Samuel H. Daniel 1, Lydia E. Zakhary 2, Paula M. El-Komos 3
Author affiliations:
Background & objective: Neck pain is one of the common problems due to long office hours and improper posture. While most of the pain originates from the muscles and is usually self-limiting, chronic pain which is resistant to treatment is very common especially with the cervical spondylosis. It is the most common progressive disorder in the aging cervical spine and may produce direct neurological damage or ischemic changes and, thus, lead to spinal cord disturbances.
Cervical facet medial branch radiofrequency ablation (RFA) is a minimal procedure for the pain originating from the cervical facets. The procedure is very safe and needs no hospital stay with a success rate over 80% of the patients. We compared the efficacy in the pain relief between RFA of the medial branch of the cervical facet alone vs combined with superficial cervical plexus block (SCPB).
Methodology: We used Power Analysis and Sample Size Software (PASS 15) (Version 15.0.10) for sample size calculation, setting confidence level at 90%, margin of error + 0.10. A total of 53 patients, seeking treatment for bilateral cervical spondylosis pain were included in the study conducted between March 2024 and June 2024. All of them received RFA on both sides; and after 2 weeks they received superficial cervical plexus block on one side. Numeric pain scale (NPS) was used to assess the pain at 1 and 6 months after the procedure. Patient Global Impression of Change (PGIC) score was also measured. Primary outcome was to measure the efficacy of the standard RFA in managing the cervical facet pain; secondary outcome was to assess any additive value of SCP block.
Results: Neck pain significantly reduced on both sides after radiofrequency ablation of cervical facet medial branch after 1 month and after 6 months (P < 0.001), with no significant added effect of superficial cervical plexus block. PGIC was compared between both sides. Significant improvement was detected in both sides after treatment. However, the difference between the groups was not statistically significant.
Conclusion: Radiofrequency alone can provide sufficient pain relief in patients with chronic neck spondylosis pain with no significant added effect of superficial cervical plexus block.
Keywords: Neck pain, Radiofrequency, Cervical plexus block, Spondylosis, Chronic pain
Citation: Daniel SH, Zakhary LE, El-Komos PM. Comparative study between cervical medial branch radiofrequency ablation versus radiofrequency plus superficial cervical plexus block in treatment of the cervical facet and cervical spondylosis pain. Anaesth. pain intensive care 2025;29(2):325-330. DOI: 10.35975/apic.v29i2.2583
Received: May 09, 2024; Reviewed: October 26, 2024; Accepted: January 01, 2025
Neck pain is one of the common problems in modern life due to long office working hours and the use of the computers and the tablets. While most of the pain originates from the muscles and is usually self-limiting especially with the use of anti-inflammatory medications and muscle spasm relieving medications (like non-steroidal anti-inflammatory drugs and gabapentin derivatives) and the physiotherapy; still the chronic pain resistant to treatment is very common, especially the pain associated with the spondylosis that occurs in the cervical vertebral column.1
Patients with cervical facet arthritis complain of neck pain, headache, and limitations of range of motion (ROM). The pain is described as a dull, aching discomfort in the posterior neck, which sometimes radiates to the shoulder or mid back. Clinical features that often, but not always, include tenderness to palpation over the facet joints or paraspinal muscles, pain with cervical extension or rotation, and absent neurologic or radicular symptoms.2 The cervical facet syndrome may be either traumatic, as due to whiplash injury and dislocations, or degenerative as a result of local spondylosis, or even a part of systemic inflammation as rheumatoid arthritis or gout.3
Cervical spondylosis is the most common progressive disorder in the aging cervical spine. It results from the process of degeneration of the intervertebral discs and facet joints of the cervical spine. Symptoms related to myelopathy and radiculopathy are caused by the formation of osteophytes, which compromise the diameter of the spinal canal. This compromise may also be partially developmental. The developmental process, together with the degenerative process, may cause mechanical pressure on the spinal cord at one or multiple levels, producing direct neurological damage or ischemic changes and, thus, lead to spinal cord disturbances.4
Imaging studies usually are not helpful, with the exception of ruling out other sources of pain, such as fractures or tumors. Signs of cervical spondylosis, narrowing of the intervertebral foramina, osteophytes, and other degenerative changes are equally prevalent in people with and without neck pain. The common findings typical of facet osteoarthritis are:5 joint space narrowing, subchondral sclerosis/bone erosions, osteophytes and/or facet joint edema.
Cervical facet medial branch RF is a minimal procedure, that helps to decrease the pain originating from the cervical facets by making a lesion in the medial branch carrying the pain signal, which is the standard in this situation.6 The procedure is very safe and needs no hospital stay with high success rate. Over 80% of the patients feel improvement in their pain; however, a lot of cases still complain of the pain after the procedure with no decrease in the numeric pain scores.6
Superficial cervical plexus (SCP) block is a traditional block for postoperative analgesia for surgeries of the head and neck as it supplies a lot of nerve branches as, greater auricular (C2–C3), transverse cervical (C2–C3), lesser occipital (C2), supraclavicular nerve (C3–C4), and two posterior roots of spinal nerve; pre-(C2–C3) and post-auricular nerve (C3–C4).7 Deepak et al. published the role of the SCP block in the management of the referred pain originates from the cervical spine and how it helps to decrease the pain.8
In his retrospective study, Joe zako (2024) finds a great role of SCP block for patients suffering from chronic pain from different etiologies when the pain is in area covered by the branches of the plexus especially the transverse cervical nerve.9
We compared the effectiveness in the pain relief between DOIng radiofrequency ablation (RFA) for the medial branch of the cervical facet pain alone or when combined with SCP block in patients suffering from cervical spondylosis and facet arthritis related pain.
