Diogo S Miguel, MD, Patrícia Ramos, MD, Jorge Oliveira, PhD, Cristina Ferreira, MD, Fátima Cruz, MD
Diogo S Miguel, MD
Serviço de Anestesiologia, Centro Hospitalar Universitário do Porto, Porto, (Portugal)
diogo.silva.miguel@gmail.com
Patrícia Ramos, MD
Serviço de Anestesiologia, Centro Hospitalar Universitário do Porto, Porto, (Portugal)
patriciasant@gmail.com
Jorge Oliveira, PhD
Centre for the Research and Technology of Agro-Environmental and Biological Science, University of Trás-os-Montes e Alto Douro, Vila Real, Portugal; Polytechnic Institute of Viseu, Viseu, (Portugal)
joliveira@esav.ipv.pt
Cristina Ferreira, MD
Serviço de Anestesiologia, Centro Hospitalar Universitário do Porto, Porto, (Portugal)
crispintoferreira@gmail.com
Fátima Cruz, MD
Serviço de Anestesiologia, Centro Hospitalar Universitário do Porto, Porto, (Portugal)
mfatimabcruz@gmail.com
Correspondence: Diogo S Miguel, MD Serviço de Anestesiologia, Centro Hospitalar do Porto Largo Prof. Abel Salazar 4099-001 Porto (Portugal)
Phone: +351 22 2077549
E-mail: diogo.silva.miguel@gmail.com
ABSTRACT
Background: Obesity is an important public health problem, with a high prevalence worldwide. Bariatric surgery emerged as an effective therapeutic tool, with improvement of quality of life and a decrease in all-cause mortality. Obesity Surgery Mortality Risk Score (OS-MRS) predicts 90-day mortality after bariatric surgery, but its association with hospital length of stay (LOS) has not been elucidated. We aimed to evaluate the association between OS-MRS and LOS after gastric bypass surgery.
Methodology: We retrieved clinical and demographic data of 474 patients who had been submitted to gastric bypass surgery for this retrospective audit at Hospital de Santo António, Centro Hospitalar Universitário do Porto, Porto, (Portugal), between January 2010 and May 2015. The patients were classified as Class A, B or C. The primary goal was to evaluate whether there was an association between OS-MRS and LOS after gastric bypass surgery. The study of the relationship between duration of surgery (DS) and LOS was also performed.
Results: After application of exclusion criteria, 402 patients were included in the statistical analysis (172 patients Class A, 187 Class B and 43 Class C). Patients classified as OS-MRS Class A had a significant shorter LOS (3.5 ± 2.3 days) than patients classified as Class B (4.2 ± 5.1 days) and Class C (5.7 ± 12.6 days; p<0.001). A significant positive correlation between DS and LOS was observed, although the degree of that correlation was weak (ρ=0.203; p=0.001).
Conclusion: A positive association of OS-MRS with hospital length of stay and duration of surgery was observed; the patients with higher OS-MRS classes had longer length of stay in the hospital and longer duration of surgery. Moreover, longer length of stay was slightly associated with longer surgery duration.
Key words: Obesity; Bariatric surgery; Hospital length of stay; Obesity, Morbid/surgery; Obesity surgery mortality risk score; OS-MRS
Citation: Miguel DS, Ramos P, Oliveira J, Ferreira C, Cruz F. OS-MRS as a predictor of hospital length of stay – a retrospective audit of patients submitted to elective gastric bypass surgery. Anaesth pain intensive care 2020;24(1):_
DOI: https://DOI.org/10.35975/apic.v2i1.
Received – 29 November 2019; Reviewed –24 January, 8 February 2020; Revised – 24 January 2020; Accepted – 8 February 2020
INTRODUCTION
Obesity is nowadays recognised as an important public health problem, having achieved epidemic proportions. According to World Health Organization, in 2016 the world prevalence of obesity among adults was around 39%,1 and the same organization estimates that every year at least 2.8 million people die worldwide as a result of being overweight or obese.
