Anwar ul Huda1, Asim Arif2, Zohaib Asim3
Author affiliations:
Background & Objective: Emergence delirium (ED) is a known complication characterized by altered mental state that occurs after general anesthesia, which might lead to involuntary agitation in the children. We did this prospective cross-sectional study to find the incidence of emergence delirium after general anesthesia in children at a tertiary care hospital. This study was conducted at Security Forces Hospital, Riyadh, Kingdom of Saudi Arabia
Methodology: We included 96 children, aged 2-12 y, who underwent general anesthesia for surgery. Emergence agitation was scored by using a standardized scoring system named Pediatric Anesthesia Emergence Delirium (PAED) score at the time of extubation and at every 15 min until discharge from PACU. We report the incidence of emergence delirium as numbers and percentages.
Results: A total of 96 children were included in the study. The median PAED score of children was 8 (5-12). The incidence of postoperative ED in pediatric patients was 38.5% (37 cases). The incidence of emergence delirium was higher in younger children with median age 56 (45-70.5) months as compared to children who were 63 (35-80) months old.
Conclusion: We found an incidence of 38.5% emergence delirium after general anesthesia in children at our hospital.
Abbreviations: ED - Emergence delirium; GA - General anesthesia; PAED - Pediatric Anesthesia Emergence Delirium; PACU - Post-anesthesia Care Unit
Keywords: Emergence Delirium, PAED Score, General Anesthesia, PACU
Citation: Huda AU, Arif A, Asim Z. Incidence and features of emergence delirium in children after general anesthesia in the Middle East population. Anaesth. pain intensive care 2024;28(2):310−314; DOI: 10.35975/apic.v28i2.2439
Received: September 13, 2023; Revised: February 04, 2024; Accepted: February 21, 2024
Emergence delirium (ED) is an altered state of consciousness that usually occurs within 45 min after cessation of anesthesia. It typically presents as disorientation, averted eyes or staring, psychomotor agitation and non-purposeful, resistive movements like pulling, kicking or flailing.1,2 ED can result in potential risk of bodily harm to patient or healthcare staffs, prolonged PACU (post-anesthesia care unit) stay and postoperative maladaptive changes including temper tantrums, attention seeking, sleep alterations and bed wetting in children.2
The objective of this study is to find out the incidence of postoperative emergence delirium in patients undergoing general anesthesia for a procedure in a tertiary care hospital of a middle east country.
Risk factors for ED include preoperative anxiety and confusion, psychological immaturity and use of various medications peri-operatively.2,3 Various pharmacological interventions in peri-operative period have been used in literature to prevent ED which include use of propofol, fentanyl, ketamine, clonidine, midazolam and dexmedetomidine etc.4
The incidence of ED varies by age of patient, anesthesia technique, type of surgeries, pain and also by choice of tool to diagnose ED. There is wide variation in the incidence of ED in scientific literature ranging from 5%.5 to 27.3%.6,7 It occurs two to three more commonly in children as compared to adults. Scientific literature suggests the incidence of ED in the range between 20 -80% in pediatric anesthesia practice.8 Cultural differences can have significant effect on preoperative anxiety and hence postoperative complications like ED.
Institutional ethical committee approval was taken. Patients aged between 2 and 12 y, ASA PS class I to III, scheduled to undergo general anesthesia for a surgical procedure, were included in the study. Written informed consent for study was obtained from the patients’ parents or guardians. We excluded children with developmental delays, neurological disease, and those who had undergone previous surgery.
Children were pre-medicated with oral midazolam (0.5 mg/kg) in the preoperative area. On arrival to operating room, standard monitoring, including pulse oximetry, electrocardiography, and non-invasive arterial pressure, was performed prior to induction of anesthesia. Baseline
heart rates, systolic and diastolic blood pressures, and mean arterial pressures were recorded. General anesthesia was administered by the primary anesthetist.
