Mai Mohammed Zakaria1, Sahar Kamal Mohammed Aboulella2, Sahar Mohammed Kamal Hassanein3, Ahmed Mohammed Elsayed El Hennawy4, Tarek Samir Salah El Din Shabana5
Author affiliations:
Background & objective: Nasogastric (NG) tube insertion is a frequently performed medical procedure. Most of the time, the oropharyngeal discomfort is usually underestimated, and insertions are carried out with just regular lubricant jelly and no additional painkillers, which results in less-than-ideal pain management. We compared the effectiveness of preemptive use of nebulized ketamine and dexamethasone in preventing post-operative sore throat following NG tube insertion in laparoscopic surgery.
Methods: This prospective randomized double-blind controlled study was carried on 108 patients of both sexes with ASA physical status I-II. aged 20-60 years, undergoing laparoscopic abdominal surgeries under general anesthesia. Patients were randomized into 3 equal groups. Group D received a dose of 8 mg nebulized dexamethasone. Group K received 50 mg nebulized ketamine. Group S received 5 ml of nebulized saline. NG tube was passed after induction of general anesthesia. Postoperative sore throat was enquired from the patients at full recovery (zero hour), then at 2, 8, 12 and 24 h. Computer software (SPSS 15.0.1. for Windows; SPSS Inc, Chicago, IL, 2001) was used for data analysis. Non-parametric quantitative data, median, range, percentages, and numbers are given for qualitative data. The appropriate analysis was conducted in line with the data obtained. P < 0.05 was regarded as significant.
Results: The incidence of postoperative sore throat (POST) was lower with both nebulized dexamethasone and nebulized ketamine compared with nebulized saline; and significantly lower with dexamethasone compared with ketamine at 0 h (P < 0.001), 2 h (P < 0.001), 8 h (P < 0.001), 12 h (P < 0.001), and 24 h (P < 0.001).
Conclusion: The current study revealed that preoperative nebulized dexamethasone was more effective than nebulized ketamine in reducing postoperative sore throat.
Abbreviations: NG- Nasogastric; NMDA- N-Methyl-D-Aspartate; PONV- Postoperative Nausea and Vomiting; POST- Postoperative Sore Throat; VAS- Visual Analogue Scale
Key words: Nebulization; Dexamethasone; Ketamine; Laparoscopic Surgery; Nasogastric Tube
Citation: Zakaria MM, Mohammed Aboulella SK, Hassanein SMK, Elsayed El Hennawy AM, Salah El Din Shabana TS. Role of preoperative dexamethasone nebulization versus ketamine nebulization in reducing complications of nasogastric tube after laparoscopic surgery. Anaesth. pain intensive care 2024;28(1):62-67.
DOI: 10.35975/apic.v28i1.2275
Received: 22 July, 2023; Reviewed: 04 October 2023; Accepted: 30 October 2023
In the clinical setting, nasogastric (NG) tube insertions are frequent medical procedures. Most of the time, the oropharyngeal discomfort is usually underestimated, and insertions are carried out with regular lubricant jelly and no additional painkillers, which results in less-than-ideal pain management.1
After general anesthesia and endotracheal intubation, postoperative sore throat (POST) is a common postoperative consequence. Both pharmaceutical and nonpharmacological approaches have been used to treat POST.2 In laparoscopic surgery, NG tubes are frequently used to decompress the stomach. POST severity increases when a nasogastric tube is used in conjunction with endotracheal intubation.3
Steroids have anti-inflammatory functions and are widely used in common practice. The inhaled corticosteroids deliver the drug to the site of action without much systemic side effects. Dexamethasone is a potent synthetic glucocorticoid with anti-inflammatory effects. It has been reported that dexamethasone effectively treats sore throat.4 Few clinical trials have evaluated the use of dexamethasone as a measure to reduce the mechanical impact of commonly used orally inserted devices. Corticosteroids are known to reduce inflammation, fluid transudation, edema and reduce pain severity.5
N-methyl-D-aspartate (NMDA) receptors play a significant role in nociception and inflammation in the human body. NMDA receptors are found in the central nervous system and peripheral nerves.6 Due to its anti-nociceptive and anti-inflammatory properties, ketamine, an N-methyl-D-aspartate (NMDA) receptor antagonist, has been administered as a gargle or nebulizer to lessen the frequency and intensity of POST.7 Ketamine nebulization is superior to ketamine gargle since the latter uses more of the drug and poses a danger of aspiration in addition to having a more unpleasant taste.8
We conducted this study to compare the efficacy of nebulization of dexamethasone with ketamine in the oropharynx of the patients before the induction of the general anesthesia, in reducing the postoperative sore throat related to nasogastric tube insertion.
One hundred and eight patients of both sexes with ASA physical status I-II, aged 20-60 years, who were undergoing laparoscopic abdominal surgeries under general anesthesia participated in this prospective randomized, double-blind controlled study. Approval from the local ethics committee of Ain Shams University and written informed consent from the patient or their representatives was obtained.
Patients with an ASA physical status III or higher, Mallampati > III, or multiple intubation attempts, history of an allergy to the study drug, surgeries lasting less than 30 min, heavy smokers, patients who had undergone more than one suction procedure, patients with esophageal pathologies, patients who had undergone laryngeal or pharyngeal surgery, patients who had recently experienced a respiratory tract infection or sore throat were excluded.
2.1. Randomization
Patients were randomized into three equal groups, 36 each, using a computer-generated random numbers table. Group D received 8 mg dexamethasone (2 ml added to 3 ml saline making a total of 5 ml). Group K received 50 mg ketamine (1ml added to 4 ml saline) and Group S received 5 ml of nebulized saline as a control group.
One of the anesthesiologists not involved in the ongoing research prepared and administered the 5 ml formulations. Before the induction of anesthesia, patients received the study medication through a nebulizer mask attached to an oxygen-driven source mounted on a wall (8 L of O2 per min) for 15 min.