Among the therapeutic options to deal with obesity, there have been some surgical approaches that aim to promote weight loss. Indeed, bariatric surgery can have an important positive impact in obese patients, leading to sustained weight loss, improvement of obesity related comorbidities.2-4 better quality of life,5 and ultimately a decrease of all-cause mortality.6
To access and stratify the risk of patients submitted to bariatric surgery, DeMaria et al. proposed a clinical score to predict 90-day mortality. Obesity Surgery Mortality Risk Score (OS-MRS) ranges from 0 to 5, with 1 point attributed per each of 5 variables: Body Mass Index (BMI) > 50 Kg/m2, arterial hypertension, male sex, age > 45 years old and risk factors for pulmonary thromboembolism (previous venous thromboembolism, previous inferior vena cava filter placement, history of right heart failure or pulmonary hypertension and/or history or physical findings of venous stasis). Patients may be classified as Class A (OS-MRS=0-1), B (OS-MRS=2-3) or C (OS-MRS=4-5), with expected mortality of 0.31%, 1.90% or 7.56%, respectively.7 After the first study by DeMaria et al., several other authors validated the OS-MRS as a useful score to predict 90-day mortality after bariatric surgery.8-11
Several authors have studied the OS-MRS relation with surgical complications, with contradicting results: while Sarela et al.12 and Lorente et al.13 have found an association with complications rate, several others have not replicated these results.14-17
However, the evidence regarding the association of OS-MRS with hospital length of stay (LOS) is still scarce, and the authors of this article could only found one study in which both OS-MRS and POSSUM scores were found to be moderately accurate for predicting inpatient stay longer than 3 days.16
In this study 474 patients submitted to gastric bypass surgery were retrospectively audited. The primary goal was to evaluate whether there was an association between OS-MRS and LOS after gastric bypass surgery. Additionally, the relationship between LOS and duration of surgery (DS) was also accessed.
METHODOLOGY
After approval by the institutional review board (114-15; 102-DEFI/NA-CES), a retrospective audit was conducted in a Portuguese tertiary university and central hospital (Hospital de Santo António, Centro Hospitalar Universitário do Porto, Porto, Portugal) between January 2010 and May 2015. Clinical and demographic data were collected, namely: age, gender, American Society of Anaesthesiology (ASA) Physical Status Classification, weight, height, OS-MRS, LOS and 90-day outcome. Patients with incomplete records, submitted to laparotomy or other bariatric procedures than gastric bypass were excluded. According to OS-MRS, the patients were classified as OS-MRS Class A, B or C.7
Normality of distribution of continuous variables was tested with Kolmogorov-Smirnov test. Accordingly, to analyse the influence of OS-MRS Class on LOS, the non-parametric Kruskal-Wallis with Dunn's post-hoc test was performed. Spearman correlation test was used to study the relationship between SL and LOS. Categorical data were analysed using the χ2 test.
The statistical analysis was performed using SPSS® version 23. A p < 0.05 was considered statistically significant.
RESULTS
A total of 474 patients were submitted to a gastric bypass between January 2010 and May 2015. After exclusion criteria, 402 patients were enrolled, and included in three groups, based on OS-MRS Class: 172 patients were classified as Class A, 187 as Class B and 43 as Class C (Figure 1).
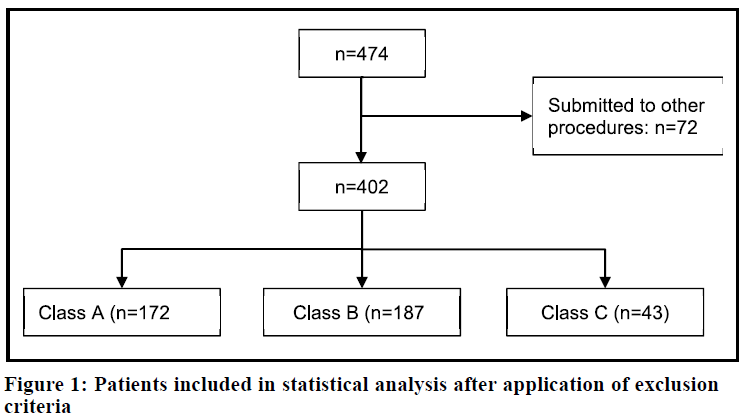
Table 1 shows the demographic and clinical data. Gender and age were statistically different between groups, while no differences were found in ASA classification and BMI. Moreover, SL was progressively longer with increasing OS-MRS Class, with the difference between Class A and Class C showing statistical significance.