At the end of the operation, all patients were transferred to PACU for routine monitoring. Emergence agitation was scored by using a standardized scoring system named ‘Pediatric Anesthesia Emergence Delirium’ (PAED) score at the time of extubation and at every 15 min until discharge from PACU to the ward. PAED score is considered a reliable and accurate tool to diagnose ED in pediatric patients. This scale consists of five items reflecting consciousness, cognition, emotion and psychomotor behaviors of pediatric patients.10
Regarding the sample size, the expected incidence of ED will be taken as 53% from a previous study.11 To estimate the incidence with a precision of 10%, 95% CI, 96 children undergoing general anesthesia for a procedure will be needed.
We entered and analyzed all study data in SPSS version 25. We reported incidence of ED as number and percentages.
We included a total of 96 children in the study. All variable data were found to have a non-normal distribution. The median age of children in the study was 59 (IQR: 43-76) months. Among 96 children, 30 (31.3%) were females vs 66 (68.8%) males. Sixty (62.5%) patients underwent day care surgery. The distribution of children by surgical specialties is demonstrated in graph I. Twenty-five (26%) children underwent adenotonsillectomy followed by dental rehabilitation 23 (24%), hernia repair 15 (15.6%), orchidopexy 8 (8.3%), EUA ENT 6 (6.3%), circumcision 4 (4.2%), eye surgery 4 (4.2%) and grommet 3 (3.1%). Among 96 patients, 2 were asthmatic, 2 had renal disease and 1 had hearing problems. No patient had any adverse event in the perioperative period.
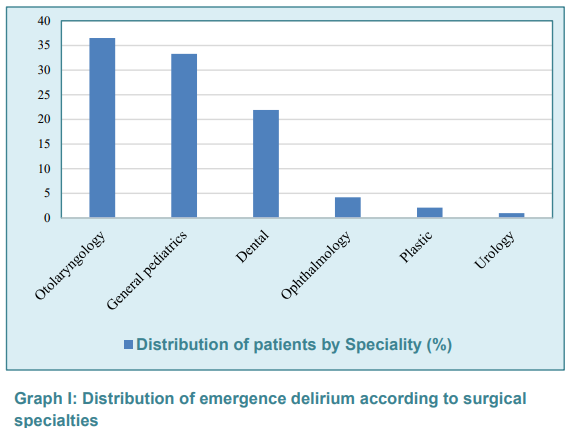
The median emergence delirium score of children was 8 (5-12). The incidence of postoperative ED in pediatric patients was 38.5% (37 cases). Patients with emergence delirium were younger with median age 56 (45-70.5) months compared to 63 (35-80) months in children without emergence delirium. Sixty five percent of children with emergence delirium were male vs 71.1% in children without emergence delirium. Fifty four percent of children with emergence delirium underwent surgery as day care while 67.7% in children without emergence delirium. Seventy percent of children with emergence delirium underwent ENT and dental surgeries vs 50.8% in children without emergence delirium.
Our study showed an incidence of postoperative emergence delirium as 38.5%. This is consistent with findings in the study by Redoque et al who reported an incidence ranging from 20-80%.12 Zainab et al reported a higher incidence of 51.6% in their study on children undergoing dental surgery.13 Pieters et al demonstrated an incidence of ED as 53% that is also higher than our study.14 There could be different explanations for these varied incidences in different studies. Several measuring tools have been developed previously to find out the incidence of ED. Additionally, different studies have also used different criteria to label ED. Some of these scales include Cravero scale, Watcha scale and PAED score etc. Watcha scale is considered a user-friendly tool to detect delirium although PAED score is used to determine its degree.14-17 PAED score has been regarded as gold standard to assess ED previously, but it has been modified by Locatelli et al.18 who focused only on first 3 criteria to increase its specificity.