It was a one arm prospective interventional study comparing the effectiveness in the pain relief between RFA for the medial branch of the cervical facet pain alone vs using it combined with SCP block. The trial was registered with www.clinicaltrial.gov with the registration number NCT06480175.
A total of 53 patients with neck spondylosis pain, between March 2024 and June 2024, were included in the study. We used Power Analysis and Sample Size Software (PASS 15) (Version 15.0.10) for sample size calculation, setting confidence level at 90%, margin of error + 0.10, and after reviewing previous study results (Niraj and Critchley, 2022), which showed that, about 82% of patients with chronic neck pain reported significant reduction in pain frequency and intensity after 3 months of intervention with intermediate cervical plexus block. Based on these results and after considering 10% attrition rate, a sample size of at least 53 patients with cervical facet and cervical spondylosis pain was considered to be sufficient to achieve study objective.
Patients with neck spondylosis pain were included in our study, with the following criteria: both genders, 30-70 years of age, ASA I, II and III, and MRI based diagnosed with cervical facet arthropathy, without any other pathology such as tumors, inflammation, dislocation or significant disc herniation. All included patients had already received medical treatment including non-steroidal anti-inflammatory drugs (NSAIDs), muscle relaxants with multiple sessions of physiotherapy before the procedure without any significant effect.
Patients excluded were those with neurological disorders, coagulopathy (INR > 1.8 or platelets < 50,000), infection at or near the injection site, presence of pacemaker or defibrillator, known allergy to medications to be used, patients with previous history of radiotherapy, chemotherapy or metastasis, pregnant patients, patients with rheumatological disorders (rheumatoid arthritis, diffuse idiopathic skeletal hyperostosis, psoriatic arthritis), patients with antiphospholipid syndrome, and uncontrolled diabetes (HbA1C > 10).
Study procedure
Patients meeting the inclusion criteria were informed about the study methods, aim, and possible side effect in language they understood; written consent was taken. Medical and past history was taken for any chronic disease, previous operations, hospital admissions, history of neurological or rheumatological diseases or history of malignancy, radiotherapy or chemotherapy.
General physical examination and neurological examination assessed peripheral and central neurological function, motor or sensory affection, neck mobility and peripheral reflexes. Pain assessment was done by using visual analogue scale (VAS) score (0-10). Patients were classified according to severity of pain;
- Mild pain (VAS ≤ 3)
- Moderate pain (VAS 4-7)
- Severe pain (VAS > 7)
MRI cervical spine was done in all patients, together with plain chest X-ray to exclude any other pathology. Complete blood picture and coagulation profile (PT, PTT, INR) was done to exclude coagulopathy.
Patients with confirmed cervical spondylosis, complaining of moderate to severe pain with failed medical treatment were included in our study. All patients received 1 gm 3rd generation antibiotic one hour before the procedure, then were placed in prone position with neck preparation using an iodine-based product and draped in a sterile manner. All of the patients were monitored by ECG, noninvasive blood pressure and pulse oximetry.
Then the ground pad of the radiofrequency machine (Neurotherm NT1100 regenerator) was placed on the back. The entry sites were detected under fluoroscopy; local anesthesia was infiltrated using lidocaine 2% followed by the insertion of the RF cannula (STRYKER 20 G, 9 cm with 1 cm active tip) targeting the medial branches supplying C4- C6 bilaterally. We used one entry site for each side and then the needles were redirected. Confirmation of the appropriate location was done on fluoroscopy in both A-P and lateral views.
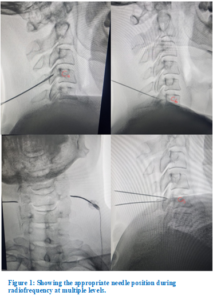
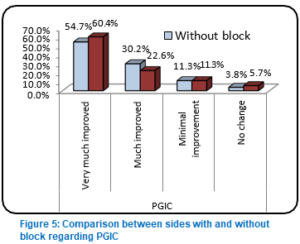
Once targeted, sensory stimulation was done and the patient was asked if he or she felt the same pain which they used to suffer from. Once confirmed with absence of motor response; lidocaine 2% 1 mL was injected and then ablation for 180 sec at 80 degrees was started. A total of 40 mg triamcinolone was injected in 3 levels on each side to decrease the neuritis produced by the thermal lesion (Figure 1).
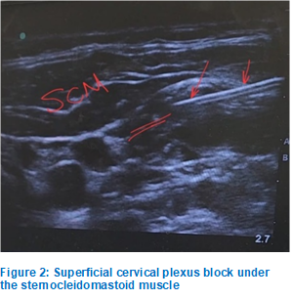
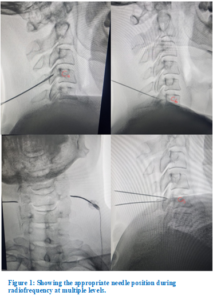
The procedure was done bilaterally. After 2 weeks, patients were readmitted and then we chose one side to inject the SCP with 5 mL of lidocaine 20% plus 40 mg triamcinolone. Injection was randomly made in the right or left side using ultrasound to confirm success. After securing an IV cannula the patients were placed supine looking to the contralateral side. The site of entry was detected using linear high frequency ultrasound probe and 3 mL of lidocaine 2% was injected then a 22G needle was advanced below the sternomastoid muscle edge to reach the target. Another 5 mL of lidocaine 2% plus 40 mg triamcinolone were injected. The side of the block was recorded for each patient (Figure 2).