Table 1: Demographic and clinical data
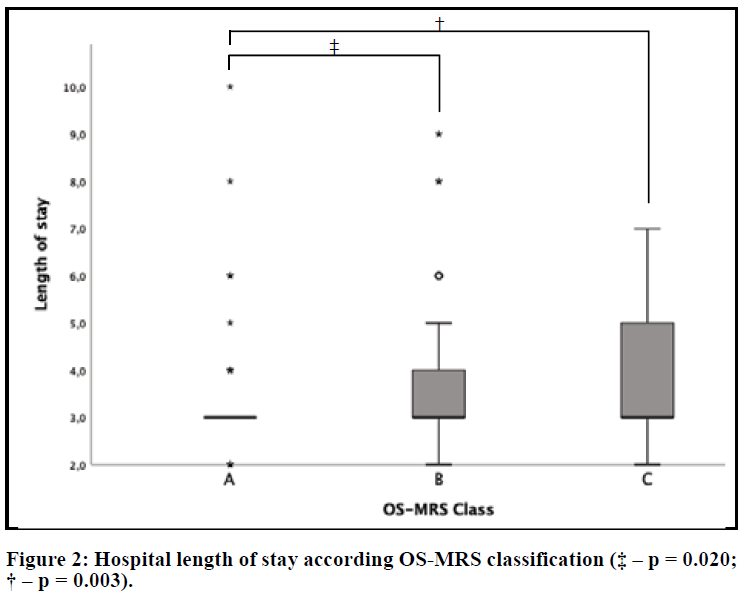
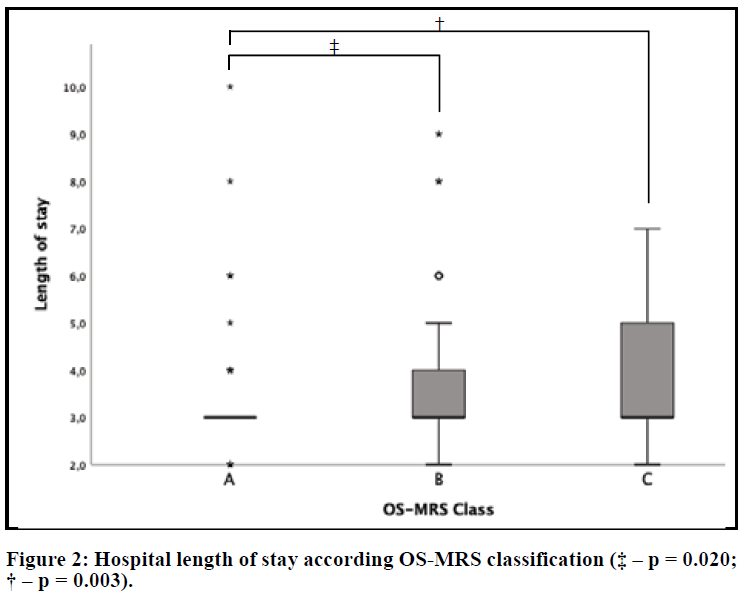
Regarding the primary goal of this study, patients classified as OS-MRS Class A had a statistically significant shorter LOS (3.5 ± 2.3 days) than patients classified as Class B (4.2 ± 5.1 days) and Class C (5.7 ± 12.6 days; p=0.001). The difference between patients classified as Class B and Class C was not statistically different (Figure 2).