In our study, patients with ED were relatively younger compared to children without ED. Redoque et al.12 also showed that incidence of ED is 3 to 8 times greater in children less than 5 years of age. In another study by Aono et al, ED occurs more frequently in preschool children.19 Patel et al demonstrated that ED is more common in preschool aged children than adults with an overall incidence 12-13% in children.20
In our study, 64.8% of children with emergence delirium were male vs 71.1% in children without emergence delirium. Also, the overall percentage of male children in our study was higher as 68.8%. Although, Munk et al demonstrated a positive correlation of male gender to the occurrence of ED in adult patients.21 Another observational study by Houben et al reported a higher incidence of ED in male pediatric patients after adenoidectomy.22
Our study results showed that 70% of children with ED underwent ENT and dental surgeries compared to 50.8% in children without ED. Lee et al also reported a positive association of ED with oral, ophthalmological and ENT surgeries.23 Vopel-Lewis et al found a higher incidence of ED in children who underwent ENT surgeries (26%, relative risk = 1.69, P = 0.004).24 Dahmani et al also described a higher incidence of ED in patients who underwent ENT and ophthalmologic surgeries.4
This is the only study on pediatric delirium incidence in Saudi population. But there are a few limitations in our study. It is a single-center study. We had a relatively smaller sample size. We recommend further research on this topic with larger sample size.
We found an incidence of 38.5% of emergence delirium after general anesthesia in children at a hospital setting in a Middle East country.
7. Data availability
The numerical data generated during this research is available with the authors.
8. Acknowledgement
We gratefully thank Faculty of Medicine
9. Conflict of interest
The study utilized the hospital resources only, and no external or industry funding was involved.
10. Authors’ contribution
AUH: Original concept, Scientific literature search, Data collection, Data analysis, Manuscript writing, Editing, Final Approval
AA: Data collection, Manuscript writing, Editing, Final Approval
ZS: Scientific literature search, Manuscript writing, Editing, Final Approval
Author affiliations:
- Anwar ul Huda, Consultant, Department of Anesthesia, Security Forces Hospital Program, Malaz, Riyadh, Kingdom of Saudi Arabia: E-mail: hudaanwar90@yahoo.com
- Asim Arif, Registrar, Department of Anesthesia, Security Forces Hospital Program, Malaz, Riyadh, Kingdom of Saudi Arabia; E-mail: Asimarif75@yahoo.com
- Zohaib Asim, Medical Student, Al Faisal University, Riyadh, Kingdom of Saudi Arabia; E-mail: zasim@alfaisal.edu
ABSTRACT
Background & Objective: Emergence delirium (ED) is a known complication characterized by altered mental state that occurs after general anesthesia, which might lead to involuntary agitation in the children. We did this prospective cross-sectional study to find the incidence of emergence delirium after general anesthesia in children at a tertiary care hospital. This study was conducted at Security Forces Hospital, Riyadh, Kingdom of Saudi Arabia
Methodology: We included 96 children, aged 2-12 y, who underwent general anesthesia for surgery. Emergence agitation was scored by using a standardized scoring system named Pediatric Anesthesia Emergence Delirium (PAED) score at the time of extubation and at every 15 min until discharge from PACU. We report the incidence of emergence delirium as numbers and percentages.
Results: A total of 96 children were included in the study. The median PAED score of children was 8 (5-12). The incidence of postoperative ED in pediatric patients was 38.5% (37 cases). The incidence of emergence delirium was higher in younger children with median age 56 (45-70.5) months as compared to children who were 63 (35-80) months old.
Conclusion: We found an incidence of 38.5% emergence delirium after general anesthesia in children at our hospital.
Abbreviations: ED - Emergence delirium; GA - General anesthesia; PAED - Pediatric Anesthesia Emergence Delirium; PACU - Post-anesthesia Care Unit
Keywords: Emergence Delirium, PAED Score, General Anesthesia, PACU
Citation: Huda AU, Arif A, Asim Z. Incidence and features of emergence delirium in children after general anesthesia in the Middle East population. Anaesth. pain intensive care 2024;28(2):310−314; DOI: 10.35975/apic.v28i2.2439
Received: September 13, 2023; Revised: February 04, 2024; Accepted: February 21, 2024
1. INTRODUCTION
Emergence delirium (ED) is an altered state of consciousness that usually occurs within 45 min after cessation of anesthesia. It typically presents as disorientation, averted eyes or staring, psychomotor agitation and non-purposeful, resistive movements like pulling, kicking or flailing.1,2 ED can result in potential risk of bodily harm to patient or healthcare staffs, prolonged PACU (post-anesthesia care unit) stay and postoperative maladaptive changes including temper tantrums, attention seeking, sleep alterations and bed wetting in children.2
The objective of this study is to find out the incidence of postoperative emergence delirium in patients undergoing general anesthesia for a procedure in a tertiary care hospital of a middle east country.