Comparison was done between both sides to study the effect of adding superficial plexus block to radiofrequency.
The patients were followed up after 1 and 6 months and were asked about the improvement in the numeric pain scale score (NPS) and the ‘Patient Global Impression of Change’ (PGIC) and the side which has better scores. VAS scores were recorded for documentation.
Outcome measurements
Numeric pain scale (NPS) was used to assess the pain at 1 and 6 months after the procedure. PGIC score was also measured. Primary outcome was to measure the efficacy of the standard RFA in managing the cervical facet pain; secondary outcome was to assess any additive value of SCP block.
Statistical analysis
Data were collected, revised, coded and entered to the Statistical Package for Social Sciences (IBM SPSS) (IBM Corp. Released 2020. IBM SPSS Statistics for Windows, Version 27.0. Armonk, NY: IBM Corp). The quantitative data are presented as means, standard deviations, ranges, median and inter-quartile range (IQR). Also, qualitative variables are presented as number and percentages. The comparison between two independent groups with quantitative data and parametric distribution were done by using Independent t-test while with non-parametric distribution were done by using Mann-Whitney test. The comparison between more than two paired groups regarding quantitative data and non-parametric distribution was done by using Friedman test. The confidence interval was set to 95% and the margin of error accepted was set to 5%. So, the P-value was considered significant at the level of < 0.05.
This study included 53 patients with neck spondylosis pain. No patient was excluded following allocation. Age, gender, height, weight, and preoperative diagnosis did not differ significantly differ (Table 1).
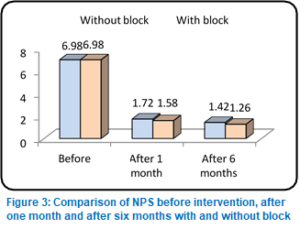
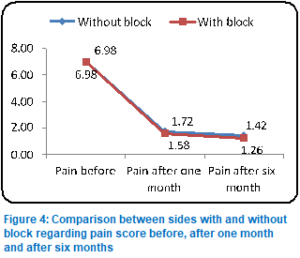
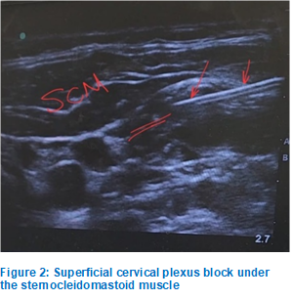
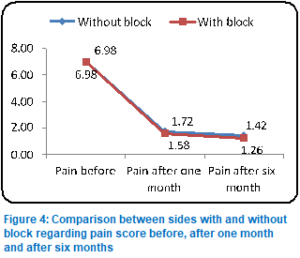
Table 2 presents the comparison of Numeric Pain Scale (NPS) scores before and after treatment in groups with and without a superficial cervical plexus (SCP) block. The paired t-test results indicate a statistically significant reduction in NPS scores after treatment for both sides compared to before treatment, with P < 0.001. Figure 4 depicts graphical presentation of the NRS scores in both groups.
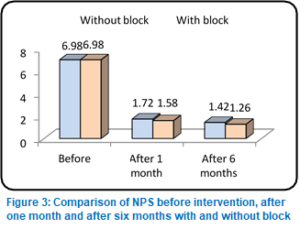
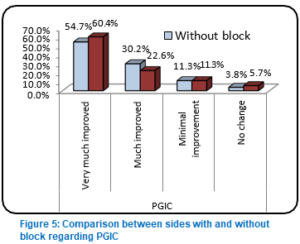
Significant difference in NPS was found in both sides when compared to NPS before the procedure, but when both sides were compared to each other, no significant difference was found. PGIC (Patient Global Impression of Change) was compared between both sides. Significant improvement was detected in both sides after treatment. However, the difference between the groups was not statistically significant (Table 3; Figure 6).
Chronic axial neck pain with or without headache or upper extremity pain is one of the major causes of disability and health care costs. The widely published literature shows that morbidity and chronic disability now account for significant health care burden, with neck pain ranking as number three among the 30 leading diseases and injuries.12
Bogduk and Marsland13 described facet joints as a source of idiopathic neck pain in 1988. Since then, numerous diagnostic accuracy studies, systematic reviews, and guidelines have been published. Multiple discussions have continued to evolve in reference to the diagnosis of facet joint pain and subsequent therapy with either facet joint nerve blocks or radiofrequency neurotomy (RFN).14 Among the therapeutic interventions, radiofrequency has been considered as the standard treatment to provide long-term improvement; however, there has been only one RCT and three observational studies assessed in the previous evaluations.14
Manchikanti et al. showed prevalence and false positive rates of 49.3% and 25.6%, respectively, in chronic neck pain using a chronic pain model.15 They also showed that the duration of relief of at least 80% was 6 days with lidocaine and 12 days with bupivacaine, with a total relief of at least 50% for 31 days and 55 days, respectively. In addition to multiple publications by Manchikanti et al. , a recent randomized controlled trial (RCT) by van Eerd et al. of the comparative value of local anesthetic blocks with RFA in patients with clinically diagnosed cervical facet joint pain showed pain treatment success of 61.1% in both groups, either RFN with a single lesion at 3 months, 55.6% in the denervation group and 51.3% in the bupivacaine alone group at 6-month follow-up with no significant difference among the groups, reinforcing long-term relief of local anesthetic injections16
The main goal of our study was to assess if there is any role of the SCP block in the treatment of the cervical facet and somatic referred cervical pain and if adding it to the RFA can be an additive effect. The results of our study showed that there was no significant difference in the NPS scores (P = 0.509) whether SCP block was done or not. also, the PGIC score showed no statistically significant value (P = 0.821). The improvement in both scores was mainly caused by the RFA of the cervical medial branches with high significance (P < 0.001).
