Ahmed Abdelrahman Boeith 1, Amr Fouad Hafez 2, Mohamed A. Wareth 3, Doaa Mohammed Kamal Eldin 4, Farouk Kamal 5
Authors contribution:
Background: Postoperative pain after laparoscopic abdominal surgeries can be severe. Despite multimodal analgesia protocols, administration of high doses of opioids is often required hindering early mobilization and discharge of the patient from the day surgery setting and is suboptimal in an Early Recovery after Surgery (ERAS) setting. A prospective randomized clinical comparative double blinded study was conducted at Ain Shams University Hospitals.
We evaluated and compared the analgesic effect of ultrasound-guided erector spinae plane (ESP) block with ultrasound-guided posterior Quadratus Lumborum Block (QLB II) in laparoscopic abdominal surgeries.
Methodology: This study was carried on 82 adult patients undergoing laparoscopic surgeries allocated randomly into 2 equal groups ESPB group and QLB II group. The first time to rescue analgesia was reported as a primary outcome. The secondary outcomes include opioid consumption intraoperative, the time of the performance of the block, visual analogue scale (VAS) at rest, at cough and during deep inspiration and total dose of rescue analgesia.
Results: No significant difference recorded between both groups regarding demographic data, first time to rescue analgesia, opioid consumption intraoperative, VAS score and total dose of postoperative analgesia. However, the duration of block procedure was significantly shorter in ESPB group relative to QLB II group (14.2 ± 1.6 min vs 25.3 ± 2.8 min, P < 0.001).
Abbreviations: ERAS: Early Recovery after Surgery, ESP: erector spinae plane, QLB: Quadratus Lumborum Block, VAS: visual analogue scale
Conclusion: Both quadratus lumborum plane block and erector spinae plane block can control postoperative pain after laparoscopic abdominal surgeries; however, erector spinae plane block provided more time saving during its performance.
Keywords: analgesia; ERAS; Erector spinae block; Laparoscopic; Postoperative pain; Quadratus lumborum block; Ultrasound; VAS score
Citation: Boeith AA, Hafez AF, Kamal F, Kamal Eldin DM, Abdelwareth M. Ultrasound guided quadratus lumborum block versus ultrasound guided erector spinae plane block for postoperative analgesia in laparoscopic abdominal surgeries. Anaesth. pain intensive care 2025;29(2):300-306. DOI: 10.35975/apic.v29i2.2592
Received: May 09, 2024; Reviewed: October 26, 2024; Accepted: January 01, 2025
Regional anesthesia role is well established in abdominal surgery, with epidural analgesia being the cornerstone in perioperative analgesia since the early 1900s. However early mobilization, minimally invasive surgical techniques, and pharmacologic venous thromboprophylaxis are now recognized as key components of enhanced recovery after surgery. The search for motor-sparing, less-invasive, safer, and efficacious alternatives to epidural analgesia has been prioritized.1
With the evolution of the ultrasound machine in the operating theatres, the skills of regional anesthesia have been changed from landmark-based techniques to regional blocks administered under direct vision guided by the ultrasound machine.2 The ultrasound-guided Erector Spinae Plane (ESP) block is a novel truncal interfacial regional technique.3
Two techniques of the ESP block for thoracic and abdominal procedures have recently been discussed in literature. The insertion site is at the level of T5 transverse process, spreading between the C7 and T8 segmental levels, or at the level of T7-T9 transverse processes, covering the area between the T6 and T12 segmental levels.4 Quadratus lumborum block (QLB) is a posterior extension of the transversus abdominis plane block (TAP) block. It was first described by Dr Blanco, and it was later modified by Sauter et al. These blocks target both somatic structures covering the anterior abdominal wall, with suggestions of abdominal visceral coverage as well, most commonly using a lateral, posterior, or anterior approach.5
The lateral approach (previously QL1) involves depositing local anesthetic at the lateral border of the QL muscle, anterior to the aponeurosis of the transversus abdominis muscle and within the anterior thoracolumbar fascia. The posterior approach (previously QL2) involves injecting posterior to the QL muscle, in the middle thoracolumbar fascia. The anterior approach (also called the transmuscular QL block) involves injecting anterior to the QL muscle, between it and the psoas major muscle and in the anterior thoracolumbar fascia.6
This randomized prospective clinical comparative double blinded study was carried out in Ain shams university hospitals for 1 year on 82 adult patients (by using G power program, setting power at 80%, alpha error at 5%) with American Society of Anesthesiologists (ASA) Physical Status Class I and II, aged between 30 and 60 years, and scheduled for laparoscopic abdominal surgery. Written and informed consent was taken from each patient. Every patient received an explanation to the purpose of the study and had a secret code number to ensure privacy to participant and confidentiality of data.
Patients were randomly allocated into two equal groups:
A computer system was used for randomization by creating a list of number each number referred to one of the two groups. Block randomization was used to ensure equality of the groups. Each number was sealed in an opaque envelope. Then, each patient was asked to choose one of the envelopes and was given to an anesthesiologist who compared it to the computer-generated list and hence assigned to one of the two groups. The patients and the investigators who are responsible for assessing the primary and secondary outcomes were blinded to study group assignment. However, the attending intraoperative anesthesiologists and assessors were not blinded to study group assignment.