Risk factors for ED include preoperative anxiety and confusion, psychological immaturity and use of various medications peri-operatively.2,3 Various pharmacological interventions in peri-operative period have been used in literature to prevent ED which include use of propofol, fentanyl, ketamine, clonidine, midazolam and dexmedetomidine etc.4
The incidence of ED varies by age of patient, anesthesia technique, type of surgeries, pain and also by choice of tool to diagnose ED. There is wide variation in the incidence of ED in scientific literature ranging from 5%.5 to 27.3%.6,7 It occurs two to three more commonly in children as compared to adults. Scientific literature suggests the incidence of ED in the range between 20 -80% in pediatric anesthesia practice.8 Cultural differences can have significant effect on preoperative anxiety and hence postoperative complications like ED.
2. METHODOLOGY
Institutional ethical committee approval was taken. Patients aged between 2 and 12 y, ASA PS class I to III, scheduled to undergo general anesthesia for a surgical procedure, were included in the study. Written informed consent for study was obtained from the patients’ parents or guardians. We excluded children with developmental delays, neurological disease, and those who had undergone previous surgery.
Children were pre-medicated with oral midazolam (0.5 mg/kg) in the preoperative area. On arrival to operating room, standard monitoring, including pulse oximetry, electrocardiography, and non-invasive arterial pressure, was performed prior to induction of anesthesia. Baseline
heart rates, systolic and diastolic blood pressures, and mean arterial pressures were recorded. General anesthesia was administered by the primary anesthetist.
At the end of the operation, all patients were transferred to PACU for routine monitoring. Emergence agitation was scored by using a standardized scoring system named ‘Pediatric Anesthesia Emergence Delirium’ (PAED) score at the time of extubation and at every 15 min until discharge from PACU to the ward. PAED score is considered a reliable and accurate tool to diagnose ED in pediatric patients. This scale consists of five items reflecting consciousness, cognition, emotion and psychomotor behaviors of pediatric patients.10
Regarding the sample size, the expected incidence of ED will be taken as 53% from a previous study.11 To estimate the incidence with a precision of 10%, 95% CI, 96 children undergoing general anesthesia for a procedure will be needed.
We entered and analyzed all study data in SPSS version 25. We reported incidence of ED as number and percentages.
3. RESULTS
We included a total of 96 children in the study. All variable data were found to have a non-normal distribution. The median age of children in the study was 59 (IQR: 43-76) months. Among 96 children, 30 (31.3%) were females vs 66 (68.8%) males. Sixty (62.5%) patients underwent day care surgery. The distribution of children by surgical specialties is demonstrated in graph I. Twenty-five (26%) children underwent adenotonsillectomy followed by dental rehabilitation 23 (24%), hernia repair 15 (15.6%), orchidopexy 8 (8.3%), EUA ENT 6 (6.3%), circumcision 4 (4.2%), eye surgery 4 (4.2%) and grommet 3 (3.1%). Among 96 patients, 2 were asthmatic, 2 had renal disease and 1 had hearing problems. No patient had any adverse event in the perioperative period.
| Box 1: Pediatric Anesthesia Emergence Delirium’ (PAED) score | ||||||
| Point | Description of items | Not at
all |
Just a little | Quite a bit | Very much | Extremely |
| 1 | The child makes eye contact with the caregiver | 4 | 3 | 2 | 1 | 0 |
| 2 | The child’s actions are purposeful | 4 | 3 | 2 | 1 | 0 |
| 3 | The child is aware of his/her surroundings | 4 | 3 | 2 | 1 | 0 |
| 4 | The child is restless | 0 | 1 | 2 | 3 | 4 |
| 5 | The child is inconsolable | 0 | 1 | 2 | 3 | 4 |
| One-calm, two-not calm but could be easily consoled, three-moderately agitated or restless and not quickly quiet, four-combative, excited and thrashing around. PAED: Pediatric emergency delirium scale.