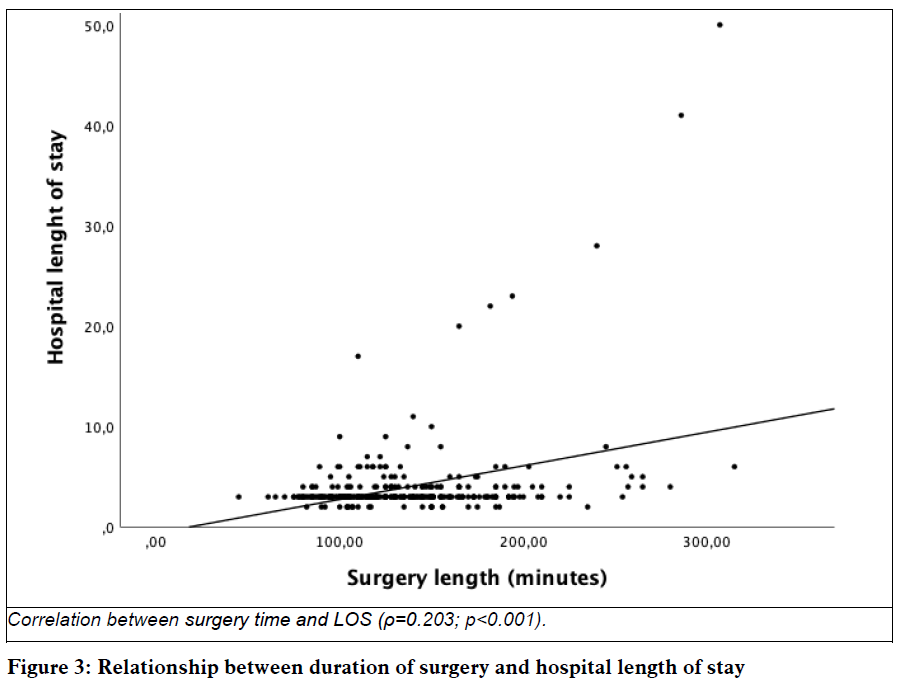
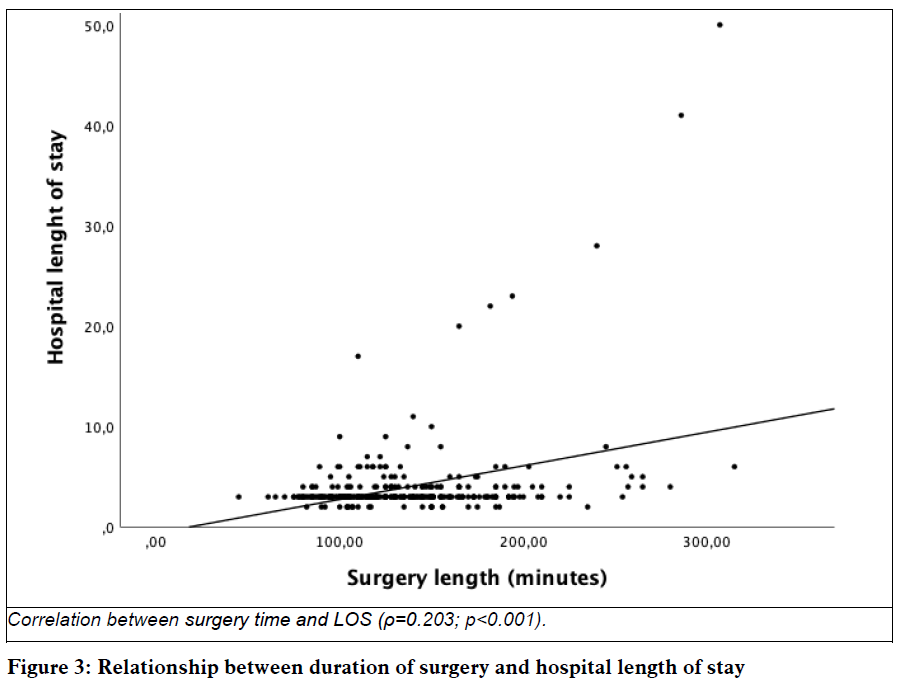
The study of the relationship between SL and LOS was also performed (Figure 3). Although there is a statistically significant correlation between both variables, the degree of that correlation is weak (ρ = 0.203; p < 0.001).
DISCUSSION
There is a positive association between OS-MRS class and LOS, with patients with higher classes having longer hospital stay.