However, Deepak et al case series on 3 patients with neck pain, who received SCP, showed good response and expected a role of SCP in blocking the transmission of the cervical spondylo-degenerative pain signals to the brain.8 Also Joe Zeko and Jordi Perez found that SCP block was helpful in neck pain for different etiologies, whether tumor related or not, especially as it’s an easy and cheap intervention and always worth trying, but they also failed to prove the role of the block in chronic pain management. SCP block may be aimed in the failed cases if the topographical correlation of cutaneous nerve supply of SCP branches and the distribution of pain provided the basis for performing the block.9 Ramamani Mariappan et al. study used the SCP block alone to control the postoperative pain in patients undergoing anterior discectomy operation but without significant noticeable effect.17
Our results showed the effectiveness of the RFA neurotomy on the managing of the cervical facet pain and this conclusion is approved with the meta-analysis done by Laxmaiah Manchikanti et al., which provided level II evidence in managing chronic neck pain.18 Andrea Künzle et al. recently published a study with a new lateral approach using the novel multitined needles with even greater results.19
On the basis of our study, we conclude that radiofrequency alone provided significant pain relief in patients with cervical spondylosis pain, at 1 and 6 months after the procedure, but the superficial cervical plexus block performed with radiofrequency did not add to the pain relief and added no extra benefit.
6. Availability of data
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.
7. Ethical considerations
This study was approved by the research ethics committee at the faculty of medicine, Ain Shams University (FMASU R 119/2024) and registered at www.clinicaltrial.gov with the registration number NCT06480175. Written informed consent was obtained from all patients.
8. Competing interests,
The authors declare that there were no conflicts of interest.
9. Funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
10. Authors contribution
PME: Conduction of the study work
SHD: Manuscript editing, literature search and review
LEZ: Literature search, statistical analysis and review
Author affiliations:
- Samuel H. Daniel, MD, Department of Anesthesia & Intensive Care Medicine , Faculty of Medicine, Ain Shams University, Cairo, Egypt; Email: samuel_7abachi@hotmail.com
- Lydia E. Zakhary, MD, Department of Anesthesia & Intensive Care Medicine , Faculty of Medicine, Ain Shams University, Cairo, Egypt; Email: Lydia_zakhary@med.asu.edu.eg
- Paula M. El-Komos, MD, Department of Anesthesia & Intensive Care Medicine , Faculty of Medicine, Ain Shams University, Cairo, Egypt; Email: paulamicheel@med.asu.edu.eg
ABSTRACT
Background & objective: Neck pain is one of the common problems due to long office hours and improper posture. While most of the pain originates from the muscles and is usually self-limiting, chronic pain which is resistant to treatment is very common especially with the cervical spondylosis. It is the most common progressive disorder in the aging cervical spine and may produce direct neurological damage or ischemic changes and, thus, lead to spinal cord disturbances.
Cervical facet medial branch radiofrequency ablation (RFA) is a minimal procedure for the pain originating from the cervical facets. The procedure is very safe and needs no hospital stay with a success rate over 80% of the patients. We compared the efficacy in the pain relief between RFA of the medial branch of the cervical facet alone vs combined with superficial cervical plexus block (SCPB).
Methodology: We used Power Analysis and Sample Size Software (PASS 15) (Version 15.0.10) for sample size calculation, setting confidence level at 90%, margin of error + 0.10. A total of 53 patients, seeking treatment for bilateral cervical spondylosis pain were included in the study conducted between March 2024 and June 2024. All of them received RFA on both sides; and after 2 weeks they received superficial cervical plexus block on one side. Numeric pain scale (NPS) was used to assess the pain at 1 and 6 months after the procedure. Patient Global Impression of Change (PGIC) score was also measured. Primary outcome was to measure the efficacy of the standard RFA in managing the cervical facet pain; secondary outcome was to assess any additive value of SCP block.
Results: Neck pain significantly reduced on both sides after radiofrequency ablation of cervical facet medial branch after 1 month and after 6 months (P < 0.001), with no significant added effect of superficial cervical plexus block. PGIC was compared between both sides. Significant improvement was detected in both sides after treatment. However, the difference between the groups was not statistically significant.
Conclusion: Radiofrequency alone can provide sufficient pain relief in patients with chronic neck spondylosis pain with no significant added effect of superficial cervical plexus block.