Patients included in the study aged 30–60 years, with ASA Physical Status Class I and II, scheduled for laparoscopic abdominal surgery under general anesthesia.
Patients excluded from the study if they showed infection at injection site, allergy to local anesthetics, coagulation disorders, severe obesity, physical or mental diseases which may interfere with the evaluation of pain scores, or kidney failure or liver failure.
All patients were assessed preoperatively, and instructed to fast for 8 hrs. On arrival to the operation theatre, Intravenous access was established, and lactated Ringer solution infused by rate 10 mL/kg. Patients received titration of 0.03 mg/kg midazolam intravenously as sedation. Standard monitors including non-invasive blood pressure, electrocardiogram (ECG), and pulse oximetry (SpO2) and capnography applied to monitor the perioperative hemodynamic parameters. For both groups, general anesthesia induced with IV injection of fentanyl (1 μg/kg) and propofol (2 mg/kg), and then, atracurium (0.5 mg/kg) was injected for endotracheal intubation. Mechanical ventilation was maintained to keep the end-tidal CO2 (EtCO2) values between 34 and 36 mmHg. Anesthesia continued with isoflurane 1%–2% in 100% oxygen. Incremental dose of atracurium (0.1 mg/kg) was given every 30 min or when needed.
After endotracheal intubation and before the start of the surgery, anesthesiologist performed the block techniques and administered the medication. Both blocks were performed under complete aseptic precautions using ultrasound machine.
2.1. In Group Q:
The patient was placed in the lateral decubitus position. After sterilization of the US site, needle entry, and draping, a low frequency curved probe of a transportable Fuji M-Turbo ultrasound system was placed horizontally in the anterior axillary line midway between the subcostal margin and the iliac crest to identify the triple abdominal muscle layers. Then, the probe moved posteriorly to the posterior axillary line until the QL muscle appeared with its attachment to the lateral edge of the transverse process of the L4 vertebral body, the psoas major muscle anteriorly, and the erector spinae muscle posteriorly; this is a well-recognizable pattern of a shamrock sign with three leaves.7 A 22-G, 80-mm needle echogenic needle was inserted in plane relative to the US probe, into the posterior aspect of the QL muscle (between QL and erector spinae muscle); this is known as QLB type 2. Then, 0.5 mL/kg of 0.25% bupivacaine was injected behind the muscle as a bolus dose on both sides.8
2.2. In Group E:
The patient was placed in lateral decubitus position. After sterilization of the US site, needle entry, and draping, a high frequency linear probe of a transportable Fuji M-Turbo ultrasound system was placed on the spinous process at T8 level on the parasagittal plane and then slide 2.5–3 cm laterally to visualize the transverse process and erector spinae muscle. Using the inplane technique, A 22-G, 80-mm needle echogenic needle was inserted between the transverse process and erector spinae muscle. Then 0.5 mL/kg of 0.25% bupivacaine was injected between the muscle and transverse process on both sides.9
Intravenous fentanyl (0.5 µg/kg) was given intraoperatively when any increase in MAP or HR more than 20% of baseline data occurred throughout the procedure. At the end of the surgery, anesthesia discontinued, reversal of muscle relaxation by 0.02 mg/kg atropine and 0.05 mg/kg prostigmine were given.
Patients were assessed in the immediate postoperative period, and then at 2, 6, 12 and at 24 h for the quality of analgesia using Visual Analogue Scale (VAS) score, and VAS more than 5 was managed by paracetamol 10 mg/kg IV every 8 hours and pethidine 50 mg IV as rescue analgesia.
2.4. The outcomes
The primary outcome of the study was the first time to rescue analgesia (recorded within the first 24 hour postoperatively). It was the time from the end of surgery to patient reporting VAS ≥ 5. Pain assessments are conducted by a researcher who was unaware of the grouping.
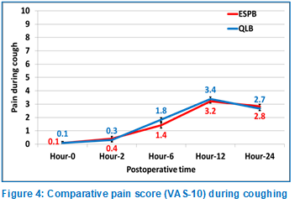
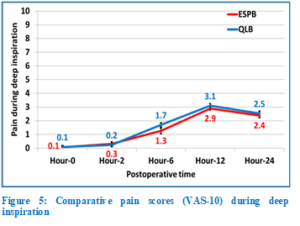
The secondary outcomes included the time spent on the performance of the block, intraoperative opioid consumption, VAS at rest, during cough and during deep inspiration (measured immediately after surgery, and at 2, 6, 12, and 24 hours postoperatively) on a scale of 0-10. Total dose of rescue analgesia (in the first 24 hours postoperatively once the VAS score exceeded 5, was recorded.
2.8. Statistical analysis
The collected data were coded, tabulated, and statistically analyzed using IBM SPSS statistics (Statistical Package for Social Sciences) software version 22.0, IBM Corp., Chicago, USA, 2013.
Descriptive statistics were done for quantitative data as mean ± SD (standard deviation) for quantitative normally distributed data, while it was done for qualitative data as numbers and percentages. Inferential analyses were done for quantitative variables using independent t-test, while in qualitative data Chi square test and Fisher’s Exact test were used. Log Rank test was used to compare rate of the need to first dose of rescue analgesia. The level of significance was taken at P < 0.050.
