Vania Ayu Puspamaniar1, Azizah Amimathul Firdha2, Nurul Azizah3, Hanik Badriyah Hidayati4
Author affiliations:
Hypokalemic Periodic Paralysis (HPP) is a neurological manifestation of hypokalemia, with a prevalence of 1 in 100,000. HPP is recognized by the sudden onset of muscle paralysis and low serum potassium. Due to its various causes, it may be misdiagnosed and neglected.
We present a case of 42-year-old Asian female with weakness of both legs and cramps. The weakness was felt upon awakening from sleep. She also complained of palpitation, tiredness, sweating, heat intolerance, and hand tremors. In the recent weeks, her appetite increased.
Periodic paralysis (PP) is characterized by bursts of painless muscle weakening. A possible cause of periodic paralysis is hypokalemia which was found in our case. Hyperthyroid is classified into potassium depletion by extra renal route which was found in this case. Management
When managing a patient with sudden onset weakness or paralysis, it is crucial to consider the possibility of periodic paralysis. HPP is a rare but serious medical emergency. This should be suspected in any patient presenting with sudden muscle weakness. Prompt correction of any abnormalities in potassium levels can lead to rapid and complete symptom resolution. To avoid persistent or recurrent paralysis, any underlying causes should be effectively managed wherever possible.
Keywords: Hypokalemia; Paralysis; Hyperthyroid; Hypokalemic Periodic Paralysis
Citation: Puspamaniar VA, Firdha AA, Azizah N, Hidayati HB. Neurological manifestations of hypokalemia: a case report. Anaesth. pain intensive care 2024;28(1):187−190; DOI: 10.35975/apic.v28i1.2387
Received: September 03, 2023; Reviewed: September 16, 2023; Accepted: September 19, 2023
Hypokalemia is a condition when potassium level in bloodstream is lower than the normal. This electrolyte imbalance manifests in various signs such as muscle twitches, muscle cramps, muscle paralysis, hypotension, arrhythmias, excessive urination, and excessive thirst. One of the neurological manifestations is Hypokalemic Periodic Paralysis (HPP). HPP is a rare disorder of channelopathy with a prevalence of 1 in 100,000. It is characterized by the sudden onset of muscle paralysis and low serum potassium levels.1-3 It commonly occurs in males rather than females. Heavy carbohydrate meals, stress, infection, glucose infusion, steroids, alcohol use, hypothermia, and strenuous exercise can trigger this condition.3 The episodes last from a few minutes to several days, with spontaneous recovery.4
HPP can be primary or secondary. The calcium or sodium ion channel mutation causes primary HPP, such as CACNA1S, SCN4A, and KCNJ2. Secondary HPP is associated with hyperthyroidism, renal tubular acidosis, Gitelman syndrome, and primary hyperaldosteronism and hypokalemia secondary to gastrointestinal losses.5
Because HPP is a rare condition, it may be misdiagnosed and neglected. Particularly in the fourth and fifth decades of life, this illness has the potential to proceed to persistent myelopathy.4 The delay of prompt treatment for HPP can lead to life-threatening conditions such as respiratory decompensation and arrhythmias.3 While early recognition and therapy could lead to good outcomes and complete recovery. We report of a patient with hypokalemic periodic paralysis and highlight the significance of conducting regular thyroid screenings as part of the patient's follow-up care
A 42-year-old female presented to the emergency room and complained of lower limb weakness for 6 hours. Her both legs felt weak and cramped. She experienced weakness upon awakening from sleep. There was no weakness in other parts of her body and no respiratory difficulty. She also complained of palpitations, tiredness, sweating, heat intolerance and hand tremors. In the recent weeks, her appetite had increased. She had no complaints of nausea, vomiting, diarrhea, cough, common cold, fever, urinary retention, constipation, headache, dizziness, loss of consciousness, and shortness of breath during activity. There was no history of trauma. A while ago, she had a similar episode and went to the ER but came home after a few injections and made a full recovery. She had no family history of periodic paralysis or other significant illnesses. She had no allergy to foods or drugs. She denied the use of any drugs or alcohol.
