Mahmoud Ahmed Kamel 1, Ahmed Saad Abdelmonem 2*, Gehan Muhammed Kamal 3, Ghada El Awady 4, Ahmed Mohamed Soliman 5
Author affiliation:
Background & Objectives: Dexamethasone is well known to potentiate the efficacy and the duration of local anesthetic drugs. The anesthetists have used this combination in spinal and epidural analgesia with satisfaction. We evaluated the efficacy of intravenous (IV) dexamethasone vs perineural administration in reducing postoperative pain in adults having supraclavicular brachial plexus blocks (BPB) for elective procedures involving the upper limbs.
Methodology: This prospective randomized, double blind study involved 44 patients aged 18 to 60 y, both sexes, posted for elective upper limb cancer (synovial sarcoma, liposarcoma, melanoma, squamous cell carcinoma and osteosarcoma) surgeries under supraclavicular block, with an expected tourniquet time less than 120 min. Patients were divided into two equal groups: Perineural Dexamethasone group: 2 mL of dexamethasone (8 mg) combined with 28 mL of bupivacaine 0.25% concentration perineurally, along with 2 mL of normal saline as an IV placebo and systemic dexamethasone group: normal saline 2 mL was combined with 28 mL of bupivacaine 0.25% perineurally, and dexamethasone 2 mL (8 mg) was administered IV.
Results: Onset time for sensory and motor block were significantly higher in systemic than perineural groups (P < 0.05). Duration of sensory blocks and duration of analgesia of the block were significantly lower in system than perineural groups (P < 0.05). There was significant difference between the two groups as regards the number of patients who needed a second dose of morphine (P = 0.030). Total morphine doses were significantly different between both groups. The duration of motor block was insignificantly different between both groups.
Conclusions: When compared to its IV counterpart, perineural dexamethasone offers a prolonged duration of motor block, sensory block, and postoperative analgesia in ultrasound-guided supraclavicular brachial plexus block.
Abbreviations: BPB: brachial plexus blocks, IV: intravenous, PACU: post-anesthesia care unit
Keywords: Cancer; Perineural; Intravenous; Dexamethasone; Dysarthria; Pain; Supraclavicular Plexus Nerve Block; Upper Limb Surgeries; VAS
Citation: Kamel MA, Abdelmonem AS, KamalGM, El Awady G, Soliman AM. Comparative study between perineural versus intravenous dexamethasone in prolonging the analgesic effect of supraclavicular plexus nerve block in upper limb surgeries. Anaesth. pain intensive care 2025;29(2):178-184. DOI: 10.35975/apic.v29i2.2701
Received: January 19, 2025; Reviewed: February 15, 2025; Accepted: February 15, 2025
The brachial plexus block (BPB) is a common and well-liked method of administering analgesia and peri-operative anesthesia during procedures involving the upper limbs. For surgeries that are conducted below the shoulder joint, the supraclavicular approach is the most consistent and straightforward method. Patients with multiple cardio-respiratory problems can benefit from a regional nerve block since it lowers their anxiety before surgery and allows them to utilize less anesthetic.1
Ultrasound guidance is a reliable and safe technique in peripheral nerve blocks. It also plays a crucial and an increasing role in medicine nowadays due its low cost, the absence of ionizing radiation and its high temporal resolution.2
The local anesthetics alone for supraclavicular BPB blocking ensure optimal working conditions, although the pain relief after the procedure is brief. Local anesthetics were combined with a variety of adjuvants, such as opioids, clonidine, neostigmine, and midazolam, in order to obtain a rapid, dense, and long-lasting BPB.3
Evidence from various research indicates that adding dexamethasone perineurally does prolong the duration of analgesia. Use of perineural dexamethasone raises concerns about possible neurotoxicity, however the evidence is not yet definitive.4 In order to increase the duration of analgesia, researchers have been looking into the use of intravenous (IV) dexamethasone as a safer substitute for perineural dexamethasone. However, perineural route of dexamethasone administration remains off label. Additionally, moderate doses of IV dexamethasone have been investigated because of their possible systemic anti-inflammatory effects.5
This study aimed to assess the efficacy of IV and perineural dexamethasone in alleviating postoperative pain in adults who underwent supraclavicular BPB for elective upper limb procedures.
This prospective randomized double blinded study involved 44 patients aged from 18 to 60 years old, both sexes, American Society of Anesthesiologists (ASA) physical status I and II, posted for elective upper limb cancer surgeries (synovial sarcoma, liposarcoma, melanoma, squamous cell carcinoma and osteosarcoma) under supraclavicular BPB and tourniquet time less than 120 min. This study was done from 2022 to 2023 after Approval from the Ethical Committee Cairo University Hospitals, Cairo, Egypt (IRB AP2105-30106). The patients' written informed consents were acquired.
Infections at the location of the planned block puncture, neuropathies, mental illness, steroid treatment, uncontrolled diabetes, coagulopathy, and a history of allergy to local anesthetics were all reasons for exclusion.
2.1. Randomization
The patients were randomly divided into two groups: Group A (Perineural Dexamethasone group): 2 mL of dexamethasone (8 mg) combined with 28 mL of bupivacaine 0.25% concentration perineurally, along with 2 mL of normal saline as an IV placebo and group B (Systemic Dexamethasone group): 2 mL normal saline was combined with 28 mL of bupivacaine 0.25% perineurally, and a 2 mL volume of dexamethasone (8 mg) was administered IV as a systemic adjuvant.