Routine monitoring was done in the operating room including an electrocardiogram, a pulse oximeter, a non-invasive blood pressure monitor, and a capnometer. To induce anesthesia and aid endotracheal intubation, propofol 2 mg/kg, fentanyl 2 μg/kg, and atracurium 0.5 mg/kg were administered intravenously. Isoflurane 1-2% was used to maintain anesthesia, and top-up doses of atracurium 0.1 mg/kg were administered every 20 min. Endotracheal tube (ETT) was inserted. End-tidal carbon dioxide was maintained between 30-35 mmHg using mechanical ventilation adjustments. An experienced anesthesiologist gently placed 18-Fr nasogastric tube under vision after lubricating with jelly. Postoperative pain was managed with paracetamol 1 g IV every 6 h for 24 h postoperatively.
The duration of the nasogastric tube insertion was noted, and the total surgical time was estimated from the moment the anesthetic was induced until the patient was extubated. At the end of the surgery, the inhalational anesthetic was stopped, the muscle relaxant was reversed, and the extubation was done when the patient was fully conscious.
The study assessed several outcomes, including POST, odynophagia (pain when swallowing), postoperative nausea and vomiting, and hoarseness of voice, that could be associated with nasogastric tube insertion. Sore throat was evaluated at 0 h (at recovery when the patient can be tested), and at 2, 8, 12, and 24 h.
POST related pain was measured using the Visual Analogue Scale (VAS) score.
Using a binary scale (yes or no), postoperative hoarseness of voice, odynophagia, postoperative nausea and vomiting (PONV) were evaluated.
2.2. Primary and secondary outcomes
The primary outcome was the comparison of postoperative sore throat using the VAS score between the three groups.
The secondary outcome assessed the rate [n (%)] of odynophagia, hoarseness of voice, and PONV between the three groups.
2.3. Sample size calculation
Using the G power software, calculate sample size, power is 80%, and alpha error is 5%. Reviewing the findings of an earlier pertinent investigation (Mostafa et al., 2018) revealed a medium effect size difference (0.3) regarding the incidence of POST among various intervention groups. A sample size of at least 36 patients per group was required in light of these findings.
2.4. Statistical analysis
Using a statistical tool for social research, the acquired data was updated, coded, and entered into a computer software (SPSS 15.0.1. for Windows; SPSS Inc, Chicago, IL, 2001). The mean and standard deviation (SD) were reported for quantitative data. Non-parametric quantitative data, median, range, percentages, and numbers are given for qualitative data. The appropriate analysis was conducted in line with the data obtained. P < 0.05 was regarded as significant.
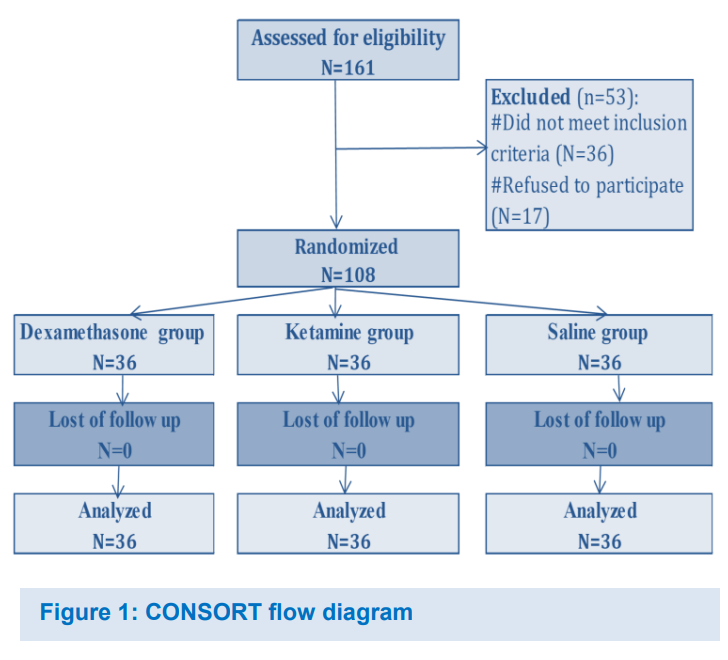
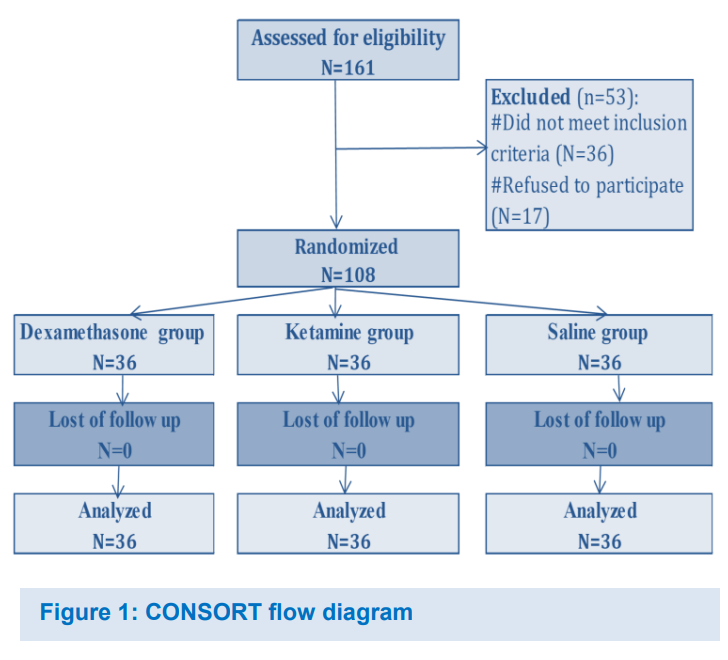
A total of 161patients were assessed for eligibility, as shown in Figure 1, out of which 53 patients were excluded so total number randomized and analyzed was 108 patients, equally divided into 36 patients in each group.
There was no statistically significant difference between the studied groups regarding baseline characteristics: age, sex, weight, ASA, and operation duration (Table 1).