· Locatelli BG, Ingelmo PM, Emre S, Meroni V, Minardi C, Frawley G, et al. Emergence delirium in children: a comparison of sevoflurane and desflurane anesthesia using the Paediatric Anesthesia Emergence Delirium scale. Paediatr Anaesth. 2013; 23: 301-308 DOI: 10.1111/pan.12038 |
||||||
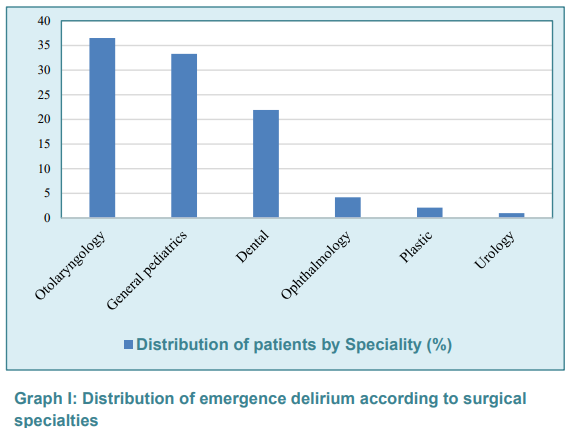
The median emergence delirium score of children was 8 (5-12). The incidence of postoperative ED in pediatric patients was 38.5% (37 cases). Patients with emergence delirium were younger with median age 56 (45-70.5) months compared to 63 (35-80) months in children without emergence delirium. Sixty five percent of children with emergence delirium were male vs 71.1% in children without emergence delirium. Fifty four percent of children with emergence delirium underwent surgery as day care while 67.7% in children without emergence delirium. Seventy percent of children with emergence delirium underwent ENT and dental surgeries vs 50.8% in children without emergence delirium.
4. DISCUSSION
Our study showed an incidence of postoperative emergence delirium as 38.5%. This is consistent with findings in the study by Redoque et al who reported an incidence ranging from 20-80%.12 Zainab et al reported a higher incidence of 51.6% in their study on children undergoing dental surgery.13 Pieters et al demonstrated an incidence of ED as 53% that is also higher than our study.14 There could be different explanations for these varied incidences in different studies. Several measuring tools have been developed previously to find out the incidence of ED. Additionally, different studies have also used different criteria to label ED. Some of these scales include Cravero scale, Watcha scale and PAED score etc. Watcha scale is considered a user-friendly tool to detect delirium although PAED score is used to determine its degree.14-17 PAED score has been regarded as gold standard to assess ED previously, but it has been modified by Locatelli et al.18 who focused only on first 3 criteria to increase its specificity.
In our study, patients with ED were relatively younger compared to children without ED. Redoque et al.12 also showed that incidence of ED is 3 to 8 times greater in children less than 5 years of age. In another study by Aono et al, ED occurs more frequently in preschool children.19 Patel et al demonstrated that ED is more common in preschool aged children than adults with an overall incidence 12-13% in children.20
In our study, 64.8% of children with emergence delirium were male vs 71.1% in children without emergence delirium. Also, the overall percentage of male children in our study was higher as 68.8%. Although, Munk et al demonstrated a positive correlation of male gender to the occurrence of ED in adult patients.21 Another observational study by Houben et al reported a higher incidence of ED in male pediatric patients after adenoidectomy.22
Our study results showed that 70% of children with ED underwent ENT and dental surgeries compared to 50.8% in children without ED. Lee et al also reported a positive association of ED with oral, ophthalmological and ENT surgeries.23 Vopel-Lewis et al found a higher incidence of ED in children who underwent ENT surgeries (26%, relative risk = 1.69, P = 0.004).24 Dahmani et al also described a higher incidence of ED in patients who underwent ENT and ophthalmologic surgeries.4
5. LIMITATIONS
This is the only study on pediatric delirium incidence in Saudi population. But there are a few limitations in our study. It is a single-center study. We had a relatively smaller sample size. We recommend further research on this topic with larger sample size.