Keywords: Neck pain, Radiofrequency, Cervical plexus block, Spondylosis, Chronic pain
Citation: Daniel SH, Zakhary LE, El-Komos PM. Comparative study between cervical medial branch radiofrequency ablation versus radiofrequency plus superficial cervical plexus block in treatment of the cervical facet and cervical spondylosis pain. Anaesth. pain intensive care 2025;29(2):325-330. DOI: 10.35975/apic.v29i2.2583
Received: May 09, 2024; Reviewed: October 26, 2024; Accepted: January 01, 2025
1. INTRODUCTION
Neck pain is one of the common problems in modern life due to long office working hours and the use of the computers and the tablets. While most of the pain originates from the muscles and is usually self-limiting especially with the use of anti-inflammatory medications and muscle spasm relieving medications (like non-steroidal anti-inflammatory drugs and gabapentin derivatives) and the physiotherapy; still the chronic pain resistant to treatment is very common, especially the pain associated with the spondylosis that occurs in the cervical vertebral column.1
Patients with cervical facet arthritis complain of neck pain, headache, and limitations of range of motion (ROM). The pain is described as a dull, aching discomfort in the posterior neck, which sometimes radiates to the shoulder or mid back. Clinical features that often, but not always, include tenderness to palpation over the facet joints or paraspinal muscles, pain with cervical extension or rotation, and absent neurologic or radicular symptoms.2 The cervical facet syndrome may be either traumatic, as due to whiplash injury and dislocations, or degenerative as a result of local spondylosis, or even a part of systemic inflammation as rheumatoid arthritis or gout.3
Cervical spondylosis is the most common progressive disorder in the aging cervical spine. It results from the process of degeneration of the intervertebral discs and facet joints of the cervical spine. Symptoms related to myelopathy and radiculopathy are caused by the formation of osteophytes, which compromise the diameter of the spinal canal. This compromise may also be partially developmental. The developmental process, together with the degenerative process, may cause mechanical pressure on the spinal cord at one or multiple levels, producing direct neurological damage or ischemic changes and, thus, lead to spinal cord disturbances.4
Imaging studies usually are not helpful, with the exception of ruling out other sources of pain, such as fractures or tumors. Signs of cervical spondylosis, narrowing of the intervertebral foramina, osteophytes, and other degenerative changes are equally prevalent in people with and without neck pain. The common findings typical of facet osteoarthritis are:5 joint space narrowing, subchondral sclerosis/bone erosions, osteophytes and/or facet joint edema.
Cervical facet medial branch RF is a minimal procedure, that helps to decrease the pain originating from the cervical facets by making a lesion in the medial branch carrying the pain signal, which is the standard in this situation.6 The procedure is very safe and needs no hospital stay with high success rate. Over 80% of the patients feel improvement in their pain; however, a lot of cases still complain of the pain after the procedure with no decrease in the numeric pain scores.6
Superficial cervical plexus (SCP) block is a traditional block for postoperative analgesia for surgeries of the head and neck as it supplies a lot of nerve branches as, greater auricular (C2–C3), transverse cervical (C2–C3), lesser occipital (C2), supraclavicular nerve (C3–C4), and two posterior roots of spinal nerve; pre-(C2–C3) and post-auricular nerve (C3–C4).7 Deepak et al. published the role of the SCP block in the management of the referred pain originates from the cervical spine and how it helps to decrease the pain.8
In his retrospective study, Joe zako (2024) finds a great role of SCP block for patients suffering from chronic pain from different etiologies when the pain is in area covered by the branches of the plexus especially the transverse cervical nerve.9
We compared the effectiveness in the pain relief between DOIng radiofrequency ablation (RFA) for the medial branch of the cervical facet pain alone or when combined with SCP block in patients suffering from cervical spondylosis and facet arthritis related pain.
2. METHODOLOGY
It was a one arm prospective interventional study comparing the effectiveness in the pain relief between RFA for the medial branch of the cervical facet pain alone vs using it combined with SCP block. The trial was registered with www.clinicaltrial.gov with the registration number NCT06480175.
A total of 53 patients with neck spondylosis pain, between March 2024 and June 2024, were included in the study. We used Power Analysis and Sample Size Software (PASS 15) (Version 15.0.10) for sample size calculation, setting confidence level at 90%, margin of error + 0.10, and after reviewing previous study results (Niraj and Critchley, 2022), which showed that, about 82% of patients with chronic neck pain reported significant reduction in pain frequency and intensity after 3 months of intervention with intermediate cervical plexus block. Based on these results and after considering 10% attrition rate, a sample size of at least 53 patients with cervical facet and cervical spondylosis pain was considered to be sufficient to achieve study objective.
Patients with neck spondylosis pain were included in our study, with the following criteria: both genders, 30-70 years of age, ASA I, II and III, and MRI based diagnosed with cervical facet arthropathy, without any other pathology such as tumors, inflammation, dislocation or significant disc herniation. All included patients had already received medical treatment including non-steroidal anti-inflammatory drugs (NSAIDs), muscle relaxants with multiple sessions of physiotherapy before the procedure without any significant effect.
Patients excluded were those with neurological disorders, coagulopathy (INR > 1.8 or platelets < 50,000), infection at or near the injection site, presence of pacemaker or defibrillator, known allergy to medications to be used, patients with previous history of radiotherapy, chemotherapy or metastasis, pregnant patients, patients with rheumatological disorders (rheumatoid arthritis, diffuse idiopathic skeletal hyperostosis, psoriatic arthritis), patients with antiphospholipid syndrome, and uncontrolled diabetes (HbA1C > 10).