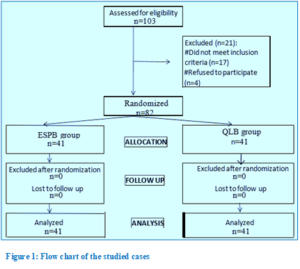
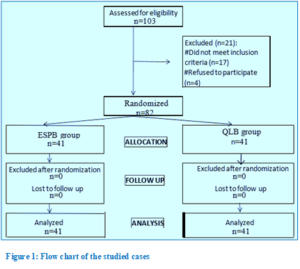
A total of 103 patients were assessed for eligibility and 82 patients were enrolled in the study. Demographic data was equivalent in both groups and there were no significant variations statistically as showed in Table 1, regarding patient age (44.1 ± 8.8 vs 42.2 ± 9.0 years; P = 0.336) for ESPB group and QLB group respectively. There were 27 (65.9%) males vs 14 (34.1%) females in the ESPB group) and 25 (61.0%) males vs 16 (39.0%) females in the QLB group (P = 0.647). Other parameters regarding mean weight, ASA classification, type and duration of surgery, showed no significant differences between the two groups.
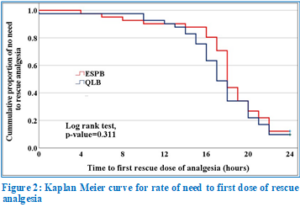
There was no significant difference between the studied groups regarding time to first dose of rescue analgesia needed, as shown in Kaplan Meier curve (Figure 2) and illustrated in Table 2 with P = 0.311.
However, there was significant difference regarding the duration of performing the block, e.g., ESPB was shorter by 14.2 ± 1.6 min in comparison to 14.2 ± 1.6 min for QLB (P < 0.001) as showed in Table 3.
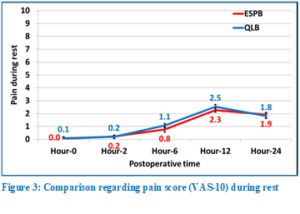
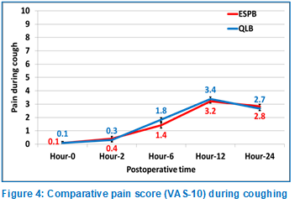
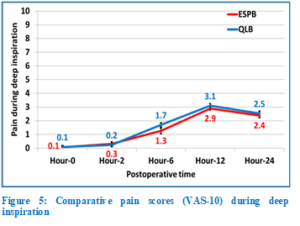
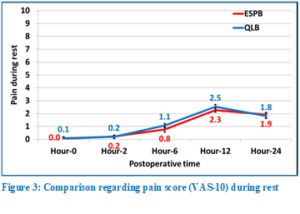
Figures 3, 4 and 5 show that there was no significant difference between the studied groups regarding pain during rest, on coughing, and on deep inspiration, respectively.
Pain is the most common cause for hospital admission following laparoscopic surgery.10 Laparoscopic pain is multifactorial, including visceral, incisional, and referred pain components. Visceral pain is a complex condition that can be caused by mechanical traction, dilation, spasm, inflammation, ischemia, and chemical stimulation.11
Quadratus lumborum block (QLB) has the potential to relieve somatic and visceral pain following laparoscopic surgeries through spread of local anesthetics into the thoracolumbar fascia which has extensive sensory innervation by both A- and C-fiber nociceptors and mechanoreceptors, as well as high-density network of sympathetic fibers to reach to the thoracic paravertebral space.8
ESPB is an effective analgesic method in bariatric surgery and major abdominal surgery when injected from the thoracic vertebral levels. The local anesthetics given during ESPB spreads in the paravertebral space, leading to effective analgesia for somatic and visceral pain. When performed bilaterally ESPB is similar to epidural analgesia.12
Our study measured and compared the postoperative analgesic effect of both blocks in laparoscopic surgeries revealing that there is no significant difference between them regarding first time to rescue analgesia, pain during rest, coughing and deep inspiration; also, the total doses of rescue analgesia were approximately the same with no significant difference, yet there was significant difference between the time to perform the block.