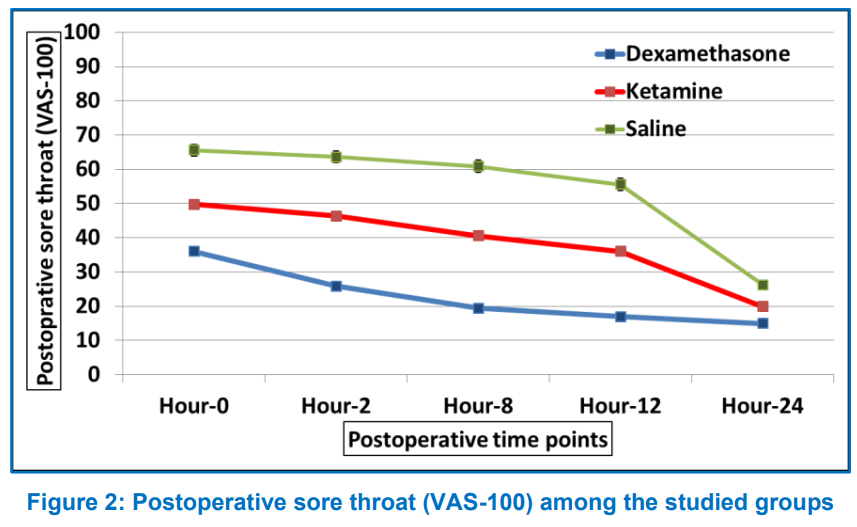
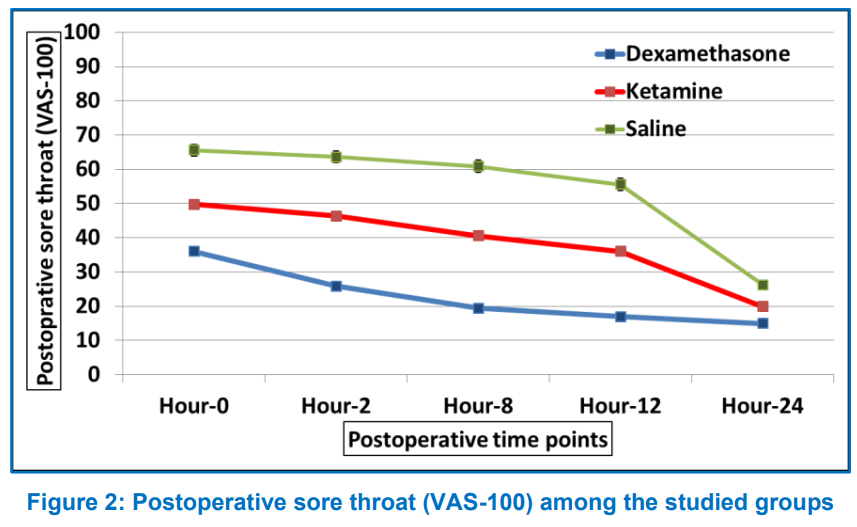
Postoperative sore throat score was measured on VAS, and it was significantly lower with both ketamine and dexamethasone compared with saline, while VAS scores were significantly lower in the dexamethasone group compared with ketamine group (Table 2 and Figure 2).
The incidence of postoperative odynophagia, the hoarseness of voice and PONV was significantly lower in the dexamethasone group compared with the saline group, with no statistically significant differences between ketamine and each of the dexamethasone and saline groups (Table 3).
The objective of the current research was to evaluate the efficacy of nebulized dexamethasone versus nebulized ketamine in alleviating post-operative sore throat after inserting a nasogastric tube in laparoscopic surgery. Postoperative pain scores were lower with nebulized ketamine and nebulized dexamethasone than with nebulized saline and significantly lower with dexamethasone when compared with ketamine. The incidence of odynophagia, hoarseness of voice, and PONV were less with nebulized dexamethasone compared to nebulized ketamine and nebulized saline.
No previous study compared the direct effect of nebulized dexamethasone versus nebulized ketamine in reducing complications of a nasogastric tube; however, the role of these drugs in reducing complications of POST after insertion of ETT has been investigated in previous studies. Corticosteroids lessen swelling, edema, fluid transudation, and irritation.9 An earlier investigation found that nebulized steroids are crucial in preventing POST by reducing the incidence and severity of sore throat and hoarseness following tracheal intubation in patients scheduled for thyroid surgery under general anesthesia.10 Other clinical trials to assess nebulized dexamethasone to prevent POST were conducted after the latter study. The findings of these studies corroborated the findings of the current analysis.