6. CONCLUSION
We found an incidence of 38.5% of emergence delirium after general anesthesia in children at a hospital setting in a Middle East country.
7. Data availability
The numerical data generated during this research is available with the authors.
8. Acknowledgement
We gratefully thank Faculty of Medicine
9. Conflict of interest
The study utilized the hospital resources only, and no external or industry funding was involved.
10. Authors’ contribution
AUH: Original concept, Scientific literature search, Data collection, Data analysis, Manuscript writing, Editing, Final Approval
AA: Data collection, Manuscript writing, Editing, Final Approval
ZS: Scientific literature search, Manuscript writing, Editing, Final Approval
11. REFERENCES
- Malarbi S, Stargatt R, Howard K, Davidson A. Characterizing the behaviour of children emerging with delirium from general anesthesia. Paediatr Anaesth. 2011;21:942-950. PMID: 21726352 DOI: 1111/j.1460-9592.2011.03646.x
- Dahmani S, Delivet H, Hilly J. Emergence delirium in children: an update. Curr Opin Anaesthesiol. 2014;27:309-315. PMID: 24784918 DOI: 1097/ACO.0000000000000076
- Banchs RJ, Lerman J. Preoperative anxiety management, emergence delirium, and postoperative behaviour. Anesthesiol Clin. 2014;32:1-23. PMID: 24491647 DOI: 1016/j.anclin.2013.10.011
- Dahmani S, Stany I, Brasher C, Lejeune C, Bruneau B, Wood C, et al. Pharmacological prevention of sevoflurane- and desflurane-related emergence agitation in children: a meta-analysis of published studies. Br J Anaesth. 2010;104:216-23. PMID: 20047899 DOI: 1093/bja/aep376
- Lepousé C, Lautner CA, Liu L, Gomis P, Leon A. Emergence delirium in adults in the post-anesthesia care unit. Br J Anaesth. 2006;96:747-753. PMID: 16670111 DOI: 1093/bja/ael094
- Yu D, Chai W, Sun X, Yao L. Emergence agitation in adults: risk factors in 2,000 patients. Can J Anaesth. 2010;57:843-848. PMID: 20526708 DOI: 1007/s12630-010-9338-9
- Kim YS, Chae YK, Choi YS, Min JH, Ahn SW, Yoon JW, et al. A comparative study of emergence agitation between sevoflurane and propofol anesthesia in adults after closed reduction of nasal bone fracture. Korean J Anesthesiol. 2012;63:48-53. PMID: 22870365 DOI: 4097/kjae.2012.63.1.48
- Nair S, Wolf A. Emergence delirium after pediatric anesthesia: new strategies in avoidance and treatment. BJA Educ. 2018;18:30-33. PMID: 33456792 DOI: 1016/j.bjae.2017.07.001
- Jindal P, Khurana G, Oberoi D, Sharma JP. Recovery profile and emergence delirium following sevoflurane and isoflurane anesthesia in children posted for cleft lip surgery. Middle East J Anaesthesiol. 2012;21:679-684. PMID: 23265030
- Grotmol OG, Nesarajah N, Hansen TG. Postoperative emergence delirium in children: a narrative review of recent publications. Signa Vitae. 2021;17(3):10-20. DOI: 22514/sv.2021.057
- Shi M, Miao S, Gu T, Wang D, Zhang H, Liu J. Dexmedetomidine for the prevention of emergence delirium and postoperative behavioural changes in pediatric patients with sevoflurane anesthesia: a double-blind, randomized trial. Drug Des Devel Ther. 2019;13:897-905. PMID: 30936683 DOI: 2147/DDDT.S196075