Laboratory examinations (whole blood picture, liver function tests, renal function tests, prothrombin time, and partial thromboplastin time) and chest x-ray and electrocardiogram (ECG) were performed on all patients after a thorough history and physical examination.
ECG, non-invasive blood pressure monitors, and pulse oximeters were used to keep patients monitored during the operation. Nasal prongs or a face mask were used to administer additional oxygen if necessary.
For every patient, we utilized sterilization solution (Bovidine iodine 10%), sterile gloves, a marking pen, an 18-gauge cannula, medication-filled 10-mL syringes, and a SonoSite M-Turbo C ultrasound machine with a high-frequency linear probe.
We positioned the patients in a semi-sitting position at a 45-degree angle, with their heads turned to face the other side of the block. Then, we adducted and pulled down the arm of the block side. After applying the ultrasonic linear probe to the supraclavicular fossa, identification of the subclavian artery using Doppler wave was done. The BP trunks and divisions were visualized and identified as superior, posterior and lateral to the artery.
Group A; “perineural Group” received the nerve block with 28 mL 0.25% bupivacaine and 2 mL dexamethasone (8 mg) as perineural adjuvant and 2 mL of normal saline as IV placebo, while Group B; “IV group” received 28 mL 0.25% bupivacaine and 2 mL of normal saline perineurally and 2 mL dexamethasone (8 mg) as a systemic adjuvant.
2.2. Assessment of sensory block
Through the use of a pin prick test, we were able to determine the degree of sensory block in each of the four upper-limb nerve areas (musculocutaneous nerve, which includes nerve fibers from roots C5 to C7) which also has a sensory branch that serves the outside of the forearm. Nerve fibers from C6 to T1 make up the median nerve, which delivers sensation to the side of the hand as well as three and a half fingers. Nerve fibers from each of the BP roots come together to form the radial nerve. It innervates a portion of the hand and the back of the forearm, allowing for sensation. Consisting of the (C8 and T1 roots, the ulnar nerve is created). For the little finger, a portion of the ring finger, and the area on the inside of the palm. with a three-point scale; 0- for normal sensation; 1- for analgesia (no pain), and 2- for anesthesia (no feeling whatsoever). sensory blockage of the musculocutaneous, median, radial, and ulnar nerves. On one side of the forearm, on the other side of the thumb, on the side of the hand opposite the palm, and on the side of the fifth finger, respectively,
The duration from the end of the administration of the local anesthetic till complete sensory block was referred to as the onset time for sensory block.
The duration of sensory block was determined by the time it took for the anesthesia to fully subside after sensory block had been fully applied.
2.3. Motor block assessment
To determine the presence of motor block, we used the modified Bromage scale, which accounts for the radial (thumb abduction), ulnar (thumb adduction), median (thumb opposition), thumb, and musculocutaneous nerve (flexion of the elbow). When compared to the contralateral limb, it was rated as follows: 0 for total block, 1 for partial block (decreased muscle activity), and 2 for no block (normal muscle activity). A motor block was considered complete when the score was 0, and the time it took for the block to begin was calculated as the duration between injection and block completion. If full sensory and motor block were not obtained 30 min after injection, the block was deemed to have failed. In such cases, the subject was re-injected with GA and removed from the trial.6 Overdosing, quick absorption, or an inadvertent intravenous infusion are the three main causes of systemic toxicity in relation to local anesthetics. Dysarthria, metallic taste, and numbness around the mouth are common symptoms of systemic poisoning. toxicity to the cardiovascular system (low blood pressure, irregular heartbeats, and sudden cardiac death) or the central nervous system (CNS) (tinnitus, disorientation, and seizures).
Post-operatively, patients were taken to the post-anesthesia care unit (PACU). Over the course of an hour, their vitals (consciousness, blood pressure, heart rate, respiration rate, and any strange sensation or weakness in their limbs) were monitored meticulously to make sure they were within normal ranges. The patients were moved to the ward after this observation time ended so that they could be closely monitored for the first day after surgery.
The study drugs and any adverse effects on the procedure or its complications were monitored for patients. These components comprised hypotension or hypertension (a drop or increase of 20% from the initial value), bradycardia (HR less than 50 beats per min) or tachycardia (HR greater than 120 beats per min), nausea, vomiting, and hypoxemia (defined as SpO2 less than 90%).
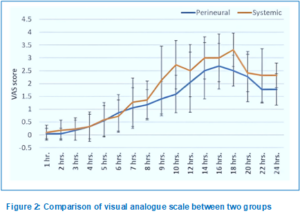
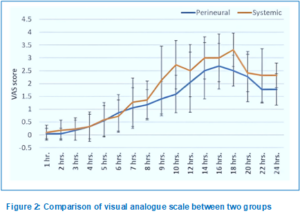
Using a visual analogue scale (VAS), patients' postoperative pain was monitored hourly for the first 10 h, and then every two hours till 24 h after end of surgery.