This result agreed with Aygun et al. comparing ESPB and QLB II in laparoscopic cholecystectomy for their impact on postoperative analgesia. The study enrolled 80 patients, divided randomly into two groups, resulting in no significant difference between the two blocks regarding pain numerical rating scales and opioid consumption during first 24 hours postoperative.13
Also, our study was in match with study provided by Ashoor et al. which compared both blocks in laparoscopic sleeve gastrectomy measuring time to first rescue analgesia and the time to perform the block, the duration of anesthesia, the time to first ambulation, the visual analogue scale (VAS) at rest, VAS at movement, the total nalbuphine consumption (mg), and the total requirements of rescue analgesia (ketorolac) over the first 24 hours after surgery. This study had 3 groups; ESPB group, QLB group and a control group. The results showed that ESPB and QLB groups were superior to the control group as regards the time to first rescue analgesia, the total dose of rescue analgesia, and the total nalbuphine consumption (P < 0.001, P < 0.001, P < 0.001, respectively). In the C group, VAS-R and VAS-M readings were higher in the first 18 hours after surgery (P < 0.001, P < 0.001, respectively). In the rest 6 hours of 24 hours after surgery, the QLB group had lower VAS-R and VAS-M readings than the C group (P < 0.001, P < 0.001, respectively).14
Also, both blocks were compared in laparoscopic abdominal surgeries in pediatrics by Taman et al. in 85 patients, receiving either bilateral QLB or ESPB at the level of T8 transverse process with 0.5 mL/kg of 0.25% bupivacaine to achieve adequate postoperative analgesia. FLACC score was used to assess pain score after surgery and the need for rescue opioid analgesia, revealed the preference of QLB for prolonged and effective postoperative analgesia than the ESPB.15
Both quadratus lumborum plane block and erector spinae plane block can control postoperative pain after laparoscopic abdominal surgeries; however, erector spinae plane block can be performed more quickly.
6. Data availability
The numerical data generated during this research is available with the authors, and can be provided on a reasonable request.
7. Conflict of interest
The authors declare no conflicts of interest.
8. Funding
The study utilized the hospital resources only, and no external or industry funding was involved.
9. Ethical approval and trial registration
The protocol of this study was approved by the Ethics Committee of Ain Shams University Hospital (FMASU R 198\2021). The study was prospectively registered clinical trials (www.clinicaltrials.gov); database ID number (NCT05297981) on 4/5/2022.
10. Authors’ contribution
AA, DK: Manuscript editing
AF: Conduct of the study work
FK: Data collection
MA: Manuscript writing
Authors contribution:
- Ahmed Abdelrahman Boeith, Lecturer of Anesthesia, Intensive Care & Pain Management, Faculty of Medicine, Ramses St., Elabbasyia square, Ain Shams University, Cairo, Egypt; Email: Ahmedabdelrahamn2008@med.asu.edu.eg; ORCID: http://orcid.org/0000-0002-3558-3512
- Amr Fouad Hafez, Lecturer of Anesthesia, Intensive Care & Pain Management, Faculty of Medicine, Ramses St., Elabbasyia square, Ain Shams University, Cairo, Egypt; Email: Amr_foud@med.asu.edu.eg; ORCID: http://orcid.org/0000-0002-3198-8491
- Farouk Kamal, Lecturer of Anesthesia, Intensive Care & Pain Management, Faculty of Medicine, Ramses St., Elabbasyia square, Ain Shams University, Cairo, Egypt; Email: Dr.faroukkamal@med.asu.edu.eg; ORCID: http://orcid.org/0000-0001-9688-9518
- Doaa Mohammed Kamal Eldin, Lecturer of Anesthesia, Intensive Care & Pain Management, Faculty of Medicine, Ramses St., Elabbasyia square, Ain Shams University, Cairo, Egypt; Eail: MKjamaluddeen@med.asu.edu.eg; ORCID: http://orcid.org/0009-0003-7807-9644
- Mohamed Abdelwareth, Lecturer of Anesthesia, Intensive Care & Pain Management, Faculty of Medicine, Ramses St., Elabbasyia square, Ain Shams University, Cairo, Egypt; Email: mohamedwareth@med.asu.edu.eg; ORCID: http://orcid.org/0009-0004-8983-1632
ABSTRACT
Background: Postoperative pain after laparoscopic abdominal surgeries can be severe. Despite multimodal analgesia protocols, administration of high doses of opioids is often required hindering early mobilization and discharge of the patient from the day surgery setting and is suboptimal in an Early Recovery after Surgery (ERAS) setting. A prospective randomized clinical comparative double blinded study was conducted at Ain Shams University Hospitals.
We evaluated and compared the analgesic effect of ultrasound-guided erector spinae plane (ESP) block with ultrasound-guided posterior Quadratus Lumborum Block (QLB II) in laparoscopic abdominal surgeries.
Methodology: This study was carried on 82 adult patients undergoing laparoscopic surgeries allocated randomly into 2 equal groups ESPB group and QLB II group. The first time to rescue analgesia was reported as a primary outcome. The secondary outcomes include opioid consumption intraoperative, the time of the performance of the block, visual analogue scale (VAS) at rest, at cough and during deep inspiration and total dose of rescue analgesia.
Results: No significant difference recorded between both groups regarding demographic data, first time to rescue analgesia, opioid consumption intraoperative, VAS score and total dose of postoperative analgesia. However, the duration of block procedure was significantly shorter in ESPB group relative to QLB II group (14.2 ± 1.6 min vs 25.3 ± 2.8 min, P < 0.001).
Abbreviations: ERAS: Early Recovery after Surgery, ESP: erector spinae plane, QLB: Quadratus Lumborum Block, VAS: visual analogue scale
Conclusion: Both quadratus lumborum plane block and erector spinae plane block can control postoperative pain after laparoscopic abdominal surgeries; however, erector spinae plane block provided more time saving during its performance.