Vital signs showed her respiratory rate 20 breaths per minute, pulse 108 beats per minute, temperature 36.5 °C, blood pressure 108/80 mmHg, and oxygen saturation 98% on room air. The physical examination of the head, neck, thorax, abdomen and extremities was normal. There was no thyroid enlargement, tenderness on neck palpation, or exophthalmos. Neurologic examination showed bilateral lower limb weakness. Cranial nerve and sensory examination was within normal range.
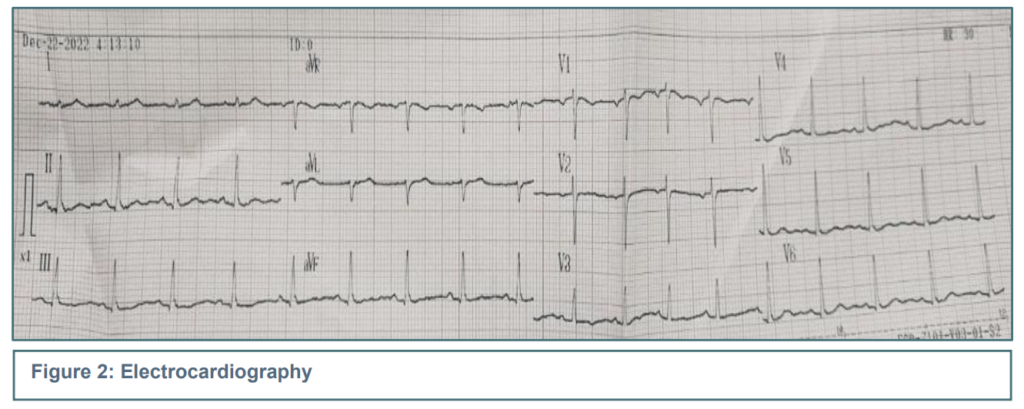
Laboratory tests showed normal complete blood count, urea, creatinine and blood glucose. The serum electrolytes showed low potassium (3.3 mmol/l), high chloride (108 mmol/l) and normal sodium (141 mmol/l). The thyroid function showed high T4 (21.97 µg/dL), normal T3, and normal TSH levels. ECG showed sinus rhythm. Her chest x-ray was normal.
From these data, the patient was diagnosed with hypokalemic periodic paralysis with hyperthyroidism. The patient was treated with Ringer lactate infusion with KCl 25 mEq/500 mL/12 h followed by Ringer lactate with Vitamin B1, B6, and B12 3 mL/500 mL over12 h, mecobalamin injection 3x500 µg, omeprazole injection 2 x 40 mg, Alinamin F injection 2x1 ampoule, KSR 2x600 mg, and Propyl thiouracil 3x100 mg. After the patient had initial therapy in the ER, the patient’s motor function was improved by 4/4. So that therapy was continued. On the second day of therapy, potassium levels returned to normal, followed by the patient's motor function (neurologic examination showing 5/5). She was discharged home after the treatment, with instructions to see an endocrinologist to follow up on her condition.
Most of the times muscle weakness is thought to be due to neuronal damage, but it can be caused by some systemic abnormalities and hypokalemia is one of them. The etiology of hypokalemia is divided into three groups–potassium depletion by renal causes, potassium depletion by extra renal causes, and potassium shift into cells. The renal causes include increased aldosterone, diuretic hypomagnesemia, renal tubular acidosis (Type I and II), metabolic alkalosis, and Liddle's syndrome. Extra renal causes consist of decreased intake, vomiting, diarrhea, Zollinger-Ellison Syndrome and fistulas. Intracellular shift of potassium is caused by increased insulin, alkalosis, hyperthyroidism, thyrotoxic periodic paralysis, and familial hypokalemic paralysis.6
Hypokalemia manifests in various signs such as muscle twitches, muscle cramps, muscle paralysis, hypotension, arrhythmias, excessive urination, and excessive thirst (polydipsia). This periodic paralysis due to hypokalemia is also known as hypokalemic periodic paralysis (HPP). With an incidence of 1 in 100,000, HPP is the most prevalent of all. Familial hypokalmic paralysis (FHP), a poorly known illness that can develop spontaneously or as the result of autosomal dominant inheritance, can sporadically manifest as HPP.7,8 This type of periodic paralysis is thought to be caused by disorganized cellular potassium control, possibly as a result of faulty sodium or calcium channels.9,10 It has been determined that mutations in the CACNA1S and SCN4A genes lead to anomalies in sodium channels and aberrant potassium ion flow. Strenuous activity, fasting, or eating foods high in carbohydrates, might cause these episodes. Different kinds of periodic paralysis have been connected to problems in electrolytes and metabolism.