The primary outcomes were duration of analgesia, while secondary outcomes were onset time of motor and sensory block, postoperative pain scores, total dose of narcotic analgesic and number of postoperative doses of morphine.
2.4. Sample size calculation
According to a prior study by Aliste et al.,7 there was a 4 ± 4.6-hour difference in the duration of analgesics between the two groups; 22 patients were needed for each group. Utilizing PS: Power and Sample Size Calculation Software Version 3.1.2 (Vanderbilt University, Nashville, Tennessee, USA), the necessary calculations for sample size were carried out.
2.5. Statistical analysis
For the statistical analysis, the software SPSS v26 (IBM Inc., Chicago, IL, USA) was utilized. The means and standard deviations (SD) of the two groups' quantitative variables were compared using an unpaired Student's t-test. Qualitative variables, presented as frequencies and percentages, were typically analyzed using Fisher's exact test or Chi-square test, as appropriate. For statistical significance, a two-tailed P value below 0.05 was considered.

Out of Fifty patients that were evaluated, three did not fulfill the requirements, and three had failed block. We divided the remaining patients evenly into two groups, each with 22 patients. We examined the data statistically after following up with all of the assigned patients (Figure 1).
The two groups did not differ significantly with respect to age, sex, or weight (Table 1). Onset time for sensory and motor block were significant higher in systemic group than perineural groups (P < 0.05). Duration of sensory block and analgesia of the block were significantly lower in systemic groups than perineural groups (P < 0.05). The two groups did not differ significantly with respect to the duration of motor block (Table 2).
Statistics applied to all patients and VAS recordings revealed that those in the systemic group achieved a score of 4 or higher at a faster rate than those in the perineural group (Figure 2).
A total of six patients in the perineural group required a single dosage of morphine (0.03 mg/Kg), with four of those patients requiring a second dose. 18 patients in the systemic group required a single dose, 10 required a second dose of morphine. The two groups exhibited a significant difference in the number of patients who required a second dosage of morphine (P = 0.030). The two groups' total morphine dosages were significantly different (Table 3).
The intraoperative recording of SBP, DBP, and HR was compared statistically. There was no significance in both groups (Figure 3-A, B & C).
Three patients experienced adverse symptoms, including nausea and vomiting.
Inadequate pain management following surgery may lead to unfavorable consequences such as increased risk of chronic pain, lengthier hospital stays, and pain.8 On the other hand, effective postoperative pain management can result in reduced stress, improved patient satisfaction, and better overall surgical outcomes.9
Our results demonstrate that the perineural group's sensory block and motor block start timings were much lower than those of the IV group. The perineural group had a much longer sensory block than the IV group. Neither group differed significantly from the other in terms of the duration of motor block. In the same line, Pahari et al. discovered that the perineural group's sensory blocking lasted much less time than the IV group.10 In agreement with our study, Weheba et al. revealed that the perineural group had far shorter onset timings for sensory block and motor block than the IV group.11 The perineural group also had a much longer sensory block than the IV group. Conversely, motor block lasted longer in the perineural group compared to the IV group. This was consistent with the findings of Nadeem and Butt showed that the perineural group had a substantially shorter onset time for sensory block and motor block compared to the IV group. 12
In this study, the duration of block analgesia was much longer in the perineural group than in the IV group.
When used in conjunction with nerve blocks, dexamethasone may alleviate pain by obstructing nociceptive C fibers, decreasing ectopic neuronal discharge, combating both systemic and localized inflammation, and altering the immunological response to injury via neuropeptides. This agreed with Pahari et al., who discovered that following an axillary BPB, the perineural group experienced considerably longer analgesia than the IV group.10 Supporting our study, Aliste et al. corroborate our investigation by showing that the perineural group experienced considerably longer postoperative analgesia compared to the IV group following an axillary BPB.7 In contrast, Nadeem and Butt highlighted that the time of analgesia not substantially distinct between the perineural and IV groups.
Results showed no statistically significant difference in the proportion of patients requiring a single dose of postoperative morphine between the two groups. Contrarily, the perineural group had a lower rate of patients who needed a second dose of postoperative morphine than the IV group. Compared to the IV group, the perineural group required a far smaller overall dose of morphine. In the same line, Weheba et al. demonstrated that the perineural group used substantially less opioids than the IV group.11 This agreed with Sakae et al. [13] who found that compared to the IV group, the perineural group had a substantially decreased number of patients requiring opioids.13 However, Lee et al. illustrated that the total number of opioid requests did not differ considerably between the two groups.14
Our results demonstrated that a considerably lower VAS score was observed in the perineural group when compared to the IV group. In agreement with our study, Pahari et al. found a substantial distinct between the perineural and IV groups with respect to pain scores.10
Supporting our study, Weheba et al. discovered that the pain score was considerably reduced in the perineural group compared to the IV group.11 On the other hand, Chun et al. reported that the pain score of the two groups were not substantially different.15
All groups showed similar levels of intraoperative SBP, DBP, and HR. This was in agreement with the results of Weheba et al., who reported that the intraoperative HR and mean arterial blood pressure were not substantially different between the perineural group and the IV group. In the same line, Nadeem and Butt found that the increase in blood pressure was insignificantly different between the perineural group and the IV group.12
According to the findings in our study, adverse effects regarding nausea and vomiting occurred in three patients. Pneumothorax did not occur in any of the patients. In terms of the occurrence of adverse effects, there were no notable variations across the groups. In the same context, Sakae et al. discovered that 4 patients in the IV group had nausea and vomiting, while only one patient in the perineural group experienced these symptoms.13 In this regard, Chun et al. stated that that the IV group had six patients experiencing nausea, while the perineural group had three patients.15
The present study was constrained by its small sample size, reliance on a single center, not comparing findings of the IV and perineural dexamethasone in different doses and concentrations and not comparing findings of the IV and perineural dexamethasone with other anesthetics.
