.32) | 26 (83.87) | 3.147 | 0.057 | |
| 1 | 25 (80.64) | 3 (9.7) | 4 (12.9) | |||
| 2 | 3 (9.7) | 0 (0) | 1 (3.22) | |||
| 3 | 0 (0) | 0 (0) | 0 (0) | |||
| (1-2) | 90.34% | 9.7% | 16.12% | 1.631 | 0.004* | 0.042* |
| P= between three groups control group, sustained inflation group & stepwise PEEP increasing group.
P1= between Sustained inflation group and Stepwise PEEP increasing. χ2: Chi-squared test, Incidence of atelectasis: LUS>0, *significant; Data presented as n (%) |
||||||
| Table 4: Oxygen Saturation of the studied patients | |||||
| Time | Control group | Sustained inflation group | Stepwise PEEP group | t | p |
| Baseline before induction | 94.87 ± 2.24 | 95.32 ± 2.15 | 94.74 ± 4.42 | 0.021 | 0.999 |
| 10 min after induction | 95.48 ± 2.68 | 95.16 ± 5.67 | 94.96 ± 2.15 | 0.073 | 0.984 |
| 10 min after abdominal insufflation | 96.12 ± 4.89 | 95.83 ± 4.46 | 96.29 ± 3.75 | 0.158 | 0.972 |
| 20 min intraoperative | 95.64 ± 4.94 | 94.70 ± 5.74 | 95.09 ± 2.13 | 0.136 | 0.992 |
| 30 min intraoperative | 94.61 ± 4.21 | 94.77 ± 3.42 | 94.70 ± 2.14 | 0.213 | 0.999 |
| 10 min after abdominal deflation | 95.70 ± 4.36 | 95.09 ± 4.25 | 95.35 ± 4.74 | 0.201 | 0.999 |
| 10 min after recruitment | 95.70 ± 4.66 | 98.32 ± 2.56 | 98.29 ± 5.35 | 0.331 | 0.987 |
| 10 min after extubation | 93.77 ± 6.73 | 95.64 ± 2.78 | 95.19 ± 3.15 | 0.025 | 0.988 |
| In PACU | 95.70 ± 3.14 | 95.74 ± 3.84 | 95.25 ± 7.34 | 0.235 | 0.997 |
| Data presented as n (%) or Mean ± SD; P < 0.05 considered as significant; χ2: Chi-squared test | |||||
| Table 5: Complication after recruitment of the studied subjects: | |||||
| Parameter | Control group | Sustained inflation
group |
Stepwise PEEP
increasing group |
X2 | FE p |
| Bradycardia | 0 (0) | 1 (3.22) | 1 (3.22) | 2.35 |
0.054 |
| Hypotension | 0 (0) | 4 (12.90) | 2 (6.45) | ||
| χ2: Chi-squared test; Data presented as n (%) | |||||
The mean incidence of atelectasis in all groups after abdominal deflation was 92.51 %. It was 90.42 %, 93.57 %, and 93.54 % in control group, SI group, and Stepwise PEEP group respectively (Table 2).
LUS was assessed postoperatively after application of recruitment maneuver and it showed statistically significant improvement of atelectasis in SI group and Stepwise PEEP compared to the control group and the atelectasis incidence was 9.7 %, 16.12 %, and 90.34 %, respectively with p value of 0.004. Moreover, we found that the recruitment maneuver by sustained inflation showed significant improvement of atelectasis compared to Stepwise PEEP group with p1 value of 0.042 (Table 3).
Oxygen saturation showed no significant differences throughout the procedure in all recorded time (Table 4).There was non-significant difference among the studied groups as regard to complications incidence of recruitment maneuver. One patient in SI group developed bradycardia and one patient in Stepwise PEEP as well. In addition to 4 patients in SI group and 2 patients in Stepwise PEEP developed hypotension. All those patients were followed and improved spontaneously without any pharmacological intervention (Table 5).