Keywords: analgesia; ERAS; Erector spinae block; Laparoscopic; Postoperative pain; Quadratus lumborum block; Ultrasound; VAS score
Citation: Boeith AA, Hafez AF, Kamal F, Kamal Eldin DM, Abdelwareth M. Ultrasound guided quadratus lumborum block versus ultrasound guided erector spinae plane block for postoperative analgesia in laparoscopic abdominal surgeries. Anaesth. pain intensive care 2025;29(2):300-306. DOI: 10.35975/apic.v29i2.2592
Received: May 09, 2024; Reviewed: October 26, 2024; Accepted: January 01, 2025
1. INTRODUCTION
Regional anesthesia role is well established in abdominal surgery, with epidural analgesia being the cornerstone in perioperative analgesia since the early 1900s. However early mobilization, minimally invasive surgical techniques, and pharmacologic venous thromboprophylaxis are now recognized as key components of enhanced recovery after surgery. The search for motor-sparing, less-invasive, safer, and efficacious alternatives to epidural analgesia has been prioritized.1
With the evolution of the ultrasound machine in the operating theatres, the skills of regional anesthesia have been changed from landmark-based techniques to regional blocks administered under direct vision guided by the ultrasound machine.2 The ultrasound-guided Erector Spinae Plane (ESP) block is a novel truncal interfacial regional technique.3
Two techniques of the ESP block for thoracic and abdominal procedures have recently been discussed in literature. The insertion site is at the level of T5 transverse process, spreading between the C7 and T8 segmental levels, or at the level of T7-T9 transverse processes, covering the area between the T6 and T12 segmental levels.4 Quadratus lumborum block (QLB) is a posterior extension of the transversus abdominis plane block (TAP) block. It was first described by Dr Blanco, and it was later modified by Sauter et al. These blocks target both somatic structures covering the anterior abdominal wall, with suggestions of abdominal visceral coverage as well, most commonly using a lateral, posterior, or anterior approach.5
The lateral approach (previously QL1) involves depositing local anesthetic at the lateral border of the QL muscle, anterior to the aponeurosis of the transversus abdominis muscle and within the anterior thoracolumbar fascia. The posterior approach (previously QL2) involves injecting posterior to the QL muscle, in the middle thoracolumbar fascia. The anterior approach (also called the transmuscular QL block) involves injecting anterior to the QL muscle, between it and the psoas major muscle and in the anterior thoracolumbar fascia.6
2. METHODOLOGY
This randomized prospective clinical comparative double blinded study was carried out in Ain shams university hospitals for 1 year on 82 adult patients (by using G power program, setting power at 80%, alpha error at 5%) with American Society of Anesthesiologists (ASA) Physical Status Class I and II, aged between 30 and 60 years, and scheduled for laparoscopic abdominal surgery. Written and informed consent was taken from each patient. Every patient received an explanation to the purpose of the study and had a secret code number to ensure privacy to participant and confidentiality of data.
Patients were randomly allocated into two equal groups:
- Group E (41 patients): Each patient received general anesthesia plus bilateral ESP block.
- Group Q (41 patients): Each patient received general anesthesia plus bilateral posterior QLB.
A computer system was used for randomization by creating a list of number each number referred to one of the two groups. Block randomization was used to ensure equality of the groups. Each number was sealed in an opaque envelope. Then, each patient was asked to choose one of the envelopes and was given to an anesthesiologist who compared it to the computer-generated list and hence assigned to one of the two groups. The patients and the investigators who are responsible for assessing the primary and secondary outcomes were blinded to study group assignment. However, the attending intraoperative anesthesiologists and assessors were not blinded to study group assignment.
Patients included in the study aged 30–60 years, with ASA Physical Status Class I and II, scheduled for laparoscopic abdominal surgery under general anesthesia.
Patients excluded from the study if they showed infection at injection site, allergy to local anesthetics, coagulation disorders, severe obesity, physical or mental diseases which may interfere with the evaluation of pain scores, or kidney failure or liver failure.
All patients were assessed preoperatively, and instructed to fast for 8 hrs. On arrival to the operation theatre, Intravenous access was established, and lactated Ringer solution infused by rate 10 mL/kg. Patients received titration of 0.03 mg/kg midazolam intravenously as sedation. Standard monitors including non-invasive blood pressure, electrocardiogram (ECG), and pulse oximetry (SpO2) and capnography applied to monitor the perioperative hemodynamic parameters. For both groups, general anesthesia induced with IV injection of fentanyl (1 μg/kg) and propofol (2 mg/kg), and then, atracurium (0.5 mg/kg) was injected for endotracheal intubation. Mechanical ventilation was maintained to keep the end-tidal CO2 (EtCO2) values between 34 and 36 mmHg. Anesthesia continued with isoflurane 1%–2% in 100% oxygen. Incremental dose of atracurium (0.1 mg/kg) was given every 30 min or when needed.
After endotracheal intubation and before the start of the surgery, anesthesiologist performed the block techniques and administered the medication. Both blocks were performed under complete aseptic precautions using ultrasound machine.