In ultrasound-guided supraclavicular brachial plexus block, addition of perineural dexamethasone offers a more prolonged motor and sensory blocks, as well as postoperative analgesia than, concurrent intravenous use of dexamethasone. To maximize therapeutic efficacy, further studies are recommended to discover the best dosages of intravenous and perineural dexamethasone.
7. Data availability
The numerical data generated during this research is available with the authors.
8. Funding
The study utilized the hospital resources only, and no external or industry funding was involved.
9. Conflict of interest
Authors declare that there was no conflict of interest.
10. Authors’ contribution
MAK, ASA: Study concept and design.
GMK: Analysis and interpretation of data.
GE: Critical revision of the manuscript for important intellectual content.
AMS: Administrative, technical, and material support.
Author affiliation:
- Mahmoud Ahmed Kamel, Department of Anesthesiology, Surgical Intensive Care & Pain Medicine, National Cancer Institute, Cairo University, Cairo, Egypt; Email: Mkamel_76@hotmail.com
- Ahmed Saad Abdelmonem, Department of Anesthesiology, Surgical Intensive Care & Pain Medicine, National Cancer Institute, Cairo University, Cairo, Egypt; Email: dr_sa3d@yahoo.com
- Gehan Muhammed Kamal, Department of Anesthesiology, Surgical Intensive Care & Pain Medicine, National Cancer Institute, Cairo University, Cairo, Egypt; Email: jehan.kamal@yahoo.com
- Ghada El Awady, Department of Anesthesiology, Surgical Intensive Care & Pain Medicine, National Cancer Institute, Cairo University, Cairo, Egypt; Email: ghadaelawady@yahoo.com
- Ahmed Mohamed Soliman, Department of Anesthesiology, Surgical Intensive Care & Pain Medicine, National Cancer Institute, Cairo University, Cairo, Egypt; Email: ams21787arif@hotmail.com
ABSTRACT
Background & Objectives: Dexamethasone is well known to potentiate the efficacy and the duration of local anesthetic drugs. The anesthetists have used this combination in spinal and epidural analgesia with satisfaction. We evaluated the efficacy of intravenous (IV) dexamethasone vs perineural administration in reducing postoperative pain in adults having supraclavicular brachial plexus blocks (BPB) for elective procedures involving the upper limbs.
Methodology: This prospective randomized, double blind study involved 44 patients aged 18 to 60 y, both sexes, posted for elective upper limb cancer (synovial sarcoma, liposarcoma, melanoma, squamous cell carcinoma and osteosarcoma) surgeries under supraclavicular block, with an expected tourniquet time less than 120 min. Patients were divided into two equal groups: Perineural Dexamethasone group: 2 mL of dexamethasone (8 mg) combined with 28 mL of bupivacaine 0.25% concentration perineurally, along with 2 mL of normal saline as an IV placebo and systemic dexamethasone group: normal saline 2 mL was combined with 28 mL of bupivacaine 0.25% perineurally, and dexamethasone 2 mL (8 mg) was administered IV.
Results: Onset time for sensory and motor block were significantly higher in systemic than perineural groups (P < 0.05). Duration of sensory blocks and duration of analgesia of the block were significantly lower in system than perineural groups (P < 0.05). There was significant difference between the two groups as regards the number of patients who needed a second dose of morphine (P = 0.030). Total morphine doses were significantly different between both groups. The duration of motor block was insignificantly different between both groups.
Conclusions: When compared to its IV counterpart, perineural dexamethasone offers a prolonged duration of motor block, sensory block, and postoperative analgesia in ultrasound-guided supraclavicular brachial plexus block.