The incidence and severity of POST were considerably decreased in the nebulized dexamethasone group compared to the nebulized saline group at 2, 4, 8, and 12 h after extubation in a study conducted by Salama et al. in 2016. However, there was no significant difference after 24 h. Dexamethasone nebulization had not been associated with any complications.11
The study by Kumari et al. in 2019 was consistent with the present study’s findings regarding reduction in the incidence and severity of POST with nebulized dexamethasone. Patients in Group K received ketamine (preservative-free) 50 mg with 4 ml of normal saline for inhalation. In comparison, those in Group D received dexamethasone. Nebulization for 15 minutes was followed by induction. A 4-point scale was used to grade POST severity. Five patients (10%) in Group D and 14 patients (28%) in Group K experienced POST in that trial (P < 0.05).12
In a prospective interventional trial, Almustafa et al. (2020) divided 80 patients equally into two groups. One hour before surgery, participants in the dexamethasone group (D) received nebulized dexamethasone 8 mg, whereas those in the control group (S) received nebulized saline. A technique for comparing outcomes was employed to assess postoperative odynophagia, PONV, POST, and voice changes. When it came to voice changes, there was a substantial difference between the two groups (P = 0.001), with 19 (47.5%) of the saline group suffering a change of voice compared to only 4 (10.0%) in the dexamethasone group. There was no discernible difference between the groups regarding the PONV and the odynophagia occurrence. The incidence of POST was 27.5% compared to 72.5% in the dexamethasone and control groups respectively (P < 0.05).13
Due to its anti-nociceptive and anti-inflammatory properties, ketamine, an NMDA receptor antagonist, has been administered as a gargle or nebulizer to lessen the frequency and intensity of POST.14 Interestingly, a prior study by Nejati et al. (2010) supported intranasal ketamine in lowering pain related to nasogastric tube placement. Compared to lubricating gel alone, the researchers found that intranasal ketamine combined with lubricating gel was more effective at reducing pain during NG tube insertion in patients without major underlying illnesses.15
Ahuja et al. (2015) demonstrated a reduction in the incidence of POST with nebulized ketamine compared to nebulized saline, which was statistically significant only at 2 and 4 h postoperatively. They concluded that preoperative ketamine nebulization reduced the incidence and severity of POST, especially in the early postoperative hours.16
In another study, Amingad and Jayaram (2016) examined the effectiveness of preoperative ketamine administered through nebulization versus ketamine gargle in reducing POST. The researchers found that although there was no statistically significant difference between the groups, the frequency of POST was lower in the nebulized ketamine group than in the gargling group.17
Bhatta et al. (2020) measured the severity of sore throat in the postoperative care unit at 0 h, then in the ward every 2 h for 8 h, and finally at 24 h. Twelve patients in the saline group had a sore throat at 0 h, but only three patients in the ketamine group had a sore throat. The prevalence peaked at 4 h in the saline group, whereas in the ketamine group, it peaked at 6 h. At 24 h, 13 patients in the saline group still experienced sore throat, whereas only two patients in the ketamine group did.18
In contrast to the findings of the present investigation, Moustafa et al. (2018) conducted a prospective trial on three equal groups of children aged 6-16 y (36 patients each), undergoing surgery. Group K received 1 mg/kg of ketamine, Group D received 0.16 mg/kg of dexamethasone, and Group M received 40 mg/kg of magnesium sulphate by nebulization. Preoperative nebulization with ketamine was more effective in reducing the intensity of POST in pediatric patients postoperatively without systemic adverse effects.19
The discrepancy in results between the latter and current studies may be attributed to the differences in dosing methods. In the work of Mostafa et al. (2018), doses were based on mg /kg, while in the current study, the drugs were given in fixed doses.19
A study by Reddy and Fiaz in 2018 showed a dose-dependent effect of ketamine nebulization where doses of 1 mg/kg and 1.5 mg/kg were superior to 0.5 mg/kg. The fixed dosing method in the current study may have resulted in relatively smaller doses in some patients.20
First, the serum level of the drugs used in the study was not estimated, so we cannot exclude the systemic effect of these drugs on attenuating POST. Second, there is an overlap between the ETT and the NG tubes as possible causes for POST. For this reason, odynophagia was added as another outcome.
Moreover, the ETT was inserted under vision after lubrication with gel in a gentle manner by the most senior anesthesiologist available. Third, the scale used to assess POST was a subjective scale and this may be associated with bias.
The results of the current study revealed that preoperative nebulized dexamethasone as well as nebulized ketamine, both effective in reducing POST; however nebulized dexamethasone is more effective than the nebulized ketamine in this regard.
7. Availability of data and material
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.
8. Ethical considerations
This study was approved by the research ethics committee at the faculty of medicine, Ain Shams University (FMASU MD 99a / 2021 / 2022) and registered retrospectively with Pan African Clinical Trial Registry, identifier: PACTR202210590810112. Written informed consent was obtained from all patients.
9. Competing interests
The authors declare that there were no conflicts of interest.
10. Funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
11. Authors contribution
MZ: conduction of the study work.
SA: manuscript editing
SH, TS: Literature search
AH: Statistical analysis and review
Author affiliations:
- Mai Mohammed Zakaria, MSc, Assistant Lecturer of Anesthesia, Intensive Care & Pain Management, Faculty of Medicine, Ain Shams University, Nasr City, Cairo, Egypt; E-mail: mai.mohammed@med.asu.edu.eg
- Sahar Kamal Mohammed Aboulella, Professor of Anesthesia, Intensive Care & Pain Management, Faculty of Medicine, Ain Shams University, Nasr City, Cairo, Egypt; Email: Sahar.aboulella@hotmail.com
- Sahar Mohammed Kamal Hassanein, Professor of Anesthesia, Intensive Care & Pain Management, Faculty of Medicine, Ain Shams University, Nasr City, Cairo, Egypt; E-mail: Kamalsahar90@gmail.com
- Ahmed Mohammed Elsayed El Hennawy, Professor of Anesthesia, Intensive Care & Pain Management, Faculty of Medicine, Ain Shams University, Nasr City, Cairo, Egypt; E-mail: Anahenno@yahoo.com
- Tarek Samir Salah El Din Shabana, MD, Lecturer of Anesthesia, Intensive Care & Pain Management, Faculty of Medicine, Ain Shams University, Nasr City, Cairo, Egypt; E-mail: tarek.shabana@hotmail.com
ABSTRACT
Background & objective: Nasogastric (NG) tube insertion is a frequently performed medical procedure. Most of the time, the oropharyngeal discomfort is usually underestimated, and insertions are carried out with just regular lubricant jelly and no additional painkillers, which results in less-than-ideal pain management. We compared the effectiveness of preemptive use of nebulized ketamine and dexamethasone in preventing post-operative sore throat following NG tube insertion in laparoscopic surgery.
Methods: This prospective randomized double-blind controlled study was carried on 108 patients of both sexes with ASA physical status I-II. aged 20-60 years, undergoing laparoscopic abdominal surgeries under general anesthesia. Patients were randomized into 3 equal groups. Group D received a dose of 8 mg nebulized dexamethasone. Group K received 50 mg nebulized ketamine. Group S received 5 ml of nebulized saline. NG tube was passed after induction of general anesthesia. Postoperative sore throat was enquired from the patients at full recovery (zero hour), then at 2, 8, 12 and 24 h. Computer software (SPSS 15.0.1. for Windows; SPSS Inc, Chicago, IL, 2001) was used for data analysis. Non-parametric quantitative data, median, range, percentages, and numbers are given for qualitative data. The appropriate analysis was conducted in line with the data obtained. P < 0.05 was regarded as significant.