Depending on the underlying cause, the clinical symptoms of the syndrome can vary significantly, but the most notable trait is the rapid onset of weakness, which can range in severity from mild, temporary weakness to severe impairment, leading to life-threatening respiratory failure. Stress factors, such a viral infection or exhaustion, as well as some drugs like beta-agonists, insulin, or steroids, can cause attacks. Low potassium levels and muscular dysfunction are the results of a disturbance of sodium and calcium ion channels.10 Tendon reflexes may be diminished or missing but sensation is typically unaffected because this is mostly a problem with muscle contraction rather than nerve conduction. Though other electrolytes are typically normal, the serum potassium level is frequently frighteningly low. Potassium replenishment and careful monitoring of the heart rhythm and serum potassium levels are needed to treat acute paralytic episodes. HPP is a potentially fatal side effect of hyperthyroidism.8
Probably the cause of hypokalemic in our patient, was the hyperthyroid condition, because there were no complaints of vomiting, diarrhea, high carbohydrate consumption, and no abnormalities on kidney function.
Based on the Wayne index as a hyperthyroid score, a score of 19 was obtained from the patient’s signs and symptoms, indicating hyperthyroidism. Our patient's increased thyroid hormone T4 levels are an indication of hyperthyroidism, which may lead to an increase in Na/K/ATPase activity and, ultimately, hypokalemia.
The correction of serum potassium levels and the focus on cardiac anomalies should be focused when stabilizing HPP with hyperthyroid patients. Only the intracellular shift of potassium is the cause of hypokalemia as total body potassium loss is not present. Overzealous potassium replacement frequently results in rebound hyperkalemia. The majority of patients will experience an increase in potassium levels following initial potassium delivery, however up to 25% of patients may experience an initial dip that stabilizes over a few hours. When too much potassium enters the extracellular environment, hyperkalemia can result. The consensus is that less than 10 mmol/h of potassium chloride should be replaced. Some reports advise using IV or oral propranolol to reverse hypokalemia by inhibiting the beta-adrenergic receptors, if a potassium supplement is insufficient. Prior to reaching a euthyroid state, this therapy may also stop attacks. As was the case with this patient, whose symptoms improved after obtaining potassium correction. After the second day of therapy, potassium levels returned to normal, which was followed by the patient's motor function..3,9
When managing a patient with sudden onset weakness or paralysis, it is crucial to consider the possibility of periodic paralysis, particularly if the patient lacks a previous history or symptoms of such conditions. Hypokalemic Periodic Paralysis (HPP) is a rare but serious medical emergency. Early diagnosis and prompt treatment can help prevent life-threatening complications, including respiratory failure and arrhythmias. HPP should be suspected in any patient presenting with sudden muscle weakness. In all cases of sudden muscle weakness, serum electrolyte levels, ECG, and thyroid function tests should be conducted. Prompt correction of any abnormalities in potassium levels can lead to rapid and complete symptom resolution. The prognosis is good because there is no brain damage, but it can recur. To avoid persistent or recurrent paralysis, any underlying cause should be effectively managed wherever possible.
5. Acknowledgement
We gratefully thank Neurology Department, Faculty of Medicine Airlangga University – RSUD Dr. Soetomo, Surabaya, Jawa, Indonesia
6. Ethical considerations
Written consent was obtained from the patient to use his data for academic purposes.
7. Authors’ contribution
VAP, NA: conception of the work, literature research, manuscript drafting
AAF: literature research, performed the analysis, manuscript editing
HBH: literature research, manuscript reviewing and revising
Author affiliations:
- Vania Ayu Puspamaniar, General Practitioner Petrokimia Gresik Hospital, Gresik, Indonesia; E-mail: puspamaniar06@gmail.com
- Azizah Amimathul Firdha, Indonesian Medical Association (IDI) Surabaya chapter, Surabaya, Indonesia; E-mail: azizah12.x2@gmail.com
- Nurul Azizah, Staff of Neurology Department, Petrokimia Gresik Hospital, Gresik, Indonesia; nurulazizah2007@yahoo.com
- Hanik Badriyah, Staff of Neurology Department, Faculty of Medicine Airlangga University – RSUD Dr. Soetomo, Surabaya, Jawa, Indonesia; E-mail: hanikhidayati@fk.unair.ac.id
ABSTRACT
Hypokalemic Periodic Paralysis (HPP) is a neurological manifestation of hypokalemia, with a prevalence of 1 in 100,000. HPP is recognized by the sudden onset of muscle paralysis and low serum potassium. Due to its various causes, it may be misdiagnosed and neglected.