4. DISCUSSION
Regardless of whether intravenous or inhalational anesthetics are employed, atelectasis is observed in approximately 90% of all GA patients during both spontaneous breathing and muscle paralysis. Atelectasis is considered the main cause of postoperative pulmonary complications.11-14
The purpose of our trial was to evaluate the efficacy of various lung recruitment maneuvers on the prevalence of atelectasis in adults who underwent laparoscopic cholecystectomy surgery with the aid of lung ultrasound.
In the current study, after abdominal deflation all patients showed significant occurrence of atelectasis with mean incidence of 92.51 %. Postoperatively, there was a statistically significant difference in lung ultrasound score, after lung recruitment application in SI group and stepwise PEEP compared to control group, and we found that SI group improved significantly than stepwise PEEP group. Hedenstierna et al.15 investigated the mechanism of atelectasis that arises during the perioperative period and reported a 90 % incidence. The incidence of atelectasis in the postoperative period was also 80 %. Lee et al.2 evaluated perioperative atelectasis using various ventilation methods. The total LUS was significantly higher in T2 (4.20) and T3 (1.77) than in T1 (0.63).
Liu et al.8 investigated the impact of an ultrasound-guided lung recruitment maneuver on atelectasis during laparoscopic surgery. At the T2 and T3 periods, the control group exhibited an atelectasis incidence of 76 % and 81 %, respectively. Furthermore, they conducted lung ultrasounds 24 hours following the surgery, which resulted in a 57 % reduction in the incidence. Despite the development of atelectasis, their research indicates that it does not persist.
Based on electrical impedance tomography (EIT), Karsten et al.16 demonstrated that the combination of the RM and PEEP ensured homogeneity in the local ventilation during laparoscopic surgery and improved oxygenation and lung compliance. De Jong et al.17 observed that mechanical ventilation in conjunction with PEEP at 5–10 cmH2O was associated with a reduction in postoperative respiratory complications and a reduction in hospital stays in major abdominal surgery in a trial of 10,978 patients.
In the current trial, we applied fixed PEEP of 6 cmH2O in all studied groups throughout the operation until abdominal deflation. Then PEEP was increased gradually in stepwise PEEP group up to 12 cmH2O. It was accompanied by improved incidence of atelectasis but still inferior to SI group. It might need to be increased more to achieve comparable improvement.
The total time of surgery was not significantly different among the studied groups, which is consistent with the findings of Pang et al.13, who found no difference in operation time. Supposedly, the incidence of atelectasis will increase with prolonged operative time.
Ramezani et al.18 observed no change in oxygen saturations in all patients at various time periods, which was consistent with the non-significant difference among our studied groups in all recorded time. Pang et al.13 discovered that intraoperative oxygenation was enhanced following CO2 pneumoperitoneum during laparoscopic cholecystectomy through the implementation of an alveolar recruitment strategy (ARS). Conversely, this variation in oxygenation in comparison to the control group did not persist in the postoperative period. These findings agree with those of comparable investigations.19,20
In the Stepwise PEEP increasing group, one patient developed bradycardia (3.22 %) and two patients experienced hypotension (6.45 %) while, in the SI group, one patient exhibited bradycardia (3.22 %) and four patients experienced hypotension (12.9 %). Conversely, Cylwik and Buda4, did not observe any significant clinical complications resulting from alveolar recruitment.
In the literature that is currently available, there are reports that do not confirm the efficacy of recruitment maneuvers in the context of reducing the risk of postoperative complications21,22. However, these studies were not conducted using ultrasound monitoring.
In this study, we used LUS successfully to assess the degree of atelectasis intraoperatively. In another trial done by Monastesse et al.,23 concluded that LUS facilitates tracking and diagnosis of atelectasis and other respiratory complications. Wu et al.,9 and Park et al.5 emphasized the usefulness of using LUS in diagnosis and prognosis of perioperative respiratory complications.
5. LIMITATIONS
Initially, we enrolled healthy patients who were undergoing relatively short procedures and possessed a normal lung function. Consequently, the generalizability of our findings is restricted to healthy patients necessitating additional research in high-risk patients or in high-risk surgical settings.