Study procedure
Patients meeting the inclusion criteria were informed about the study methods, aim, and possible side effect in language they understood; written consent was taken. Medical and past history was taken for any chronic disease, previous operations, hospital admissions, history of neurological or rheumatological diseases or history of malignancy, radiotherapy or chemotherapy.
General physical examination and neurological examination assessed peripheral and central neurological function, motor or sensory affection, neck mobility and peripheral reflexes. Pain assessment was done by using visual analogue scale (VAS) score (0-10). Patients were classified according to severity of pain;
- Mild pain (VAS ≤ 3)
- Moderate pain (VAS 4-7)
- Severe pain (VAS > 7)
MRI cervical spine was done in all patients, together with plain chest X-ray to exclude any other pathology. Complete blood picture and coagulation profile (PT, PTT, INR) was done to exclude coagulopathy.
Patients with confirmed cervical spondylosis, complaining of moderate to severe pain with failed medical treatment were included in our study. All patients received 1 gm 3rd generation antibiotic one hour before the procedure, then were placed in prone position with neck preparation using an iodine-based product and draped in a sterile manner. All of the patients were monitored by ECG, noninvasive blood pressure and pulse oximetry.
Then the ground pad of the radiofrequency machine (Neurotherm NT1100 regenerator) was placed on the back. The entry sites were detected under fluoroscopy; local anesthesia was infiltrated using lidocaine 2% followed by the insertion of the RF cannula (STRYKER 20 G, 9 cm with 1 cm active tip) targeting the medial branches supplying C4- C6 bilaterally. We used one entry site for each side and then the needles were redirected. Confirmation of the appropriate location was done on fluoroscopy in both A-P and lateral views.
Once targeted, sensory stimulation was done and the patient was asked if he or she felt the same pain which they used to suffer from. Once confirmed with absence of motor response; lidocaine 2% 1 mL was injected and then ablation for 180 sec at 80 degrees was started. A total of 40 mg triamcinolone was injected in 3 levels on each side to decrease the neuritis produced by the thermal lesion (Figure 1).
The procedure was done bilaterally. After 2 weeks, patients were readmitted and then we chose one side to inject the SCP with 5 mL of lidocaine 20% plus 40 mg triamcinolone. Injection was randomly made in the right or left side using ultrasound to confirm success. After securing an IV cannula the patients were placed supine looking to the contralateral side. The site of entry was detected using linear high frequency ultrasound probe and 3 mL of lidocaine 2% was injected then a 22G needle was advanced below the sternomastoid muscle edge to reach the target. Another 5 mL of lidocaine 2% plus 40 mg triamcinolone were injected. The side of the block was recorded for each patient (Figure 2).
Comparison was done between both sides to study the effect of adding superficial plexus block to radiofrequency.
The patients were followed up after 1 and 6 months and were asked about the improvement in the numeric pain scale score (NPS) and the ‘Patient Global Impression of Change’ (PGIC) and the side which has better scores. VAS scores were recorded for documentation.
Outcome measurements
Numeric pain scale (NPS) was used to assess the pain at 1 and 6 months after the procedure. PGIC score was also measured. Primary outcome was to measure the efficacy of the standard RFA in managing the cervical facet pain; secondary outcome was to assess any additive value of SCP block.
Statistical analysis
Data were collected, revised, coded and entered to the Statistical Package for Social Sciences (IBM SPSS) (IBM Corp. Released 2020. IBM SPSS Statistics for Windows, Version 27.0. Armonk, NY: IBM Corp). The quantitative data are presented as means, standard deviations, ranges, median and inter-quartile range (IQR). Also, qualitative variables are presented as number and percentages. The comparison between two independent groups with quantitative data and parametric distribution were done by using Independent t-test while with non-parametric distribution were done by using Mann-Whitney test. The comparison between more than two paired groups regarding quantitative data and non-parametric distribution was done by using Friedman test. The confidence interval was set to 95% and the margin of error accepted was set to 5%. So, the P-value was considered significant at the level of < 0.05.
| Table 1: Demographic data and characteristics of the patients (n=53) | ||
| Parameter | Count | Range |
| Age (y) | 60.40 ± 4.19 | 53–68 |
| Gender | ||
| · Females | 29 (54.7) | |
| · Males | 24 (45.3) | |
| BMI | 30.23 ± 1.95 | 27–34 |
| MABP | 80.60 ± 3.80 | 74–86 |
| Data presented as mean ± SD or n (%) | ||
3. RESULTS
This study included 53 patients with neck spondylosis pain. No patient was excluded following allocation. Age, gender, height, weight, and preoperative diagnosis did not differ significantly differ (Table 1).
Table 2 presents the comparison of Numeric Pain Scale (NPS) scores before and after treatment in groups with and without a superficial cervical plexus (SCP) block. The paired t-test results indicate a statistically significant reduction in NPS scores after treatment for both sides compared to before treatment, with P < 0.001. Figure 4 depicts graphical presentation of the NRS scores in both groups.