Results: The incidence of postoperative sore throat (POST) was lower with both nebulized dexamethasone and nebulized ketamine compared with nebulized saline; and significantly lower with dexamethasone compared with ketamine at 0 h (P < 0.001), 2 h (P < 0.001), 8 h (P < 0.001), 12 h (P < 0.001), and 24 h (P < 0.001).
Conclusion: The current study revealed that preoperative nebulized dexamethasone was more effective than nebulized ketamine in reducing postoperative sore throat.
Abbreviations: NG- Nasogastric; NMDA- N-Methyl-D-Aspartate; PONV- Postoperative Nausea and Vomiting; POST- Postoperative Sore Throat; VAS- Visual Analogue Scale
Key words: Nebulization; Dexamethasone; Ketamine; Laparoscopic Surgery; Nasogastric Tube
Citation: Zakaria MM, Mohammed Aboulella SK, Hassanein SMK, Elsayed El Hennawy AM, Salah El Din Shabana TS. Role of preoperative dexamethasone nebulization versus ketamine nebulization in reducing complications of nasogastric tube after laparoscopic surgery. Anaesth. pain intensive care 2024;28(1):62-67.
DOI: 10.35975/apic.v28i1.2275
Received: 22 July, 2023; Reviewed: 04 October 2023; Accepted: 30 October 2023
1. INTRODUCTION
In the clinical setting, nasogastric (NG) tube insertions are frequent medical procedures. Most of the time, the oropharyngeal discomfort is usually underestimated, and insertions are carried out with regular lubricant jelly and no additional painkillers, which results in less-than-ideal pain management.1
After general anesthesia and endotracheal intubation, postoperative sore throat (POST) is a common postoperative consequence. Both pharmaceutical and nonpharmacological approaches have been used to treat POST.2 In laparoscopic surgery, NG tubes are frequently used to decompress the stomach. POST severity increases when a nasogastric tube is used in conjunction with endotracheal intubation.3
Steroids have anti-inflammatory functions and are widely used in common practice. The inhaled corticosteroids deliver the drug to the site of action without much systemic side effects. Dexamethasone is a potent synthetic glucocorticoid with anti-inflammatory effects. It has been reported that dexamethasone effectively treats sore throat.4 Few clinical trials have evaluated the use of dexamethasone as a measure to reduce the mechanical impact of commonly used orally inserted devices. Corticosteroids are known to reduce inflammation, fluid transudation, edema and reduce pain severity.5
N-methyl-D-aspartate (NMDA) receptors play a significant role in nociception and inflammation in the human body. NMDA receptors are found in the central nervous system and peripheral nerves.6 Due to its anti-nociceptive and anti-inflammatory properties, ketamine, an N-methyl-D-aspartate (NMDA) receptor antagonist, has been administered as a gargle or nebulizer to lessen the frequency and intensity of POST.7 Ketamine nebulization is superior to ketamine gargle since the latter uses more of the drug and poses a danger of aspiration in addition to having a more unpleasant taste.8
We conducted this study to compare the efficacy of nebulization of dexamethasone with ketamine in the oropharynx of the patients before the induction of the general anesthesia, in reducing the postoperative sore throat related to nasogastric tube insertion.
2. METHODOLOGY
One hundred and eight patients of both sexes with ASA physical status I-II, aged 20-60 years, who were undergoing laparoscopic abdominal surgeries under general anesthesia participated in this prospective randomized, double-blind controlled study. Approval from the local ethics committee of Ain Shams University and written informed consent from the patient or their representatives was obtained.
Patients with an ASA physical status III or higher, Mallampati > III, or multiple intubation attempts, history of an allergy to the study drug, surgeries lasting less than 30 min, heavy smokers, patients who had undergone more than one suction procedure, patients with esophageal pathologies, patients who had undergone laryngeal or pharyngeal surgery, patients who had recently experienced a respiratory tract infection or sore throat were excluded.
2.1. Randomization
Patients were randomized into three equal groups, 36 each, using a computer-generated random numbers table. Group D received 8 mg dexamethasone (2 ml added to 3 ml saline making a total of 5 ml). Group K received 50 mg ketamine (1ml added to 4 ml saline) and Group S received 5 ml of nebulized saline as a control group.
One of the anesthesiologists not involved in the ongoing research prepared and administered the 5 ml formulations. Before the induction of anesthesia, patients received the study medication through a nebulizer mask attached to an oxygen-driven source mounted on a wall (8 L of O2 per min) for 15 min.
Routine monitoring was done in the operating room including an electrocardiogram, a pulse oximeter, a non-invasive blood pressure monitor, and a capnometer. To induce anesthesia and aid endotracheal intubation, propofol 2 mg/kg, fentanyl 2 μg/kg, and atracurium 0.5 mg/kg were administered intravenously. Isoflurane 1-2% was used to maintain anesthesia, and top-up doses of atracurium 0.1 mg/kg were administered every 20 min. Endotracheal tube (ETT) was inserted. End-tidal carbon dioxide was maintained between 30-35 mmHg using mechanical ventilation adjustments. An experienced anesthesiologist gently placed 18-Fr nasogastric tube under vision after lubricating with jelly. Postoperative pain was managed with paracetamol 1 g IV every 6 h for 24 h postoperatively.
The duration of the nasogastric tube insertion was noted, and the total surgical time was estimated from the moment the anesthetic was induced until the patient was extubated. At the end of the surgery, the inhalational anesthetic was stopped, the muscle relaxant was reversed, and the extubation was done when the patient was fully conscious.