2.1. In Group Q:
The patient was placed in the lateral decubitus position. After sterilization of the US site, needle entry, and draping, a low frequency curved probe of a transportable Fuji M-Turbo ultrasound system was placed horizontally in the anterior axillary line midway between the subcostal margin and the iliac crest to identify the triple abdominal muscle layers. Then, the probe moved posteriorly to the posterior axillary line until the QL muscle appeared with its attachment to the lateral edge of the transverse process of the L4 vertebral body, the psoas major muscle anteriorly, and the erector spinae muscle posteriorly; this is a well-recognizable pattern of a shamrock sign with three leaves.7 A 22-G, 80-mm needle echogenic needle was inserted in plane relative to the US probe, into the posterior aspect of the QL muscle (between QL and erector spinae muscle); this is known as QLB type 2. Then, 0.5 mL/kg of 0.25% bupivacaine was injected behind the muscle as a bolus dose on both sides.8
2.2. In Group E:
The patient was placed in lateral decubitus position. After sterilization of the US site, needle entry, and draping, a high frequency linear probe of a transportable Fuji M-Turbo ultrasound system was placed on the spinous process at T8 level on the parasagittal plane and then slide 2.5–3 cm laterally to visualize the transverse process and erector spinae muscle. Using the inplane technique, A 22-G, 80-mm needle echogenic needle was inserted between the transverse process and erector spinae muscle. Then 0.5 mL/kg of 0.25% bupivacaine was injected between the muscle and transverse process on both sides.9
Intravenous fentanyl (0.5 µg/kg) was given intraoperatively when any increase in MAP or HR more than 20% of baseline data occurred throughout the procedure. At the end of the surgery, anesthesia discontinued, reversal of muscle relaxation by 0.02 mg/kg atropine and 0.05 mg/kg prostigmine were given.
Patients were assessed in the immediate postoperative period, and then at 2, 6, 12 and at 24 h for the quality of analgesia using Visual Analogue Scale (VAS) score, and VAS more than 5 was managed by paracetamol 10 mg/kg IV every 8 hours and pethidine 50 mg IV as rescue analgesia.
2.4. The outcomes
The primary outcome of the study was the first time to rescue analgesia (recorded within the first 24 hour postoperatively). It was the time from the end of surgery to patient reporting VAS ≥ 5. Pain assessments are conducted by a researcher who was unaware of the grouping.
| Table 1: Comparison regarding demographic characteristics | ||||
| Variables | ESPB
(n = 41) |
QLB
(n = 41) |
P-value | |
| Age (y) | 44.1 ± 8.8 | 42.2 ± 9.0 | ^0.336 | |
| Gender | Male | 27 (65.9%) | 25 (61.0%) | #0.647 |
| Female | 14 (34.1%) | 16 (39.0%) | ||
| Weight (kg) | 95.8 ± 7.3 | 94.9 ± 7.3 | ^0.558 | |
| ASA | I | 23 (56.1%) | 21 (51.2%) | #0.658 |
| II | 18 (43.9%) | 20 (48.8%) | ||
| Surgery type | LCS | 15 (36.6%) | 16 (39.0%) | #0.965 |
| LNF | 13 (31.7%) | 13 (31.7%) | ||
| LSG | 13 (31.7%) | 12 (29.3%) | ||
| Surgery duration (min) | 114.0 ± 5.5 | 113.0 ± 4.9 | ^0.411 | |
| Abbreviations:.LCS: Laparoscopic cholecystectomy. LNF: Laparoscopic Nissen fundoplication. LSG: Laparoscopic sleeve gastrectomy. Data presented as Mean ± SD or n (%). ^Independent t-test. #Chi square test. | ||||
| Table 2: Comparison regarding rescue analgesia | |||||
| Postoperative Analgesia | ESPB
(n=41) |
QLB
(n=41) |
P-value | Relative effect | |
| RR | 95% CI | ||||
| Need to rescue analgesia | 36 (87.8%) | 37 (90.2%) | §0.999 | 1.10 | 0.89–1.36 |
| Doses
• One dose • Two doses |
31 (86.1%) 5 (13.9%) |
29 (78.4%) 8 (21.6%) |
#0.388 |
1.11 |
0.89–1.38 |
| Mean ± SE | 95% CI | ||||
| Time to first dose (h) | 17.3 ± 4.2 | 16.6 ± 4.1 | 0.521 | 0.6 ± 1.0 | -1.3–2.6 |
| Data presented as Mean ± SD. ^Independent t-test. #Chi square test. §Fisher's Exact test. Relative effect: Effect in QLB group relative to that in ESPB group. RR: Relative risk. SE: Standard error. CI: Confidence interval. | |||||
The secondary outcomes included the time spent on the performance of the block, intraoperative opioid consumption, VAS at rest, during cough and during deep inspiration (measured immediately after surgery, and at 2, 6, 12, and 24 hours postoperatively) on a scale of 0-10. Total dose of rescue analgesia (in the first 24 hours postoperatively once the VAS score exceeded 5, was recorded.
2.8. Statistical analysis
The collected data were coded, tabulated, and statistically analyzed using IBM SPSS statistics (Statistical Package for Social Sciences) software version 22.0, IBM Corp., Chicago, USA, 2013.