We present a case of 42-year-old Asian female with weakness of both legs and cramps. The weakness was felt upon awakening from sleep. She also complained of palpitation, tiredness, sweating, heat intolerance, and hand tremors. In the recent weeks, her appetite increased.
Periodic paralysis (PP) is characterized by bursts of painless muscle weakening. A possible cause of periodic paralysis is hypokalemia which was found in our case. Hyperthyroid is classified into potassium depletion by extra renal route which was found in this case. Management
When managing a patient with sudden onset weakness or paralysis, it is crucial to consider the possibility of periodic paralysis. HPP is a rare but serious medical emergency. This should be suspected in any patient presenting with sudden muscle weakness. Prompt correction of any abnormalities in potassium levels can lead to rapid and complete symptom resolution. To avoid persistent or recurrent paralysis, any underlying causes should be effectively managed wherever possible.
Keywords: Hypokalemia; Paralysis; Hyperthyroid; Hypokalemic Periodic Paralysis
Citation: Puspamaniar VA, Firdha AA, Azizah N, Hidayati HB. Neurological manifestations of hypokalemia: a case report. Anaesth. pain intensive care 2024;28(1):187−190; DOI: 10.35975/apic.v28i1.2387
Received: September 03, 2023; Reviewed: September 16, 2023; Accepted: September 19, 2023
INTRODUCTION
Hypokalemia is a condition when potassium level in bloodstream is lower than the normal. This electrolyte imbalance manifests in various signs such as muscle twitches, muscle cramps, muscle paralysis, hypotension, arrhythmias, excessive urination, and excessive thirst. One of the neurological manifestations is Hypokalemic Periodic Paralysis (HPP). HPP is a rare disorder of channelopathy with a prevalence of 1 in 100,000. It is characterized by the sudden onset of muscle paralysis and low serum potassium levels.1-3 It commonly occurs in males rather than females. Heavy carbohydrate meals, stress, infection, glucose infusion, steroids, alcohol use, hypothermia, and strenuous exercise can trigger this condition.3 The episodes last from a few minutes to several days, with spontaneous recovery.4
HPP can be primary or secondary. The calcium or sodium ion channel mutation causes primary HPP, such as CACNA1S, SCN4A, and KCNJ2. Secondary HPP is associated with hyperthyroidism, renal tubular acidosis, Gitelman syndrome, and primary hyperaldosteronism and hypokalemia secondary to gastrointestinal losses.5
Because HPP is a rare condition, it may be misdiagnosed and neglected. Particularly in the fourth and fifth decades of life, this illness has the potential to proceed to persistent myelopathy.4 The delay of prompt treatment for HPP can lead to life-threatening conditions such as respiratory decompensation and arrhythmias.3 While early recognition and therapy could lead to good outcomes and complete recovery. We report of a patient with hypokalemic periodic paralysis and highlight the significance of conducting regular thyroid screenings as part of the patient's follow-up care
CASE REPORT
A 42-year-old female presented to the emergency room and complained of lower limb weakness for 6 hours. Her both legs felt weak and cramped. She experienced weakness upon awakening from sleep. There was no weakness in other parts of her body and no respiratory difficulty. She also complained of palpitations, tiredness, sweating, heat intolerance and hand tremors. In the recent weeks, her appetite had increased. She had no complaints of nausea, vomiting, diarrhea, cough, common cold, fever, urinary retention, constipation, headache, dizziness, loss of consciousness, and shortness of breath during activity. There was no history of trauma. A while ago, she had a similar episode and went to the ER but came home after a few injections and made a full recovery. She had no family history of periodic paralysis or other significant illnesses. She had no allergy to foods or drugs. She denied the use of any drugs or alcohol.