The study assessed several outcomes, including POST, odynophagia (pain when swallowing), postoperative nausea and vomiting, and hoarseness of voice, that could be associated with nasogastric tube insertion. Sore throat was evaluated at 0 h (at recovery when the patient can be tested), and at 2, 8, 12, and 24 h.
| Table 1: Baseline characteristics of the studied groups | |||||
| Variables | Measure | Dexamethasone (n = 36) | Ketamine
(n = 36) |
Saline
(n = 36) |
p-value |
| Age (y) | Mean ± SD | 37.5 ± 6.2 | 37.1 ± 5.6 | 36.8 ± 5.7 | ^0.898 |
| Range | 26.0–51.0 | 26.0–50.0 | 21.0–46.0 | ||
| Sex [n (%)] | Male | 16 (44.4%) | 15 (41.7%) | 13 (36.1%) | #0.765 |
| Female | 20 (55.6%) | 21 (58.3%) | 23 (63.9%) | ||
| Weight (kg) | Mean ± SD | 81.3 ± 12.8 | 77.8 ± 11.7 | 81.4 ± 11.7 | ^0.358 |
| Range | 57.2–108.4 | 54.1–107.9 | 56.4–107.2 | ||
| ASA [n (%)] |
I | 25 (69.4%) | 28 (77.8%) | 30 (83.3%) | #0.372 |
| II | 11 (30.6%) | 8 (22.2%) | 6 (16.7%) | ||
| Operation time (min) | Mean ± SD | 83.2 ± 12.0 | 79.4 ± 12.4 | 81.2 ± 17.8 | ^0.541 |
| Range | 63.0–110.0 | 53.0–106.0 | 51.0–116.0 | ||
| (*) significant p-value < 0.05 ^ANOVA test. *Significant. Homogenous groups had the same symbol (a,b,c) based on the post hoc Bonferroni test. | |||||
POST related pain was measured using the Visual Analogue Scale (VAS) score.
Using a binary scale (yes or no), postoperative hoarseness of voice, odynophagia, postoperative nausea and vomiting (PONV) were evaluated.
2.2. Primary and secondary outcomes
The primary outcome was the comparison of postoperative sore throat using the VAS score between the three groups.
The secondary outcome assessed the rate [n (%)] of odynophagia, hoarseness of voice, and PONV between the three groups.
2.3. Sample size calculation
Using the G power software, calculate sample size, power is 80%, and alpha error is 5%. Reviewing the findings of an earlier pertinent investigation (Mostafa et al., 2018) revealed a medium effect size difference (0.3) regarding the incidence of POST among various intervention groups. A sample size of at least 36 patients per group was required in light of these findings.
2.4. Statistical analysis
Using a statistical tool for social research, the acquired data was updated, coded, and entered into a computer software (SPSS 15.0.1. for Windows; SPSS Inc, Chicago, IL, 2001). The mean and standard deviation (SD) were reported for quantitative data. Non-parametric quantitative data, median, range, percentages, and numbers are given for qualitative data. The appropriate analysis was conducted in line with the data obtained. P < 0.05 was regarded as significant.
| Table 2: Postoperative sore throat (VAS-100) among the studied groups | |||||
| Time | Measure | Dexamethasone (n = 36) | Ketamine
(n = 36) |
Saline
(n = 36) |
^p-value |
| Hour-0 | Mean ± SD | 36.0 ± 4.9 a | 49.7 ± 5.5 b | 65.6 ± 8.4 c | < 0.001* |
| Range | 30.0–45.0 | 40.0–60.0 | 55.0–85.0 | ||
| Hour-2 | Mean ± SD | 25.8 ± 4.7 a | 46.4 ± 4.6 b | 63.6 ± 8.4 c | < 0.001* |
| Range | 20.0–35.0 | 35.0–50.0 | 50.0–80.0 | ||
| Hour-8 | Mean ± SD | 19.4 ± 5.4 a | 40.6 ± 6.1 b | 60.8 ± 9.0 c | < 0.001* |
| Range | 15.0–30.0 | 25.0–50.0 | 45.0–75.0 | ||
| Hour-12 | Mean ± SD | 16.9 ± 5.4 a | 36.0 ± 6.5 b | 55.6 ± 8.8 c | < 0.001* |
| Range | 10.0–25.0 | 20.0–45.0 | 40.0–35.0 | ||
| Hour-24 | Mean ± SD | 15.0 ± 4.9 a | 19.9 ± 6.4 b | 26.3 ± 5.8 c | < 0.001* |
| Range | 10.0–25.0 | 10.0–30.0 | 15.0–35.0 | ||
| (*) significant p-value < 0.05 ^ANOVA test. *Significant. Homogenous groups had the same symbol (a,b,c) based on the post hoc Bonferroni test. | |||||
| Table 3: Postoperative complications among the studied groups | ||||
| Complications | Dexamethasone
(n = 36) |
Ketamine
(n = 36) |
Saline
(n = 36) |
#p-value |
| Odynophagia | 2 (5.6%) a | 7 (19.4%) a,b | 12 (33.3%) b | 0.012* |
| Hoarseness | 1 (2.8%) a | 5 (13.9%)a,b | 9 (25.0%) b | 0.024* |
| PONV | 0 (0.0%) a | 1 (2.8%) a,b | 6 (16.7%) b | 0.009* |
| (*) significant P < 0.05, #Chi square test. *Significant. Homogenous groups had the same symbol (a,b) based on the post hoc Bonferroni test. | ||||
3. RESULTS
A total of 161patients were assessed for eligibility, as shown in Figure 1, out of which 53 patients were excluded so total number randomized and analyzed was 108 patients, equally divided into 36 patients in each group.
There was no statistically significant difference between the studied groups regarding baseline characteristics: age, sex, weight, ASA, and operation duration (Table 1).
Postoperative sore throat score was measured on VAS, and it was significantly lower with both ketamine and dexamethasone compared with saline, while VAS scores were significantly lower in the dexamethasone group compared with ketamine group (Table 2 and Figure 2).