Abbreviations: BPB: brachial plexus blocks, IV: intravenous, PACU: post-anesthesia care unit
Keywords: Cancer; Perineural; Intravenous; Dexamethasone; Dysarthria; Pain; Supraclavicular Plexus Nerve Block; Upper Limb Surgeries; VAS
Citation: Kamel MA, Abdelmonem AS, KamalGM, El Awady G, Soliman AM. Comparative study between perineural versus intravenous dexamethasone in prolonging the analgesic effect of supraclavicular plexus nerve block in upper limb surgeries. Anaesth. pain intensive care 2025;29(2):178-184. DOI: 10.35975/apic.v29i2.2701
Received: January 19, 2025; Reviewed: February 15, 2025; Accepted: February 15, 2025
1. INTRODUCTION
The brachial plexus block (BPB) is a common and well-liked method of administering analgesia and peri-operative anesthesia during procedures involving the upper limbs. For surgeries that are conducted below the shoulder joint, the supraclavicular approach is the most consistent and straightforward method. Patients with multiple cardio-respiratory problems can benefit from a regional nerve block since it lowers their anxiety before surgery and allows them to utilize less anesthetic.1
Ultrasound guidance is a reliable and safe technique in peripheral nerve blocks. It also plays a crucial and an increasing role in medicine nowadays due its low cost, the absence of ionizing radiation and its high temporal resolution.2
The local anesthetics alone for supraclavicular BPB blocking ensure optimal working conditions, although the pain relief after the procedure is brief. Local anesthetics were combined with a variety of adjuvants, such as opioids, clonidine, neostigmine, and midazolam, in order to obtain a rapid, dense, and long-lasting BPB.3
Evidence from various research indicates that adding dexamethasone perineurally does prolong the duration of analgesia. Use of perineural dexamethasone raises concerns about possible neurotoxicity, however the evidence is not yet definitive.4 In order to increase the duration of analgesia, researchers have been looking into the use of intravenous (IV) dexamethasone as a safer substitute for perineural dexamethasone. However, perineural route of dexamethasone administration remains off label. Additionally, moderate doses of IV dexamethasone have been investigated because of their possible systemic anti-inflammatory effects.5
This study aimed to assess the efficacy of IV and perineural dexamethasone in alleviating postoperative pain in adults who underwent supraclavicular BPB for elective upper limb procedures.
2. METHODOLOGY
This prospective randomized double blinded study involved 44 patients aged from 18 to 60 years old, both sexes, American Society of Anesthesiologists (ASA) physical status I and II, posted for elective upper limb cancer surgeries (synovial sarcoma, liposarcoma, melanoma, squamous cell carcinoma and osteosarcoma) under supraclavicular BPB and tourniquet time less than 120 min. This study was done from 2022 to 2023 after Approval from the Ethical Committee Cairo University Hospitals, Cairo, Egypt (IRB AP2105-30106). The patients' written informed consents were acquired.
Infections at the location of the planned block puncture, neuropathies, mental illness, steroid treatment, uncontrolled diabetes, coagulopathy, and a history of allergy to local anesthetics were all reasons for exclusion.
2.1. Randomization
The patients were randomly divided into two groups: Group A (Perineural Dexamethasone group): 2 mL of dexamethasone (8 mg) combined with 28 mL of bupivacaine 0.25% concentration perineurally, along with 2 mL of normal saline as an IV placebo and group B (Systemic Dexamethasone group): 2 mL normal saline was combined with 28 mL of bupivacaine 0.25% perineurally, and a 2 mL volume of dexamethasone (8 mg) was administered IV as a systemic adjuvant.
Laboratory examinations (whole blood picture, liver function tests, renal function tests, prothrombin time, and partial thromboplastin time) and chest x-ray and electrocardiogram (ECG) were performed on all patients after a thorough history and physical examination.
ECG, non-invasive blood pressure monitors, and pulse oximeters were used to keep patients monitored during the operation. Nasal prongs or a face mask were used to administer additional oxygen if necessary.
For every patient, we utilized sterilization solution (Bovidine iodine 10%), sterile gloves, a marking pen, an 18-gauge cannula, medication-filled 10-mL syringes, and a SonoSite M-Turbo C ultrasound machine with a high-frequency linear probe.
We positioned the patients in a semi-sitting position at a 45-degree angle, with their heads turned to face the other side of the block. Then, we adducted and pulled down the arm of the block side. After applying the ultrasonic linear probe to the supraclavicular fossa, identification of the subclavian artery using Doppler wave was done. The BP trunks and divisions were visualized and identified as superior, posterior and lateral to the artery.
Group A; “perineural Group” received the nerve block with 28 mL 0.25% bupivacaine and 2 mL dexamethasone (8 mg) as perineural adjuvant and 2 mL of normal saline as IV placebo, while Group B; “IV group” received 28 mL 0.25% bupivacaine and 2 mL of normal saline perineurally and 2 mL dexamethasone (8 mg) as a systemic adjuvant.
2.2. Assessment of sensory block
Through the use of a pin prick test, we were able to determine the degree of sensory block in each of the four upper-limb nerve areas (musculocutaneous nerve, which includes nerve fibers from roots C5 to C7) which also has a sensory branch that serves the outside of the forearm. Nerve fibers from C6 to T1 make up the median nerve, which delivers sensation to the side of the hand as well as three and a half fingers. Nerve fibers from each of the BP roots come together to form the radial nerve. It innervates a portion of the hand and the back of the forearm, allowing for sensation. Consisting of the (C8 and T1 roots, the ulnar nerve is created). For the little finger, a portion of the ring finger, and the area on the inside of the palm. with a three-point scale; 0- for normal sensation; 1- for analgesia (no pain), and 2- for anesthesia (no feeling whatsoever). sensory blockage of the musculocutaneous, median, radial, and ulnar nerves. On one side of the forearm, on the other side of the thumb, on the side of the hand opposite the palm, and on the side of the fifth finger, respectively,
The duration from the end of the administration of the local anesthetic till complete sensory block was referred to as the onset time for sensory block.
The duration of sensory block was determined by the time it took for the anesthesia to fully subside after sensory block had been fully applied.