Our results are aligned with a previous work by Gilhooly et al., which showed that both OS-MRS and POSSUM scores were moderately accurate for predicting stay of 3 or more days due to morbidity and poor mobility.16
Our study has also found a positive correlation between the SL and LOS. In addition, SL was also progressively longer with increasing OS-MRS class. This finding may be justified with the assumption that the patients with higher OS-MRS class might represent greater technical difficulty for the surgeon, thus increasing the procedure time. Therefore, both the complexity of the patient and the difficulty of the procedure may explain the longer LOS.
STUDY LIMITATIONS
Being a retrospective audit, randomization and investigational unawareness were not included. Thus, a prospective, double blind randomized trial may add information to the results shown in this study.
The discharge criteria have not been strictly defined. Furthermore, the clinical records were in many cases incomplete and did not allow a more extensive and complete data collection regarding patient’s clinical characteristics and their evolution following surgery.
In addition, this was a single centre study, which may affect the generalization of the conclusions.
CONCLUSIONS
A positive association of OS-MRS with hospital length of stay and duration of surgery was observed, with patients with higher OS-MRS classes having longer length of stay and had longer duration of surgery. Moreover, longer length of stay was slightly associated with longer surgery duration.
Conflict of interest: None declared by the authors.
Authors’ contribution:
DM: Concept, bibliography review, data collection, statistical analysis, manuscript editing
PR: Concept, bibliography review, data collection, manuscript editing
JO: Concept, statistical analysis, manuscript editing
CF, FC: Concept, bibliography review, manuscript review, final approval
REFERENCES
Diogo S Miguel, MD
Serviço de Anestesiologia, Centro Hospitalar Universitário do Porto, Porto, (Portugal)
diogo.silva.miguel@gmail.com
Patrícia Ramos, MD
Serviço de Anestesiologia, Centro Hospitalar Universitário do Porto, Porto, (Portugal)
patriciasant@gmail.com
Jorge Oliveira, PhD
Centre for the Research and Technology of Agro-Environmental and Biological Science, University of Trás-os-Montes e Alto Douro, Vila Real, Portugal; Polytechnic Institute of Viseu, Viseu, (Portugal)
joliveira@esav.ipv.pt
Cristina Ferreira, MD
Serviço de Anestesiologia, Centro Hospitalar Universitário do Porto, Porto, (Portugal)
crispintoferreira@gmail.com
Fátima Cruz, MD
Serviço de Anestesiologia, Centro Hospitalar Universitário do Porto, Porto, (Portugal)
mfatimabcruz@gmail.com
Correspondence: Diogo S Miguel, MD Serviço de Anestesiologia, Centro Hospitalar do Porto Largo Prof. Abel Salazar 4099-001 Porto (Portugal)
Phone: +351 22 2077549
E-mail: diogo.silva.miguel@gmail.com
ABSTRACT
Background: Obesity is an important public health problem, with a high prevalence worldwide. Bariatric surgery emerged as an effective therapeutic tool, with improvement of quality of life and a decrease in all-cause mortality. Obesity Surgery Mortality Risk Score (OS-MRS) predicts 90-day mortality after bariatric surgery, but its association with hospital length of stay (LOS) has not been elucidated. We aimed to evaluate the association between OS-MRS and LOS after gastric bypass surgery.
Methodology: We retrieved clinical and demographic data of 474 patients who had been submitted to gastric bypass surgery for this retrospective audit at Hospital de Santo António, Centro Hospitalar Universitário do Porto, Porto, (Portugal), between January 2010 and May 2015. The patients were classified as Class A, B or C. The primary goal was to evaluate whether there was an association between OS-MRS and LOS after gastric bypass surgery. The study of the relationship between duration of surgery (DS) and LOS was also performed.
Results: After application of exclusion criteria, 402 patients were included in the statistical analysis (172 patients Class A, 187 Class B and 43 Class C). Patients classified as OS-MRS Class A had a significant shorter LOS (3.5 ± 2.3 days) than patients classified as Class B (4.2 ± 5.1 days) and Class C (5.7 ± 12.6 days; p<0.001). A significant positive correlation between DS and LOS was observed, although the degree of that correlation was weak (ρ=0.203; p=0.001).