The incidence of postoperative odynophagia, the hoarseness of voice and PONV was significantly lower in the dexamethasone group compared with the saline group, with no statistically significant differences between ketamine and each of the dexamethasone and saline groups (Table 3).
4. DISCUSSION
The objective of the current research was to evaluate the efficacy of nebulized dexamethasone versus nebulized ketamine in alleviating post-operative sore throat after inserting a nasogastric tube in laparoscopic surgery. Postoperative pain scores were lower with nebulized ketamine and nebulized dexamethasone than with nebulized saline and significantly lower with dexamethasone when compared with ketamine. The incidence of odynophagia, hoarseness of voice, and PONV were less with nebulized dexamethasone compared to nebulized ketamine and nebulized saline.
No previous study compared the direct effect of nebulized dexamethasone versus nebulized ketamine in reducing complications of a nasogastric tube; however, the role of these drugs in reducing complications of POST after insertion of ETT has been investigated in previous studies. Corticosteroids lessen swelling, edema, fluid transudation, and irritation.9 An earlier investigation found that nebulized steroids are crucial in preventing POST by reducing the incidence and severity of sore throat and hoarseness following tracheal intubation in patients scheduled for thyroid surgery under general anesthesia.10 Other clinical trials to assess nebulized dexamethasone to prevent POST were conducted after the latter study. The findings of these studies corroborated the findings of the current analysis.
The incidence and severity of POST were considerably decreased in the nebulized dexamethasone group compared to the nebulized saline group at 2, 4, 8, and 12 h after extubation in a study conducted by Salama et al. in 2016. However, there was no significant difference after 24 h. Dexamethasone nebulization had not been associated with any complications.11
The study by Kumari et al. in 2019 was consistent with the present study’s findings regarding reduction in the incidence and severity of POST with nebulized dexamethasone. Patients in Group K received ketamine (preservative-free) 50 mg with 4 ml of normal saline for inhalation. In comparison, those in Group D received dexamethasone. Nebulization for 15 minutes was followed by induction. A 4-point scale was used to grade POST severity. Five patients (10%) in Group D and 14 patients (28%) in Group K experienced POST in that trial (P < 0.05).12
In a prospective interventional trial, Almustafa et al. (2020) divided 80 patients equally into two groups. One hour before surgery, participants in the dexamethasone group (D) received nebulized dexamethasone 8 mg, whereas those in the control group (S) received nebulized saline. A technique for comparing outcomes was employed to assess postoperative odynophagia, PONV, POST, and voice changes. When it came to voice changes, there was a substantial difference between the two groups (P = 0.001), with 19 (47.5%) of the saline group suffering a change of voice compared to only 4 (10.0%) in the dexamethasone group. There was no discernible difference between the groups regarding the PONV and the odynophagia occurrence. The incidence of POST was 27.5% compared to 72.5% in the dexamethasone and control groups respectively (P < 0.05).13
Due to its anti-nociceptive and anti-inflammatory properties, ketamine, an NMDA receptor antagonist, has been administered as a gargle or nebulizer to lessen the frequency and intensity of POST.14 Interestingly, a prior study by Nejati et al. (2010) supported intranasal ketamine in lowering pain related to nasogastric tube placement. Compared to lubricating gel alone, the researchers found that intranasal ketamine combined with lubricating gel was more effective at reducing pain during NG tube insertion in patients without major underlying illnesses.15
Ahuja et al. (2015) demonstrated a reduction in the incidence of POST with nebulized ketamine compared to nebulized saline, which was statistically significant only at 2 and 4 h postoperatively. They concluded that preoperative ketamine nebulization reduced the incidence and severity of POST, especially in the early postoperative hours.16
In another study, Amingad and Jayaram (2016) examined the effectiveness of preoperative ketamine administered through nebulization versus ketamine gargle in reducing POST. The researchers found that although there was no statistically significant difference between the groups, the frequency of POST was lower in the nebulized ketamine group than in the gargling group.17
Bhatta et al. (2020) measured the severity of sore throat in the postoperative care unit at 0 h, then in the ward every 2 h for 8 h, and finally at 24 h. Twelve patients in the saline group had a sore throat at 0 h, but only three patients in the ketamine group had a sore throat. The prevalence peaked at 4 h in the saline group, whereas in the ketamine group, it peaked at 6 h. At 24 h, 13 patients in the saline group still experienced sore throat, whereas only two patients in the ketamine group did.18
In contrast to the findings of the present investigation, Moustafa et al. (2018) conducted a prospective trial on three equal groups of children aged 6-16 y (36 patients each), undergoing surgery. Group K received 1 mg/kg of ketamine, Group D received 0.16 mg/kg of dexamethasone, and Group M received 40 mg/kg of magnesium sulphate by nebulization. Preoperative nebulization with ketamine was more effective in reducing the intensity of POST in pediatric patients postoperatively without systemic adverse effects.19
The discrepancy in results between the latter and current studies may be attributed to the differences in dosing methods. In the work of Mostafa et al. (2018), doses were based on mg /kg, while in the current study, the drugs were given in fixed doses.19
A study by Reddy and Fiaz in 2018 showed a dose-dependent effect of ketamine nebulization where doses of 1 mg/kg and 1.5 mg/kg were superior to 0.5 mg/kg. The fixed dosing method in the current study may have resulted in relatively smaller doses in some patients.20
5. LIMITATIONS
First, the serum level of the drugs used in the study was not estimated, so we cannot exclude the systemic effect of these drugs on attenuating POST. Second, there is an overlap between the ETT and the NG tubes as possible causes for POST. For this reason, odynophagia was added as another outcome.
Moreover, the ETT was inserted under vision after lubrication with gel in a gentle manner by the most senior anesthesiologist available. Third, the scale used to assess POST was a subjective scale and this may be associated with bias.
6. CONCLUSION
The results of the current study revealed that preoperative nebulized dexamethasone as well as nebulized ketamine, both effective in reducing POST; however nebulized dexamethasone is more effective than the nebulized ketamine in this regard.
7. Availability of data and material
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.