Significant difference in NPS was found in both sides when compared to NPS before the procedure, but when both sides were compared to each other, no significant difference was found. PGIC (Patient Global Impression of Change) was compared between both sides. Significant improvement was detected in both sides after treatment. However, the difference between the groups was not statistically significant (Table 3; Figure 6).
| Table 2: Comparison regarding pain scores before, after one and six months of interventions | |||||
| Time | Without block
(n=53) |
With block
(n=53) |
Test value | P-value | |
| Pain before | Mean ± SD | 6.98 ± 0.54 | 6.98 ± 0.54 | 0.000 | 1.000 |
| Median (IQR) | 7 (7–7) | 7 (7–7) | |||
| Range | 6–8 | 6–8 | |||
| Pain after one month | Mean ± SD | 1.72 ± 1.60 | 1.58 ± 1.68 | -0.660 | 0.509 |
| Median (IQR) | 1 (1–3) | 1 (0–2) | |||
| Range | 0–7 | 0–7 | |||
| Pain after six months | Mean ± SD | 1.42 ± 1.38 | 1.26 ± 1.44 | -1.117 | 0.264 |
| Median (IQR) | 1 (0–2) | 1 (0–1) | |||
| Range | 0–7 | 0–6 | |||
| P > 0.05: Non significant; P < 0.05: Significant; P < 0.01: Highly significant; ≠: Mann-Whitney test | |||||
| Table 3: Comparison between sides with and without block regarding PGIC | ||||
| Patient Global Impression of Change | Without block
(n=53) |
With block
(n=53) |
Test value | P-value |
| Very much improved | 29 (54.7%) | 32 (60.4%) | 0.919* | 0.821 |
| Much improved | 16 (30.2%) | 12 (22.6%) | ||
| Minimal improvement | 6 (11.3%) | 6 (11.3%) | ||
| No change | 2 (3.8%) | 3 (5.7%) | ||
| Data presented as n (%); P < 0.05 considered as significant; *: Chi-square test | ||||
4. DISCUSSION
Chronic axial neck pain with or without headache or upper extremity pain is one of the major causes of disability and health care costs. The widely published literature shows that morbidity and chronic disability now account for significant health care burden, with neck pain ranking as number three among the 30 leading diseases and injuries.12
Bogduk and Marsland13 described facet joints as a source of idiopathic neck pain in 1988. Since then, numerous diagnostic accuracy studies, systematic reviews, and guidelines have been published. Multiple discussions have continued to evolve in reference to the diagnosis of facet joint pain and subsequent therapy with either facet joint nerve blocks or radiofrequency neurotomy (RFN).14 Among the therapeutic interventions, radiofrequency has been considered as the standard treatment to provide long-term improvement; however, there has been only one RCT and three observational studies assessed in the previous evaluations.14
Manchikanti et al. showed prevalence and false positive rates of 49.3% and 25.6%, respectively, in chronic neck pain using a chronic pain model.15 They also showed that the duration of relief of at least 80% was 6 days with lidocaine and 12 days with bupivacaine, with a total relief of at least 50% for 31 days and 55 days, respectively. In addition to multiple publications by Manchikanti et al. , a recent randomized controlled trial (RCT) by van Eerd et al. of the comparative value of local anesthetic blocks with RFA in patients with clinically diagnosed cervical facet joint pain showed pain treatment success of 61.1% in both groups, either RFN with a single lesion at 3 months, 55.6% in the denervation group and 51.3% in the bupivacaine alone group at 6-month follow-up with no significant difference among the groups, reinforcing long-term relief of local anesthetic injections16
The main goal of our study was to assess if there is any role of the SCP block in the treatment of the cervical facet and somatic referred cervical pain and if adding it to the RFA can be an additive effect. The results of our study showed that there was no significant difference in the NPS scores (P = 0.509) whether SCP block was done or not. also, the PGIC score showed no statistically significant value (P = 0.821). The improvement in both scores was mainly caused by the RFA of the cervical medial branches with high significance (P < 0.001).
However, Deepak et al case series on 3 patients with neck pain, who received SCP, showed good response and expected a role of SCP in blocking the transmission of the cervical spondylo-degenerative pain signals to the brain.8 Also Joe Zeko and Jordi Perez found that SCP block was helpful in neck pain for different etiologies, whether tumor related or not, especially as it’s an easy and cheap intervention and always worth trying, but they also failed to prove the role of the block in chronic pain management. SCP block may be aimed in the failed cases if the topographical correlation of cutaneous nerve supply of SCP branches and the distribution of pain provided the basis for performing the block.9 Ramamani Mariappan et al. study used the SCP block alone to control the postoperative pain in patients undergoing anterior discectomy operation but without significant noticeable effect.17
Our results showed the effectiveness of the RFA neurotomy on the managing of the cervical facet pain and this conclusion is approved with the meta-analysis done by Laxmaiah Manchikanti et al., which provided level II evidence in managing chronic neck pain.18 Andrea Künzle et al. recently published a study with a new lateral approach using the novel multitined needles with even greater results.19
5. CONCLUSION
On the basis of our study, we conclude that radiofrequency alone provided significant pain relief in patients with cervical spondylosis pain, at 1 and 6 months after the procedure, but the superficial cervical plexus block performed with radiofrequency did not add to the pain relief and added no extra benefit.
6. Availability of data
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.
7. Ethical considerations
This study was approved by the research ethics committee at the faculty of medicine, Ain Shams University (FMASU R 119/2024) and registered at www.clinicaltrial.gov with the registration number NCT06480175. Written informed consent was obtained from all patients.
8. Competing interests,
The authors declare that there were no conflicts of interest.
9. Funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
10. Authors contribution
PME: Conduction of the study work
SHD: Manuscript editing, literature search and review
LEZ: Literature search, statistical analysis and review
10. REFERENCES
- Berger AA, Liu Y, Mosel L, Champagne KA, Ruoff MT, Cornett EM, et al. Efficacy of dry needling and acupuncture in the treatment of neck pain. Anesth Pain Med. 2021;11(2):e113627. [PubMed] DOI: 5812/aapm.113627
- Yoo YM, Kim KH. Facet joint disorders: from diagnosis to treatment. Korean J Pain. 2024;37(1):3-12. [PubMed] DOI: 3344/kjp.23228
- Bogduk N, Yoganandan N. Biomechanics of the cervical spine part 3: minor injuries. Clin Biomech. 2001;16(4):267-75. [PubMed] DOI: 1016/s0268-0033(01)00003-1
- Shedid D, Benzel EC. Cervical spondylosis anatomy: pathophysiology and biomechanics. Neurosurgery. 2007;60(1 Suppl 1):S7-13. [PubMed] DOI: 1227/01.NEU.0000215430.86569.C4
- Windsor RE, Nagula D, Storm S, Overton A, Jahnke S. Electrical stimulation induced cervical medial branch referral patterns. Pain Physician. 2003;6(4):411-8. [PubMed]
- Burnham T, Conger A, Salazar F, Petersen R, Kendall R, Cunningham S, et al. Effectiveness of cervical medial branch radiofrequency ablation for chronic facet joint syndrome in patients selected by a practical medial branch block paradigm. Pain Med. 2020;21(10):2071-6. [PubMed] DOI: 1093/pm/pnz358
- Herring AA, Stone MB, Frenkel O, Chipman A, Nagdev AD. Ultrasound-guided superficial cervical plexus block for anesthesia and analgesia in emergency care settings. Am J Emerg Med. 2012;30(7):1263-7. [PubMed] DOI: 1016/j.ajem.2011.06.023
- Thapa D, Ahuja V, Dhiman D. Role of superficial cervical plexus block in somatic referred cervical spine pain. Indian J Anaesth. 2017;61(12):1012-4. [PubMed] DOI: 4103/ija.IJA_196_17
- Zako J, Perez J. Unlocking the potential of the superficial cervical plexus block in chronic pain management: a narrative review and single-center, retrospective case series. J Clin Med. 2024;13(21):6310. [PubMed] DOI: 3390/jcm13216310
- Greengrass RA, Narouze S, Bendtsen TF, Hadzic A. Cervical plexus and greater occipital nerve blocks: controversies and technique update. Reg Anesth Pain Med. 2019;44(6):623-6. [PubMed] DOI: 1136/rapm-2018-100261
- Rampakakis E, Ste-Marie PA, Sampalis JS, Karellis A, Shir Y, Fitzcharles MA. Real-life assessment of the validity of patient global impression of change in fibromyalgia. RMD Open. 2015;1(1):e000146. [PubMed] DOI: 1136/rmdopen-2015-000146
- Manchikanti L, Centeno CJ, Atluri S, Albers SL, Shapiro S, Malanga GA, et al. Bone marrow concentrate therapy in musculoskeletal disorders: evidence-based policy position statement of American Society of Interventional Pain Physicians (ASIPP). Pain Physician. 2020;23(2):E85-E131. [PubMed]
- Bogduk N, Marsland A. The cervical zygapophysial joints as a source of neck pain. Spine (Phila Pa 1976). 1988;13(6):610-7. [PubMed]
- Manchikanti L, Kaye AD, Soin A, Albers SL, Beall D, Latchaw R, et al. Comprehensive evidence-based guidelines for facet joint interventions in the management of chronic spinal pain: American Society of Interventional Pain Physicians (ASIPP) guidelines facet joint interventions 2020 guidelines. Pain Physician. 2020;23(3 Suppl):S1-S127. [PubMed]
- Manchikanti L, Kosanovic R, Cash KA, Pampati V, Soin A, Kaye AD, et al. Assessment of prevalence of cervical facet joint pain with diagnostic cervical medial branch blocks: analysis based on chronic pain model. Pain Physician. 2020;23(6):531-40. [PubMed]
- van Eerd M, de Meij N, Kessels A, Patijn J, Weber W, Wintraecken V, et al. Efficacy and long-term effect of radiofrequency denervation in patients with clinically diagnosed cervical facet joint pain: a double-blind randomized controlled trial. Spine (Phila Pa 1976). 2021;46(5):285-93. [PubMed] DOI: 1097/BRS.0000000000003799
- Mariappan R, Mehta J, Massicotte E, Nagappa M, Manninen P, Venkatraghavan L. Effect of superficial cervical plexus block on postoperative quality of recovery after anterior cervical discectomy and fusion: a randomized controlled trial. Can J Anaesth. 2015;62(8):883-90. [PubMed] DOI: 1007/s12630-015-0382-3
- Manchikanti L, Knezevic NN, Knezevic E, Abdi S, Sanapati MR, Soin A, et al. Systematic review and meta-analysis of the effectiveness of radiofrequency neurotomy in managing chronic neck pain. Pain Ther. 2023;12(1):19-66. [PubMed] DOI: 1007/s40122-022-00455-0
- Künzle A, van Kuijk SMJ, Koetsier E. Efficacy of cervical facet joint radiofrequency ablation using a multitined cannula: a technical note and observational study. Pain Physician. 2023;26(4):E353-E361. [PubMed]