2.3. Motor block assessment
To determine the presence of motor block, we used the modified Bromage scale, which accounts for the radial (thumb abduction), ulnar (thumb adduction), median (thumb opposition), thumb, and musculocutaneous nerve (flexion of the elbow). When compared to the contralateral limb, it was rated as follows: 0 for total block, 1 for partial block (decreased muscle activity), and 2 for no block (normal muscle activity). A motor block was considered complete when the score was 0, and the time it took for the block to begin was calculated as the duration between injection and block completion. If full sensory and motor block were not obtained 30 min after injection, the block was deemed to have failed. In such cases, the subject was re-injected with GA and removed from the trial.6 Overdosing, quick absorption, or an inadvertent intravenous infusion are the three main causes of systemic toxicity in relation to local anesthetics. Dysarthria, metallic taste, and numbness around the mouth are common symptoms of systemic poisoning. toxicity to the cardiovascular system (low blood pressure, irregular heartbeats, and sudden cardiac death) or the central nervous system (CNS) (tinnitus, disorientation, and seizures).
Post-operatively, patients were taken to the post-anesthesia care unit (PACU). Over the course of an hour, their vitals (consciousness, blood pressure, heart rate, respiration rate, and any strange sensation or weakness in their limbs) were monitored meticulously to make sure they were within normal ranges. The patients were moved to the ward after this observation time ended so that they could be closely monitored for the first day after surgery.
The study drugs and any adverse effects on the procedure or its complications were monitored for patients. These components comprised hypotension or hypertension (a drop or increase of 20% from the initial value), bradycardia (HR less than 50 beats per min) or tachycardia (HR greater than 120 beats per min), nausea, vomiting, and hypoxemia (defined as SpO2 less than 90%).
Using a visual analogue scale (VAS), patients' postoperative pain was monitored hourly for the first 10 h, and then every two hours till 24 h after end of surgery.
The primary outcomes were duration of analgesia, while secondary outcomes were onset time of motor and sensory block, postoperative pain scores, total dose of narcotic analgesic and number of postoperative doses of morphine.
2.4. Sample size calculation
According to a prior study by Aliste et al.,7 there was a 4 ± 4.6-hour difference in the duration of analgesics between the two groups; 22 patients were needed for each group. Utilizing PS: Power and Sample Size Calculation Software Version 3.1.2 (Vanderbilt University, Nashville, Tennessee, USA), the necessary calculations for sample size were carried out.
2.5. Statistical analysis
For the statistical analysis, the software SPSS v26 (IBM Inc., Chicago, IL, USA) was utilized. The means and standard deviations (SD) of the two groups' quantitative variables were compared using an unpaired Student's t-test. Qualitative variables, presented as frequencies and percentages, were typically analyzed using Fisher's exact test or Chi-square test, as appropriate. For statistical significance, a two-tailed P value below 0.05 was considered.

3. RESULTS
Out of Fifty patients that were evaluated, three did not fulfill the requirements, and three had failed block. We divided the remaining patients evenly into two groups, each with 22 patients. We examined the data statistically after following up with all of the assigned patients (Figure 1).
The two groups did not differ significantly with respect to age, sex, or weight (Table 1). Onset time for sensory and motor block were significant higher in systemic group than perineural groups (P < 0.05). Duration of sensory block and analgesia of the block were significantly lower in systemic groups than perineural groups (P < 0.05). The two groups did not differ significantly with respect to the duration of motor block (Table 2).
Statistics applied to all patients and VAS recordings revealed that those in the systemic group achieved a score of 4 or higher at a faster rate than those in the perineural group (Figure 2).
| Table 1: Demographic data and duration of surgery between systemic and perineural group | |||||
| Parameter | Perineural group (n=22) | Systemic group
(n=22) |
t/X2 | P-value | |
| Age (y) | 52.55 ± 3.7 | 51.32 ± 3.92 | 1.068 | 0.292 | |
| Gender | Male | 10 (45.5%) | 11 (50%) | 0.091 | 0.763 |
| Female | 12 (54.5%) | 11 (50%) | |||
| Weight (Kg) | 78.4 ± 6.12 | 76.13 ± 8.81 | 0.994 | 0.326 | |
| Duration of surgery | 83.36 ± 14.80 | 76.59 ± 8.65 | 1.854 | 0.071 | |
| Data are presented as mean ± SD. T= t-test, X2= Chi-square, *significant p value <0.05. | |||||
A total of six patients in the perineural group required a single dosage of morphine (0.03 mg/Kg), with four of those patients requiring a second dose. 18 patients in the systemic group required a single dose, 10 required a second dose of morphine. The two groups exhibited a significant difference in the number of patients who required a second dosage of morphine (P = 0.030). The two groups' total morphine dosages were significantly different (Table 3).