8. Ethical considerations
This study was approved by the research ethics committee at the faculty of medicine, Ain Shams University (FMASU MD 99a / 2021 / 2022) and registered retrospectively with Pan African Clinical Trial Registry, identifier: PACTR202210590810112. Written informed consent was obtained from all patients.
9. Competing interests
The authors declare that there were no conflicts of interest.
10. Funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
11. Authors contribution
MZ: conduction of the study work.
SA: manuscript editing
SH, TS: Literature search
AH: Statistical analysis and review
12. REFERENCES
- Czarnecki ML, Turner HN, Collins PM, Doellman D, Wrona S, Reynolds J. Procedural pain management: a position statement with clinical practice recommendations. Pain Manag Nurs. 2011 Jun;12(2):95-111. [PubMed] DOI: 1016/j.pmn.2011.02.003
- Sumathi PA, Shenoy T, Ambareesha M, Krishna HM. Controlled comparison between betamethasone gel and lidocaine jelly applied over tracheal tube to reduce postoperative sore throat, cough, and hoarseness of voice. Br J Anaesth. 2008 Feb;100(2):215-8. [PubMed] DOI: 1093/bja/aem341
- Thomsen TW, Shaffer RW, Setnik GS. Videos in clinical medicine. Nasogastric intubation. N Engl J Med. 2006 Apr 27;354(17):e16. [PubMed] DOI: 1056/NEJMvcm050183
- Zhao X, Cao X, Li Q. Dexamethasone for the prevention of postoperative sore throat: a systematic review and meta-analysis. J Clin Anesth. 2015 Feb;27(1):45-50. [PubMed] DOI: 1016/j.jclinane.2014.06.014
- Ashwini H, Seema Kumari K, Lavanya R. Comparative study of dexamethasone nebulisation with magnesium sulphate nebulization in preventing post operative sore throat following endotracheal intubation. Indian J Clin Anaesth. 2018;5(3):341-347. DOI: 18231/2394-4994.2018.0065
- Lin CY, Tsai PS, Hung YC, Huang CJ. L-type calcium channels are involved in mediating the anti-inflammatory effects of magnesium sulphate. Br J Anaesth. 2010 Jan;104(1):44-51. [PubMed] DOI: 1093/bja/aep336
- Chan L, Lee ML, Lo YL. Postoperative sore throat and ketamine gargle. Br J Anaesth. 2010 Jul;105(1):97. [PubMed] DOI: 1093/bja/aeq152
- Ahuja V, Mitra S, Sarna R. Nebulized ketamine decreases incidence and severity of post-operative sore throat. Indian J Anaesth. 2015 Jan;59(1):37-42. [PubMed] DOI: 4103/0019-5049.149448
- Kulkarni LM, Holyachi R, Kurdi MS. Vegetable gum based gel lubrication of endotracheal tube cuffs improves efficacy of alkalinized intracuff lignocaine in preventing postoperative sore throat: A randomized controlled study. Anaesth. pain intensive care 2016;20(4):422-428 [FreeFullText]
- Chen YQ, Li JP, Xiao J. Prophylactic effectiveness of budesonide inhalation in reducing postoperative throat complaints. Eur Arch Otorhinolaryngol. 2014 Jun;271(6):1667-72. [PubMed] DOI: 1007/s00405-014-2896-7
- Salama AK, El-badawy AM. Does nebulized dexamethasone decrease the incidence of postextubation sore throat?: a randomized controlled study. Ain-Shams J Anaesthesiol. 2016;9:104–107.
- Kumari S, Bhashyam S, Lakshmi B. Effects of Nebulized Dexamethasone Versus Nebulized Ketamine on the Attenuation of Post-operative Sore Throat Following Endotracheal Intubation. Int J Sci Study. 2019;7(9):546-556. [FreeFullText]
- Almustafa M, Obeidat F, Mismar A, Rashdan M, Jabaiti K, Alryalat SA, Al-Hardan D, Suleiman A. Role of Preoperative Dexamethasone Nebulization in Reducing Bougie Complications Encountered After Sleeve Gastrectomy: a Prospective Double-Blind Control Interventional Study. Obes Surg. 2020 Feb;30(2):501-506. [PubMed] DOI: 1007/s11695-019-04202-x
- Chan L, Lee ML, Lo YL. Postoperative sore throat and ketamine gargle. Br J Anaesth. 2010 Jul;105(1):97. [PubMed] DOI: 1093/bja/aeq152
- Nejati A, Golshani K, Moradi Lakeh M, Khashayar P, Moharari RS. Ketamine improves nasogastric tube insertion. Emerg Med J. 2010 Aug;27(8):582-5. [PubMed] DOI: 1136/emj.2009.075275
- Ahuja V, Mitra S, Sarna R. Nebulized ketamine decreases incidence and severity of post-operative sore throat. Indian J Anaesth. 2015 Jan;59(1):37-42. [PubMed] DOI: 4103/0019-5049.149448
- Amingad B, Jayaram S, Comparison of ketamine nebulisation with ketamine gargle in attenuating post-operative sore throat. Indian J Clin Anaesth. 2016;3(3):347-351. [FreeFullText]
- Bhatta PD, Shakya BM, Bista NR, Marhatta MN, Shrestha N. Effect of preoperative nebulized ketamine on incidence and severity of postoperative sore throat in patient undergoing general anaesthesia with endotracheal intubation. JIOM Nepal. 2020; 42(1):12-6. [FreeFullText]
- Mostafa RH, Saleh AN, Hussein MM. A comparative study of three nebulized medications for the prevention of postoperative sore throat in the pediatric popula tion. Open Anesthe J. 2018;12(1):85-97. DOI: 2174/2589645801812010085
- Reddy M, Fiaz S. Dose-dependent effectiveness of ketamine nebulisation in preventing post-operative sore throat due to tracheal intubation. Sri Lankan J Anaesthesiol. 2018;26(1):22-27. DOI: 10.4038/slja.v26i1.8264