Conclusion: A positive association of OS-MRS with hospital length of stay and duration of surgery was observed; the patients with higher OS-MRS classes had longer length of stay in the hospital and longer duration of surgery. Moreover, longer length of stay was slightly associated with longer surgery duration.
Key words: Obesity; Bariatric surgery; Hospital length of stay; Obesity, Morbid/surgery; Obesity surgery mortality risk score; OS-MRS
Citation: Miguel DS, Ramos P, Oliveira J, Ferreira C, Cruz F. OS-MRS as a predictor of hospital length of stay – a retrospective audit of patients submitted to elective gastric bypass surgery. Anaesth pain intensive care 2020;24(1):_
DOI: https://DOI.org/10.35975/apic.v2i1.
Received – 29 November 2019; Reviewed –24 January, 8 February 2020; Revised – 24 January 2020; Accepted – 8 February 2020
INTRODUCTION
Obesity is nowadays recognised as an important public health problem, having achieved epidemic proportions. According to World Health Organization, in 2016 the world prevalence of obesity among adults was around 39%,1 and the same organization estimates that every year at least 2.8 million people die worldwide as a result of being overweight or obese.
Among the therapeutic options to deal with obesity, there have been some surgical approaches that aim to promote weight loss. Indeed, bariatric surgery can have an important positive impact in obese patients, leading to sustained weight loss, improvement of obesity related comorbidities.2-4 better quality of life,5 and ultimately a decrease of all-cause mortality.6
To access and stratify the risk of patients submitted to bariatric surgery, DeMaria et al. proposed a clinical score to predict 90-day mortality. Obesity Surgery Mortality Risk Score (OS-MRS) ranges from 0 to 5, with 1 point attributed per each of 5 variables: Body Mass Index (BMI) > 50 Kg/m2, arterial hypertension, male sex, age > 45 years old and risk factors for pulmonary thromboembolism (previous venous thromboembolism, previous inferior vena cava filter placement, history of right heart failure or pulmonary hypertension and/or history or physical findings of venous stasis). Patients may be classified as Class A (OS-MRS=0-1), B (OS-MRS=2-3) or C (OS-MRS=4-5), with expected mortality of 0.31%, 1.90% or 7.56%, respectively.7 After the first study by DeMaria et al., several other authors validated the OS-MRS as a useful score to predict 90-day mortality after bariatric surgery.8-11
Several authors have studied the OS-MRS relation with surgical complications, with contradicting results: while Sarela et al.12 and Lorente et al.13 have found an association with complications rate, several others have not replicated these results.14-17
However, the evidence regarding the association of OS-MRS with hospital length of stay (LOS) is still scarce, and the authors of this article could only found one study in which both OS-MRS and POSSUM scores were found to be moderately accurate for predicting inpatient stay longer than 3 days.16
In this study 474 patients submitted to gastric bypass surgery were retrospectively audited. The primary goal was to evaluate whether there was an association between OS-MRS and LOS after gastric bypass surgery. Additionally, the relationship between LOS and duration of surgery (DS) was also accessed.
METHODOLOGY
After approval by the institutional review board (114-15; 102-DEFI/NA-CES), a retrospective audit was conducted in a Portuguese tertiary university and central hospital (Hospital de Santo António, Centro Hospitalar Universitário do Porto, Porto, Portugal) between January 2010 and May 2015. Clinical and demographic data were collected, namely: age, gender, American Society of Anaesthesiology (ASA) Physical Status Classification, weight, height, OS-MRS, LOS and 90-day outcome. Patients with incomplete records, submitted to laparotomy or other bariatric procedures than gastric bypass were excluded. According to OS-MRS, the patients were classified as OS-MRS Class A, B or C.7
Normality of distribution of continuous variables was tested with Kolmogorov-Smirnov test. Accordingly, to analyse the influence of OS-MRS Class on LOS, the non-parametric Kruskal-Wallis with Dunn's post-hoc test was performed. Spearman correlation test was used to study the relationship between SL and LOS. Categorical data were analysed using the χ2 test.
The statistical analysis was performed using SPSS® version 23. A p < 0.05 was considered statistically significant.