| Table 2: Block and duration of analgesia of the block between systemic and perineural group | ||||
| Variables | Perineural group (n=22) | Systemic group
(n=22) |
t/X2 | P |
| Onset time of sensory block (min) | 16.82 ± 1.40 | 24.41 ± 2.15 | <0.001* | <0.001* |
| Duration of sensory block (min) | 715.45 ± 76.84 | 647.05 ± 59.81 | 0.002* | 0.002* |
| Onset time of motor block (min) | 24.86 ± 2.17 | 26.73 ± 2.43 | 0.010* | 0.010* |
| Duration of motor block (min) | 605.00 ± 59.82 | 587.27 ± 26.17 | 0.210 | 0.210 |
| Duration of analgesia of the block (h) | 16.36 ± 1.87 | 13.41 ± 1.62 | -- | <0.001* |
| Data are presented as mean ± SD. *significant P <0.05. | ||||
| Table 3: Comparison of the numbers of postoperative doses of morphine in the study groups | ||||||
| Variables | N | Perineural group
(n=22) |
N | Systemic group
(n=22) |
t | P |
| Morphine 1st dose | 6 | 2.08 ± 0.08 | 18 | 2.14 ± 0.10 | 1.197 | 0.244 |
| Morphine 2nd dose | 4 | 2.00 ± 0.00 | 10 | 2.13 ± 0.10 | 2.457 | 0.030* |
| Total morphine doses (mg) | 20.5 ± 3.4 | 59.75 ± 5.84 | 27.243 | <0.001* | ||
| Data are presented as mean ± SD. *significant P <0.05. T= t-test. | ||||||
The intraoperative recording of SBP, DBP, and HR was compared statistically. There was no significance in both groups (Figure 3-A, B & C).
Three patients experienced adverse symptoms, including nausea and vomiting.
4. DISCUSSION
Inadequate pain management following surgery may lead to unfavorable consequences such as increased risk of chronic pain, lengthier hospital stays, and pain.8 On the other hand, effective postoperative pain management can result in reduced stress, improved patient satisfaction, and better overall surgical outcomes.9
Our results demonstrate that the perineural group's sensory block and motor block start timings were much lower than those of the IV group. The perineural group had a much longer sensory block than the IV group. Neither group differed significantly from the other in terms of the duration of motor block. In the same line, Pahari et al. discovered that the perineural group's sensory blocking lasted much less time than the IV group.10 In agreement with our study, Weheba et al. revealed that the perineural group had far shorter onset timings for sensory block and motor block than the IV group.11 The perineural group also had a much longer sensory block than the IV group. Conversely, motor block lasted longer in the perineural group compared to the IV group. This was consistent with the findings of Nadeem and Butt showed that the perineural group had a substantially shorter onset time for sensory block and motor block compared to the IV group. 12
In this study, the duration of block analgesia was much longer in the perineural group than in the IV group.
When used in conjunction with nerve blocks, dexamethasone may alleviate pain by obstructing nociceptive C fibers, decreasing ectopic neuronal discharge, combating both systemic and localized inflammation, and altering the immunological response to injury via neuropeptides. This agreed with Pahari et al., who discovered that following an axillary BPB, the perineural group experienced considerably longer analgesia than the IV group.10 Supporting our study, Aliste et al. corroborate our investigation by showing that the perineural group experienced considerably longer postoperative analgesia compared to the IV group following an axillary BPB.7 In contrast, Nadeem and Butt highlighted that the time of analgesia not substantially distinct between the perineural and IV groups.
Results showed no statistically significant difference in the proportion of patients requiring a single dose of postoperative morphine between the two groups. Contrarily, the perineural group had a lower rate of patients who needed a second dose of postoperative morphine than the IV group. Compared to the IV group, the perineural group required a far smaller overall dose of morphine. In the same line, Weheba et al. demonstrated that the perineural group used substantially less opioids than the IV group.11 This agreed with Sakae et al. [13] who found that compared to the IV group, the perineural group had a substantially decreased number of patients requiring opioids.13 However, Lee et al. illustrated that the total number of opioid requests did not differ considerably between the two groups.14
Our results demonstrated that a considerably lower VAS score was observed in the perineural group when compared to the IV group. In agreement with our study, Pahari et al. found a substantial distinct between the perineural and IV groups with respect to pain scores.10
Supporting our study, Weheba et al. discovered that the pain score was considerably reduced in the perineural group compared to the IV group.11 On the other hand, Chun et al. reported that the pain score of the two groups were not substantially different.15
All groups showed similar levels of intraoperative SBP, DBP, and HR. This was in agreement with the results of Weheba et al., who reported that the intraoperative HR and mean arterial blood pressure were not substantially different between the perineural group and the IV group. In the same line, Nadeem and Butt found that the increase in blood pressure was insignificantly different between the perineural group and the IV group.12
According to the findings in our study, adverse effects regarding nausea and vomiting occurred in three patients. Pneumothorax did not occur in any of the patients. In terms of the occurrence of adverse effects, there were no notable variations across the groups. In the same context, Sakae et al. discovered that 4 patients in the IV group had nausea and vomiting, while only one patient in the perineural group experienced these symptoms.13 In this regard, Chun et al. stated that that the IV group had six patients experiencing nausea, while the perineural group had three patients.15
5. LIMITATIONS
The present study was constrained by its small sample size, reliance on a single center, not comparing findings of the IV and perineural dexamethasone in different doses and concentrations and not comparing findings of the IV and perineural dexamethasone with other anesthetics.
6. CONCLUSION
In ultrasound-guided supraclavicular brachial plexus block, addition of perineural dexamethasone offers a more prolonged motor and sensory blocks, as well as postoperative analgesia than, concurrent intravenous use of dexamethasone. To maximize therapeutic efficacy, further studies are recommended to discover the best dosages of intravenous and perineural dexamethasone.