The second limitation is that the practical application of lung ultrasound-guided recruitment maneuvers may be restricted due to the difficulty of applying the ultrasound probe to the posterior region of the body, particularly during surgery.
Third, the trial was conducted at a single center and involved a brief procedure, consequently, prolonged procedures may be linked to varying outcomes.
6. CONCLUSION
Lung recruitment maneuver can reduce the incidence of atelectasis in adults undergoing laparoscopic cholecystectomy surgery. In comparison to the Stepwise PEEP group, the recruitment maneuver by SI demonstrated significant improvements in atelectasis. Additional research is necessary to establish the function of ultrasound-guided recruitment maneuvers in different surgical environments.
7. Data availability
The numerical data is available with the authors, and can be provided on a reasonable request upon request.
8. Conflict of interest
There was no conflict of interest among all of the authors.
9. Funding
The trial used the institutional resources only, and no industry or sponsor funding was availed in the conduct of this study.
10. Authors contribution
WS: concept, manuscript editing, corresponding, approval,
AA: manuscript editing, approval,
HS, AS: clinical conduction, preparation of manuscript,
11. REFERENCES
- Généreux V, Chassé M, Girard F, Massicotte N, Chartrand-Lefebvre C, Girard M. Effects of positive end-expiratory pressure/recruitment manoeuvres compared with zero end-expiratory pressure on atelectasis during open gynaecological surgery as assessed by ultrasonography: a randomised controlled trial. Br J Anaesth. 2020;124(1):101-9. [PubMed] DOI: 1016/j.bja.2019.09.040
- Lee JH, Choi S, Ji SH, Jang YE, Kim EH, Kim HS, et al. Effect of an ultrasound-guided lung recruitment manoeuvre on postoperative atelectasis in children: a randomised controlled trial. Eur J Anaesthesiol. 2020;37(8):719-27. [PubMed] DOI: 1097/EJA.0000000000001175
- Singh N, Kumari B. Jaipur Award Abstracts: Airway. Indian J Anaesth. 2020;64(1):S54-S9. [PMC]
- Cylwik J, Buda N. The impact of ultrasound-guided recruitment maneuvers on the risk of postoperative pulmonary complications in patients undergoing general anesthesia. J Ultrasonogr. 2022;22(88):6-11. [PubMed] DOI: 15557/JoU.2022.0002
- Park SK, Yang H, Yoo S, Kim WH, Lim YJ, Bahk JH, et al. Ultrasound-guided versus conventional lung recruitment manoeuvres in laparoscopic gynaecological surgery: a randomised controlled trial. Eur J Anaesthesiol. 2021;38(3):275-84. [PubMed] DOI: 1097/EJA.0000000000001435
- Gattinoni L, Marini JJ, Quintel M. Recruiting the acutely injured lung: how and why? Am J Respir Crit Care Med. 2020;201(2):130-2. [PubMed] DOI: 1164/rccm.201910-2005ED
- Dhivya R, Arun Prasath D, Yachendra VSG, Surya R, Ramakrishnan L. Modified Lung Ultrasound Score to Determine the Degree of Perioperative Atelectasis in Adults Undergoing Elective Laparoscopic Surgery under General Anaesthesia-A Prospective Observational Study. J Med Chem Sci. 2023;6(9):2104-10. DOI: 26655/JMCHEMSCI.2023.9.17
- Liu Y, Wang J, Geng Y, Zhang Y, Su H, Yang Y. The effect of ultrasound-guided lung recruitment maneuvers on atelectasis in lung-healthy patients undergoing laparoscopic gynecologic surgery: a randomized controlled trial. BMC Anesthesiol. 2022;22(1):200. [PubMed] DOI: 1186/s12871-022-01742-1