Vital signs showed her respiratory rate 20 breaths per minute, pulse 108 beats per minute, temperature 36.5 °C, blood pressure 108/80 mmHg, and oxygen saturation 98% on room air. The physical examination of the head, neck, thorax, abdomen and extremities was normal. There was no thyroid enlargement, tenderness on neck palpation, or exophthalmos. Neurologic examination showed bilateral lower limb weakness. Cranial nerve and sensory examination was within normal range.
| Table 1: Laboratory test results | ||
| Category | Normal Range | Results |
| Hemoglobin (g/dL) | 11 – 16.5 | 13.6 |
| WBC (x103/mm3) | 4 - 10 | 9.14 |
| HCT (%) | 35-45 | 41.8 |
| Thrombocyte (x103/mm3) | 150-450 | 326 |
| RBC (x106/µL) | 4-5 | 4.57 |
| Differential count | ||
| Eosinophils (%) | 1-2 | 1.4 |
| Basophils (%) | 0-1 | 0.4 |
| Neutrophils (%) | 54-62 | 60.7 |
| Lymphocytes (%) | 25-33 | 32.3 |
| Monocyte (%) | 3-7 | 5.2 |
| Glucose (mg/dL) | 70-140 | 106 |
| Serum electrolytes | ||
| Sodium (mmol/l) | 135-148 | 141 |
| Potassium (mmol/l) | 3.5-5.3 | 3.3 |
| Chloride (mmol/l) | 98-107 | 108 |
| Renal Function | ||
| Urea (mg/dL) | < 50 | 12 |
| Creatinine | 0.5-0.9 | 0.6 |
| Thyroid function tests | ||
| T3 (CLIA) | 0.58-1.62 ng/ml | 0.85 ng/ml |
| T4 (CLIA) | 5-14.5 µg/dL | 21.97 µg/dL |
| TSH (CLIA) | 0.35-5.1 µIU/mL | 4.35 µIU/mL |
| SARS-CoV2 | Negative | Negative |
| Results outside normal range are bold; CLIA: The Clinical Laboratory Improvement Amendments of 1988 | ||
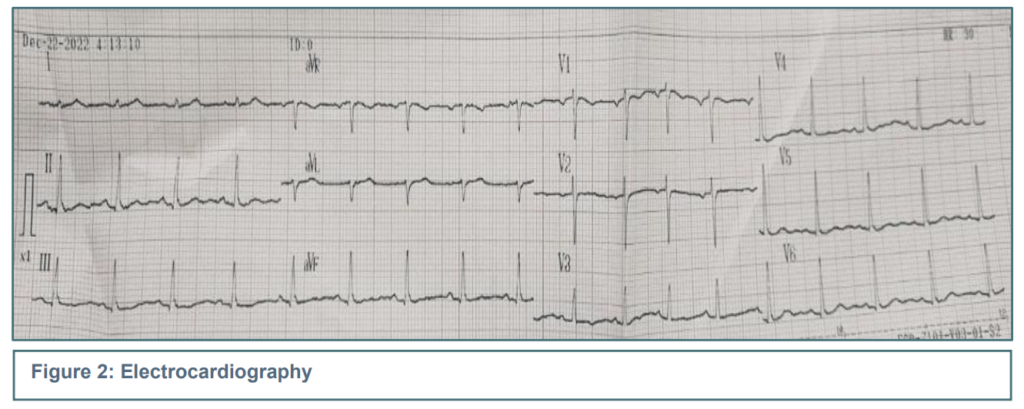
Laboratory tests showed normal complete blood count, urea, creatinine and blood glucose. The serum electrolytes showed low potassium (3.3 mmol/l), high chloride (108 mmol/l) and normal sodium (141 mmol/l). The thyroid function showed high T4 (21.97 µg/dL), normal T3, and normal TSH levels. ECG showed sinus rhythm. Her chest x-ray was normal.