- Reduque LL, Verghese ST. Pediatric emergence delirium. Cont Ed Anesth Crit Care Pain. 2013;13:39‑ DOI: 10.1093/bjaceaccp/mks051
- Jooma Z, Perrie H, Scribante J, Kleyenstuber T. Emergence delirium in children undergoing dental surgery under general anesthesia. Paediatr Anaesth. 2020;30:1020-1026. PMID: 32470145 DOI: 1111/pan.13937
- Pieters BJ, Penn E, Nicklaus P, Bruegger D, Mehta B, Weatherly R. Emergence delirium and postoperative pain in children undergoing adenotonsillectomy: a comparison of propofol vs sevoflurane anesthesia. Paediatr Anaesth. 2010;20:944-950. PMID: 20735801 DOI: 1111/j.1460-9592.2010.03394.x
- Sikich N, Lerman J. Development and psychometric evaluation of the pediatric anesthesia emergence delirium scale. Anesthesiology. 2004;100:1138-1145. PMID: 15114210 DOI: 1097/00000542-200405000-00015
- Cravero J, Surgenor S, Whalen K. Emergence agitation in pediatric patients after sevoflurane anesthesia and no surgery: a comparison with halothane. Paediatr Anaesth. 2000;10:419-424. PMID: 10886700 DOI: 1046/j.1460-9592.2000.00560.x
- Bajwa SA, Costi D, Cyna AM. A comparison of emergence delirium scales following general anesthesia in children. Paediatr Anaesth. 2010;20:704-711. PMID: 20497353 DOI: 1111/j.1460-9592.2010.03328.x
- Locatelli BG, Ingelmo PM, Emre S, Meroni V, Minardi C, Frawley G, et al. Emergence delirium in children: a comparison of sevoflurane and desflurane anesthesia using the Paediatric Anesthesia Emergence Delirium scale. Paediatr Anaesth. 2013;23:301-8. PMID: 23043512 DOI: 1111/pan.12038
- Aono J, Ueda W, Mamiya K, Takimoto E, Manabe M. Greater incidence of delirium during recovery from sevoflurane anesthesia in preschool boys. Anesthesiology. 1997;87:1298-300. PMID: 9416712 DOI: 1097/00000542-199712000-00006
- Urits I, Peck J, Giacomazzi S, Patel R, Wolf J, Mathew D, et al. Emergence Delirium in Perioperative Pediatric Care: A Review of Current Evidence and New Directions. Adv Ther. 2020;37:1897-1909. PMID: 32274749 DOI: 1007/s12325-020-01317-x
- Munk L, Andersen G, Møller AM. Post-anesthetic emergence delirium in adults: incidence, predictors and consequences. Acta Anaesthesiol Scand. 2016;60:1059-1066. PMID: 26968337 DOI: 1111/aas.12717
- Houben A, Ghamari S, Fischer A, Neumann C, Baehner T, Ellerkmann RK. Pediatric emergence delirium is linked to increased early postoperative negative behavior within two weeks after adenoidectomy: an observational study. Braz J Anesthesiol. 2021;S0104-0014(21)00138-X. PMID: 33887334 DOI: 1016/j.bjane.2021.03.008
- Lee YC, Kim JM, Ko HB, Lee SR. Use of laryngeal mask airway and its removal in a deeply anaesthetized state reduces emergence agitation after sevoflurane anaesthesia in children. J Int Med Res. 2011;39:2385-2392. PMID: 22289558 DOI: 1177/147323001103900639
- Voepel-Lewis T, Malviya S, Tait AR. A prospective cohort study of emergence agitation in the pediatric postanesthesia care unit. Anesth Analg. 2003;96:1625-1630. PMID: 12760985 DOI: 10.1213/01.ANE.0000062522.21048.61