Descriptive statistics were done for quantitative data as mean ± SD (standard deviation) for quantitative normally distributed data, while it was done for qualitative data as numbers and percentages. Inferential analyses were done for quantitative variables using independent t-test, while in qualitative data Chi square test and Fisher’s Exact test were used. Log Rank test was used to compare rate of the need to first dose of rescue analgesia. The level of significance was taken at P < 0.050.
3. RESULTS
A total of 103 patients were assessed for eligibility and 82 patients were enrolled in the study. Demographic data was equivalent in both groups and there were no significant variations statistically as showed in Table 1, regarding patient age (44.1 ± 8.8 vs 42.2 ± 9.0 years; P = 0.336) for ESPB group and QLB group respectively. There were 27 (65.9%) males vs 14 (34.1%) females in the ESPB group) and 25 (61.0%) males vs 16 (39.0%) females in the QLB group (P = 0.647). Other parameters regarding mean weight, ASA classification, type and duration of surgery, showed no significant differences between the two groups.
| Table 3: Comparison regarding duration of block procedure | |||||
| Measures | ESPB
(n=41) |
QLB
(n=41) |
P-value | Relative effect | |
| Mean ± SE | 95% CI | ||||
| Mean ± SD | 14.2 ± 1.6 | 25.3 ± 2.8 | ^<0.001* | -11.0 ± 0.5 | -12.0–-10.0 |
| Range | 10.0−17.0 | 20.0−30.0 | |||
| ^Independent t-test. *Significant. Relative effect: Effect in QLB group relative to that in ESPB group. SE: Standard error. CI: Confidence interval. | |||||
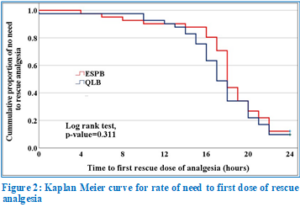
There was no significant difference between the studied groups regarding time to first dose of rescue analgesia needed, as shown in Kaplan Meier curve (Figure 2) and illustrated in Table 2 with P = 0.311.
However, there was significant difference regarding the duration of performing the block, e.g., ESPB was shorter by 14.2 ± 1.6 min in comparison to 14.2 ± 1.6 min for QLB (P < 0.001) as showed in Table 3.
Figures 3, 4 and 5 show that there was no significant difference between the studied groups regarding pain during rest, on coughing, and on deep inspiration, respectively.
4. DISCUSSION
Pain is the most common cause for hospital admission following laparoscopic surgery.10 Laparoscopic pain is multifactorial, including visceral, incisional, and referred pain components. Visceral pain is a complex condition that can be caused by mechanical traction, dilation, spasm, inflammation, ischemia, and chemical stimulation.11
Quadratus lumborum block (QLB) has the potential to relieve somatic and visceral pain following laparoscopic surgeries through spread of local anesthetics into the thoracolumbar fascia which has extensive sensory innervation by both A- and C-fiber nociceptors and mechanoreceptors, as well as high-density network of sympathetic fibers to reach to the thoracic paravertebral space.8
ESPB is an effective analgesic method in bariatric surgery and major abdominal surgery when injected from the thoracic vertebral levels. The local anesthetics given during ESPB spreads in the paravertebral space, leading to effective analgesia for somatic and visceral pain. When performed bilaterally ESPB is similar to epidural analgesia.12
Our study measured and compared the postoperative analgesic effect of both blocks in laparoscopic surgeries revealing that there is no significant difference between them regarding first time to rescue analgesia, pain during rest, coughing and deep inspiration; also, the total doses of rescue analgesia were approximately the same with no significant difference, yet there was significant difference between the time to perform the block.
This result agreed with Aygun et al. comparing ESPB and QLB II in laparoscopic cholecystectomy for their impact on postoperative analgesia. The study enrolled 80 patients, divided randomly into two groups, resulting in no significant difference between the two blocks regarding pain numerical rating scales and opioid consumption during first 24 hours postoperative.13
Also, our study was in match with study provided by Ashoor et al. which compared both blocks in laparoscopic sleeve gastrectomy measuring time to first rescue analgesia and the time to perform the block, the duration of anesthesia, the time to first ambulation, the visual analogue scale (VAS) at rest, VAS at movement, the total nalbuphine consumption (mg), and the total requirements of rescue analgesia (ketorolac) over the first 24 hours after surgery. This study had 3 groups; ESPB group, QLB group and a control group. The results showed that ESPB and QLB groups were superior to the control group as regards the time to first rescue analgesia, the total dose of rescue analgesia, and the total nalbuphine consumption (P < 0.001, P < 0.001, P < 0.001, respectively). In the C group, VAS-R and VAS-M readings were higher in the first 18 hours after surgery (P < 0.001, P < 0.001, respectively). In the rest 6 hours of 24 hours after surgery, the QLB group had lower VAS-R and VAS-M readings than the C group (P < 0.001, P < 0.001, respectively).14
Also, both blocks were compared in laparoscopic abdominal surgeries in pediatrics by Taman et al. in 85 patients, receiving either bilateral QLB or ESPB at the level of T8 transverse process with 0.5 mL/kg of 0.25% bupivacaine to achieve adequate postoperative analgesia. FLACC score was used to assess pain score after surgery and the need for rescue opioid analgesia, revealed the preference of QLB for prolonged and effective postoperative analgesia than the ESPB.15
5. CONCLUSION
Both quadratus lumborum plane block and erector spinae plane block can control postoperative pain after laparoscopic abdominal surgeries; however, erector spinae plane block can be performed more quickly.