- Wu L, Yang Y, Yin Y, Yang L, Sun X, Zhang J. Lung ultrasound for evaluating perioperative atelectasis and aeration in the post-anesthesia care unit. J Clin Monit Comput. 2023;37(5):1295-1302. [PubMed] DOI: 1007/s10877-023-00994-7
- Boccatonda A, Cocco G, Ianniello E, Montanari M, D'Ardes D, Borghi C, et al. One year of SARS-CoV-2 and lung ultrasound: what has been learned and future perspectives. J Ultrasound. 2021;24:115-23. [PubMed] DOI: 1007/s40477-021-00575-x
- Ball L, Costantino F, Orefice G, Chandrapatham K, Pelosi P. Intraoperative mechanical ventilation: state of the art. Minerva Anestesiol. 2017;83(10):1075-88. [PubMed] DOI: 23736/S0375-9393.17.11970-X
- Pang QY, An R, Liu HL. Effects of inhalation and intravenous anesthesia on intraoperative cardiopulmonary function and postoperative complications in patients undergoing thoracic surgery. Minerva Anestesiol. 2018;84(11):1287-97. [PubMed] DOI: 23736/S0375-9393.18.12501-6
- Pang C, Yap J, Chen P. The effect of an alveolar recruitment strategy on oxygenation during laparoscopic cholecystectomy. Anaesth Intensive Care. 2003;31(2):176-80. [PubMed] DOI: 1177/0310057X0303100206
- Kelkar KV. Post-operative pulmonary complications after non-cardiothoracic surgery. Indian J Anaesth. 2015;59(9):599-605. [PubMed] DOI: 4103/0019-5049.165857
- Hedenstierna G, Edmark L. Mechanisms of atelectasis in the perioperative period. Best Pract Res Clin Anaesthesiol. 2010;24(2):157-69. [PubMed] DOI: 1016/j.bpa.2009.12.002
- Karsten J, Luepschen H, Grossherr M, Bruch HP, Leonhardt S, Gehring H, et al. Effect of PEEP on regional ventilation during laparoscopic surgery monitored by electrical impedance tomography. Acta Anaesthesiol Scand. 2011;55(7):878-86. [PubMed] DOI: 1111/j.1399-6576.2011.02467.x
- De Jong MA, Ladha KS, Melo MFV, Staehr-Rye AK, Bittner EA, Kurth T, et al. Differential effects of intraoperative positive end expiratory pressure (PEEP) on respiratory outcome in major abdominal surgery versus craniotomy. Ann Surg. 2016;264(2):362. [PubMed] DOI: 1097/SLA.0000000000001499
- Ramezani F, Delpisheh A. Modified Lung Ultrasound Score to Determine the Degree of Perioperative Atelectasis in Adults Undergoing Elective Laparoscopic under General Anaesthesia- A Prospective Observational Study. J Med Chem Sci. 2023;6(9):2104-10.DOI: 26655/JMCHEMSCI.2023.9.17
- Rothen H, Sporre B, Engberg G, Wegenius G, Hedenstierna G. Re-expansion of atelectasis during general anaesthesia may have a prolonged effect. Acta Anaesthesiol Scand. 1995;39(1):118-25. [PubMed] DOI: 1111/j.1399-6576.1995.tb05602.x
- Clarke J, Schuitemaker M, Sleigh J. The effect of intraoperative ventilation strategies on perioperative atelectasis. Anaesth Intensive Care. 1998;26(3):262-6. [PubMed] DOI: 1177/0310057X9802600305
- Barbosa FT, Castro AA, de Sousa-Rodrigues CF. Positive end-expiratory pressure (PEEP) during anaesthesia for prevention of mortality and postoperative pulmonary complications. Cochrane Database Syst Rev. 2014;(6). [PubMed] DOI: 1002/14651858.CD007922.pub3
- Bluth T, Neto AS, Schultz MJ, Pelosi P, de Abreu MG. Effect of intraoperative high positive end-expiratory pressure (PEEP) with recruitment maneuvers vs low PEEP on postoperative pulmonary complications in obese patients: a randomized clinical trial. JAMA. 2019;321(23):2292-305. [PubMed] DOI: 1001/jama.2019.7505
- Montastesse A, Girard F, Massicotte N, Chartrand-Lefebvre C, Girard M. Lung ultrasound for the assessment of perioperative atelectasis: a pilot feasibility study. Anesth Analg. 2017;124(2):494-504. [PubMed] DOI: 1213/ANE.0000000000001603