From these data, the patient was diagnosed with hypokalemic periodic paralysis with hyperthyroidism. The patient was treated with Ringer lactate infusion with KCl 25 mEq/500 mL/12 h followed by Ringer lactate with Vitamin B1, B6, and B12 3 mL/500 mL over12 h, mecobalamin injection 3x500 µg, omeprazole injection 2 x 40 mg, Alinamin F injection 2x1 ampoule, KSR 2x600 mg, and Propyl thiouracil 3x100 mg. After the patient had initial therapy in the ER, the patient’s motor function was improved by 4/4. So that therapy was continued. On the second day of therapy, potassium levels returned to normal, followed by the patient's motor function (neurologic examination showing 5/5). She was discharged home after the treatment, with instructions to see an endocrinologist to follow up on her condition.
3. DISCUSSION
Most of the times muscle weakness is thought to be due to neuronal damage, but it can be caused by some systemic abnormalities and hypokalemia is one of them. The etiology of hypokalemia is divided into three groups–potassium depletion by renal causes, potassium depletion by extra renal causes, and potassium shift into cells. The renal causes include increased aldosterone, diuretic hypomagnesemia, renal tubular acidosis (Type I and II), metabolic alkalosis, and Liddle's syndrome. Extra renal causes consist of decreased intake, vomiting, diarrhea, Zollinger-Ellison Syndrome and fistulas. Intracellular shift of potassium is caused by increased insulin, alkalosis, hyperthyroidism, thyrotoxic periodic paralysis, and familial hypokalemic paralysis.6
Hypokalemia manifests in various signs such as muscle twitches, muscle cramps, muscle paralysis, hypotension, arrhythmias, excessive urination, and excessive thirst (polydipsia). This periodic paralysis due to hypokalemia is also known as hypokalemic periodic paralysis (HPP). With an incidence of 1 in 100,000, HPP is the most prevalent of all. Familial hypokalmic paralysis (FHP), a poorly known illness that can develop spontaneously or as the result of autosomal dominant inheritance, can sporadically manifest as HPP.7,8 This type of periodic paralysis is thought to be caused by disorganized cellular potassium control, possibly as a result of faulty sodium or calcium channels.9,10 It has been determined that mutations in the CACNA1S and SCN4A genes lead to anomalies in sodium channels and aberrant potassium ion flow. Strenuous activity, fasting, or eating foods high in carbohydrates, might cause these episodes. Different kinds of periodic paralysis have been connected to problems in electrolytes and metabolism.
Depending on the underlying cause, the clinical symptoms of the syndrome can vary significantly, but the most notable trait is the rapid onset of weakness, which can range in severity from mild, temporary weakness to severe impairment, leading to life-threatening respiratory failure. Stress factors, such a viral infection or exhaustion, as well as some drugs like beta-agonists, insulin, or steroids, can cause attacks. Low potassium levels and muscular dysfunction are the results of a disturbance of sodium and calcium ion channels.10 Tendon reflexes may be diminished or missing but sensation is typically unaffected because this is mostly a problem with muscle contraction rather than nerve conduction. Though other electrolytes are typically normal, the serum potassium level is frequently frighteningly low. Potassium replenishment and careful monitoring of the heart rhythm and serum potassium levels are needed to treat acute paralytic episodes. HPP is a potentially fatal side effect of hyperthyroidism.8
Probably the cause of hypokalemic in our patient, was the hyperthyroid condition, because there were no complaints of vomiting, diarrhea, high carbohydrate consumption, and no abnormalities on kidney function.
Based on the Wayne index as a hyperthyroid score, a score of 19 was obtained from the patient’s signs and symptoms, indicating hyperthyroidism. Our patient's increased thyroid hormone T4 levels are an indication of hyperthyroidism, which may lead to an increase in Na/K/ATPase activity and, ultimately, hypokalemia.