7. Data availability
The numerical data generated during this research is available with the authors.
8. Funding
The study utilized the hospital resources only, and no external or industry funding was involved.
9. Conflict of interest
Authors declare that there was no conflict of interest.
10. Authors’ contribution
MAK, ASA: Study concept and design.
GMK: Analysis and interpretation of data.
GE: Critical revision of the manuscript for important intellectual content.
AMS: Administrative, technical, and material support.
11. REFERENCES
- Shrestha B, Maharjan S, Shrestha S, Gautam B, Thapa C, Thapa P, et al. Comparative study between tramadol and dexamethasone as an admixture to bupivacaine in supraclavicular brachial plexus block. JNMA J Nepal Med Assoc. 2007;46:158-64. [PubMed]
- Mahesh M. The essential physics of medical imaging, third edition. Med Phys. 2013;40. [PubMed] DOI: 1118/1.4811156
- Golwala M, Swadia V, Dhimar AA, Sridhar N. Pain relief by dexamethasone as an adjuvant to local anaesthetics in supraclavicular brachial plexus block. J Anaesthesiol Clin Pharmacol. 2009;25:285-8. [FreeFullText]
- Rosenfeld D, Ivancic M, Hattrup S, Renfree K, Watkins A, Hentz J, et al. Perineural versus intravenous dexamethasone as adjuncts to local anaesthetic brachial plexus block for shoulder surgery. Anaesthesia. 2016;71:380-8. [PubMed] DOI: 1111/anae.13409
- De Oliveira GS, Almeida MD, Benzon HT, McCarthy RJ. Perioperative single dose systemic dexamethasone for postoperative pain: a meta-analysis of randomized controlled trials. Anesthesiology. 2011;115:575-88. [PubMed] DOI: 1097/ALN.0b013e31822a24c2
- Ribeiro KS, Ollapally A, Misquith J. Dexamethasone as an adjuvant to bupivacaine in supraclavicular brachial plexus block in paediatrics for post-operative analgesia. J Clin Diagn Res. 2016;10:Uc01-uc4. [PubMed] DOI: 7860/JCDR/2016/22089.8957
- Aliste J, Leurcharusmee P, Engsusophon P, Gordon A, Michelagnoli G, Sriparkdee C, et al. A randomized comparison between intravenous and perineural dexamethasone for ultrasound-guided axillary block. Can J Anaesth. 2017;64:29-36. [PubMed] DOI: 1007/s12630-016-0741-8
- Park R, Mohiuddin M, Arellano R, Pogatzki-Zahn E, Klar G, Gilron I. Prevalence of postoperative pain following hospital discharge: Protocol for a systematic review. JMIR Res Protoc. 2020;9:22437. [PubMed] DOI: 2196/22437
- Tang JC, Ma JW, Jian JJ, Shen J, Cao LL. Effect of different anesthetic modalities with multimodal analgesia on postoperative pain level in colorectal tumor patients. World J Gastroenterol Oncol. 2024;16:364. [PubMed] DOI: 4251/wjgo.v16.i2.364
- Pahari T, Hirachan R, Neupane S, Bhattarai KM, Pakhrin P. Comparative study on the efficacy of perineural vs intravenous dexamethasone as an adjunct to bupivacaine to prolong analgesia after axillary brachial plexus block in a tertiary care center, Pokhara. JGMC Nepal. 2024;17:22-6. DOI: 3126/jgmcn.v17i1.61120
- Moawad HE, El-Ebahnsawy NS, Badr-Eldin MN, El-Badrawy RE. Intravenous versus perineural dexamethasone in interscalene nerve block with levobupivacaine for shoulder and upper arm surgeries. Egypt J Hosp Med. 2022;86:882-90. [FreeFullText]
- Nadeem A, Butt MM. Comparison of intravenous dexamethasone adjunctive to bupivacaine with perineural dexamethasone adjunctive to bupivacaine in ultra sound guided interscelene brachial plexus block. Med Forum Mon. 2020;31. [FreeFullText]
- Sakae TM, Marchioro P, Schuelter-Trevisol F, Trevisol DJ. Dexamethasone as a ropivacaine adjuvant for ultrasound-guided interscalene brachial plexus block: A randomized, double-blinded clinical trial. J Clin Anesth. 2017;38:133-6. [PubMed] DOI: 1016/j.jclinane.2017.02.004
- Lee HJ, Woo JH, Chae JS, Kim YJ, Shin SJ. Intravenous Versus Perineural Dexamethasone for Reducing Rebound Pain After Interscalene Brachial Plexus Block: A Randomized Controlled Trial. J Korean Med Sci. 2023;38:183-98. [PubMed] DOI: 3346/jkms.2023.38.e183
- Chun EH, Kim YJ, Woo JH. Which is your choice for prolonging the analgesic duration of single-shot interscalene brachial blocks for arthroscopic shoulder surgery? intravenous dexamethasone 5 mg vs. perineural dexamethasone 5 mg randomized, controlled, clinical trial. Medicine (Baltimore). 2016;95:3828-987. [PubMed] DOI: 1097/MD.0000000000003828