6. Data availability
The numerical data generated during this research is available with the authors, and can be provided on a reasonable request.
7. Conflict of interest
The authors declare no conflicts of interest.
8. Funding
The study utilized the hospital resources only, and no external or industry funding was involved.
9. Ethical approval and trial registration
The protocol of this study was approved by the Ethics Committee of Ain Shams University Hospital (FMASU R 198\2021). The study was prospectively registered clinical trials (www.clinicaltrials.gov); database ID number (NCT05297981) on 4/5/2022.
10. Authors’ contribution
AA, DK: Manuscript editing
AF: Conduct of the study work
FK: Data collection
MA: Manuscript writing
11. REFERENCES
- Ljungqvist O, Scott M, Fearon KC. Enhanced recovery after surgery: a review. JAMA Surg. 2017;152(3):292–8. [PubMed] DOI: 1001/jamasurg.2016.4952
- Hebbard P, Fujiwara Y, Shibata Y, Royse C. Ultrasound-guided transversus abdominis plane (TAP) block. Anaesth Intensive Care. 2007;35:616–7. [PubMed]
- Forero M, Adhikary SD, Lopez H, Tsui C, Chin KJ. The erector spinae plane block: a novel analgesic technique in thoracic neuropathic pain. Reg Anesth Pain Med. 2016;41(5):621–7. [PubMed] DOI: 1097/AAP.0000000000000451
- Chin KJ, Adhikary S, Sarwani N, Forero M. The analgesic efficacy of pre-operative bilateral erector spinae plane (ESP) blocks in patients having ventral hernia repair. Anaesthesia. 2017;72(4):452–60. [PubMed] DOI: 1111/anae.13814
- Sauter AR, Ullensvang K, Niemi G, Lorentzen HT, Bendtsen TF, Børglum J, et al. The Shamrock lumbar plexus block: a dose-finding study. Eur J Anaesthesiol. 2015;32:764–70. [PubMed] DOI: 1097/EJA.0000000000000265
- El-Boghdadly K, Elsharkawy H, Short A, Chin KJ. Quadratus lumborum block nomenclature and anatomical considerations. Reg Anesth Pain Med. 2016;41(4):548–9. [PubMed] DOI: 1097/AAP.0000000000000411
- Ueshima H, Otake H, Jui-An L. Ultrasound-guided quadratus lumborum block: an updated review of anatomy and techniques. Biomed Res Int. 2017;2017:2752876. [PubMed] DOI: 1155/2017/2752876
- Aditianingsih D, Pryambodho AN, Tantri AR, et al. A randomized controlled trial on analgesic effect of repeated quadratus lumborum block versus continuous epidural analgesia following laparoscopic nephrectomy. BMC Anesthesiol. 2019;19:221. [PubMed] DOI: 1186/s12871-019-0891-7
- Niraj G, Tariq Z. Continuous erector spinae plane (ESP) analgesia in different open abdominal surgical procedures: a case series. J Anesth Surg. 2018;5(1):57–60. DOI: 15436/2377-1364.18.1853
- Rosero EB, Joshi GP. Hospital readmission after ambulatory laparoscopic cholecystectomy: incidence and predictors. J Surg Res. 2017;219:108–15. [PubMed] DOI: 1016/j.jss.2017.05.071
- Fu H, Fu Y, Xu X, Gao Y. Ultrasound-guided rectus sheath block combined with butorphanol for single-incision laparoscopic cholecystectomy: what is the optimal dose of ropivacaine? J Pain Res. 2020;13:2609–15. [PubMed] DOI: 2147/JPR.S265418
- Restrepo-Garces CE, Chin KJ, Suarez P, Diaz A. Bilateral continuous erector spinae plane block contributes to effective postoperative analgesia after major open abdominal surgery. A A Case Rep. 2017;9(11):319–21. [PubMed] DOI: 1213/XAA.0000000000000605
- Aygun H, Nilgun Ozturk K, Pamukcu AS, Inal A, Kiziloglu I, Thomas DT, et al. Ultrasound guided erector spinae plane block and quadratus lumborum block for postoperative analgesia in laparoscopic cholecystectomy patients. J Clin Anesth. 2020;62:109696. [PubMed] DOI: 1016/j.jclinane.2019.109696
- Ashoor TM, Jalal AS, Said AM, Ali MM, Esmat IM. Ultrasound-guided techniques for postoperative analgesia in patients undergoing laparoscopic sleeve gastrectomy: erector spinae plane block vs quadratus lumborum block. Pain Physician. 2023;26(3):245–56. [PubMed]
- Taman HI, El Said Saber HI, Farid AM, Elawady MM. Bilateral erector spinae plane block vs quadratus lumborum block for pediatric postoperative pain management after laparoscopic abdominal surgery. Anaesth Pain Intensive Care. 2022;26(5):602–7. DOI: 35975/apic.v26i5.2017