The correction of serum potassium levels and the focus on cardiac anomalies should be focused when stabilizing HPP with hyperthyroid patients. Only the intracellular shift of potassium is the cause of hypokalemia as total body potassium loss is not present. Overzealous potassium replacement frequently results in rebound hyperkalemia. The majority of patients will experience an increase in potassium levels following initial potassium delivery, however up to 25% of patients may experience an initial dip that stabilizes over a few hours. When too much potassium enters the extracellular environment, hyperkalemia can result. The consensus is that less than 10 mmol/h of potassium chloride should be replaced. Some reports advise using IV or oral propranolol to reverse hypokalemia by inhibiting the beta-adrenergic receptors, if a potassium supplement is insufficient. Prior to reaching a euthyroid state, this therapy may also stop attacks. As was the case with this patient, whose symptoms improved after obtaining potassium correction. After the second day of therapy, potassium levels returned to normal, which was followed by the patient's motor function..3,9
4. CONCLUSION
When managing a patient with sudden onset weakness or paralysis, it is crucial to consider the possibility of periodic paralysis, particularly if the patient lacks a previous history or symptoms of such conditions. Hypokalemic Periodic Paralysis (HPP) is a rare but serious medical emergency. Early diagnosis and prompt treatment can help prevent life-threatening complications, including respiratory failure and arrhythmias. HPP should be suspected in any patient presenting with sudden muscle weakness. In all cases of sudden muscle weakness, serum electrolyte levels, ECG, and thyroid function tests should be conducted. Prompt correction of any abnormalities in potassium levels can lead to rapid and complete symptom resolution. The prognosis is good because there is no brain damage, but it can recur. To avoid persistent or recurrent paralysis, any underlying cause should be effectively managed wherever possible.
5. Acknowledgement
We gratefully thank Neurology Department, Faculty of Medicine Airlangga University – RSUD Dr. Soetomo, Surabaya, Jawa, Indonesia
6. Ethical considerations
Written consent was obtained from the patient to use his data for academic purposes.
7. Authors’ contribution
VAP, NA: conception of the work, literature research, manuscript drafting
AAF: literature research, performed the analysis, manuscript editing
HBH: literature research, manuscript reviewing and revising
8. REFERENCES
- Fialho D, Griggs RC, Matthews E. Periodic paralysis. Handb Clin Neurol. 2018;148:505–20. [PubMed] DOI: 1016/B978-0-444-64076-5.00032-6
- Holm-Yildiz S, Witting N, Dahlqvist J, de Stricker Borch J, Solheim T, Fornander F, et al. Permanent muscle weakness in hypokalemic periodic paralysis. Neurology. 2020;95(4):e342-e352. [PubMed] DOI: 1212/WNL.0000000000009828
- Lewis KL, Malouff TD, Kesler AM, Harris DM. Hypokalemic periodic paralysis - the importance of patient education. Rom J Intern Med. 2019;57(3):263–5. [PubMed] DOI: 2478/rjim-2019-0004
- Weber F, Lehmann-Horn F. Hypokalemic Periodic Paralysis. 2002 Apr 30. In: Adam MP, Feldman J, Mirzaa GM, et al., editors. GeneReviews® [Internet]. Seattle (WA): University of Washington, Seattle; 1993-2024. Available from: https://www.ncbi.nlm.nih.gov/books/NBK1338/
- Sardar Z, Waheed KAF, Javed MA, Akhtar F, Bokhari SRA. Clinical and Etiological Spectrum of Hypokalemic Periodic Paralysis in a Tertiary Care Hospital in Pakistan. Cureus. 2019;11(1):e3921. [PubMed] DOI: 7759/cureus.3921
- Kelley DE, Gharib H, Kennedy FP, Duda RJ, McManis PG. Thyrotoxic periodic paralysis. Report of 10 cases and review of electromyographic findings. Arch Intern Med 1989;149(11):2597–600. [PubMed] DOI: 1001/archinte.149.11.2597
- Fontaine B, Vale-Santos J, Jurkat-Rott K, Reboul J, Plassart E, Rime CS, et al. Mapping of the hypokalaemic periodic paralysis (HPP) locus to chromosome 1q31-32 in three European families. Nat Genet 1994;6(3):267–72. [PubMed] DOI: 1038/ng0394-267
- Soule BR, Simone NL. Hypokalemic Periodic Paralysis: a case report and review of the literature. Cases J. 2008;1(1):256. [PubMed] DOI: 1186/1757-1626-1-256
- Wang W, Jiang L, Ye L, Zhu N, Su T, Guan L, et al. Mutation screening in Chinese hypokalemic periodic paralysis patients. Mol Genet Metab. 2006;87(4):359–63. [PubMed] DOI: 1016/j.ymgme.2005.10.020
- 1Jurkat-Rott K, Lerche H, Lehmann-Horn F. Skeletal muscle channelopathies. J Neurol. 2002;249(11):1493–502. [PubMed] DOI: 10.1007/s00415-002-0871-5