RESULTS
A total of 474 patients were submitted to a gastric bypass between January 2010 and May 2015. After exclusion criteria, 402 patients were enrolled, and included in three groups, based on OS-MRS Class: 172 patients were classified as Class A, 187 as Class B and 43 as Class C (Figure 1).
Table 1 shows the demographic and clinical data. Gender and age were statistically different between groups, while no differences were found in ASA classification and BMI. Moreover, SL was progressively longer with increasing OS-MRS Class, with the difference between Class A and Class C showing statistical significance.
| Demographic and clinical data | OS-MRS Class | p | |||
| A (n=172) | B (n=187) | C (n=43) | |||
| Sex | F | 168 | 149 | 11 | < 0.001 |
| M | 4 | 38 | 32 | ||
| ASA | 2 | 46 | 39 | 3 | 0.238 |
| 3 | 126 | 146 | 38 | ||
| 4 | 0 | 2 | 2 | ||
| Age | 36.88 ± 7.73a | 48.91 ± 9.58b | 50.86 ± 7.14b | < 0.001 | |
| Body Mass Index | 43.18 ± 6.39 | 44.32 ± 5.94 | 46.62 ± 7.59 | 0.072 | |
| Duration of surgery | 127.53 ± 35.95a | 136.88 ± 43.46a,b | 151.95 ± 51.50b | 0.007 | |
| LOS | 3.5 ± 2.3a | 4.2 ± 5.1b | 5.7 ± 12.6b | 0.001 | |
| Values are expressed as mean ± SD except for the sex and ASA classification. Values in the same line that do not share the same superscript are statistically different (p<0.05). See text for more detail. | |||||
Regarding the primary goal of this study, patients classified as OS-MRS Class A had a statistically significant shorter LOS (3.5 ± 2.3 days) than patients classified as Class B (4.2 ± 5.1 days) and Class C (5.7 ± 12.6 days; p=0.001). The difference between patients classified as Class B and Class C was not statistically different (Figure 2).
The study of the relationship between SL and LOS was also performed (Figure 3). Although there is a statistically significant correlation between both variables, the degree of that correlation is weak (ρ = 0.203; p < 0.001).
DISCUSSION
There is a positive association between OS-MRS class and LOS, with patients with higher classes having longer hospital stay.
Our results are aligned with a previous work by Gilhooly et al., which showed that both OS-MRS and POSSUM scores were moderately accurate for predicting stay of 3 or more days due to morbidity and poor mobility.16
Our study has also found a positive correlation between the SL and LOS. In addition, SL was also progressively longer with increasing OS-MRS class. This finding may be justified with the assumption that the patients with higher OS-MRS class might represent greater technical difficulty for the surgeon, thus increasing the procedure time. Therefore, both the complexity of the patient and the difficulty of the procedure may explain the longer LOS.
STUDY LIMITATIONS
Being a retrospective audit, randomization and investigational unawareness were not included. Thus, a prospective, double blind randomized trial may add information to the results shown in this study.
The discharge criteria have not been strictly defined. Furthermore, the clinical records were in many cases incomplete and did not allow a more extensive and complete data collection regarding patient’s clinical characteristics and their evolution following surgery.
In addition, this was a single centre study, which may affect the generalization of the conclusions.
CONCLUSIONS
A positive association of OS-MRS with hospital length of stay and duration of surgery was observed, with patients with higher OS-MRS classes having longer length of stay and had longer duration of surgery. Moreover, longer length of stay was slightly associated with longer surgery duration.
Conflict of interest: None declared by the authors.
Authors’ contribution:
DM: Concept, bibliography review, data collection, statistical analysis, manuscript editing
PR: Concept, bibliography review, data collection, manuscript editing
JO: Concept, statistical analysis, manuscript editing
CF, FC: Concept, bibliography review, manuscript review, final approval
REFERENCES
- WHO. Global Health Observatory (GHO) data. 2017. Available from: http://www.who.int/gho/ncd/risk_factors/overweight/en/ Accessed on: 11 October 2018
- Fouse T, Brethauer S. Resolution of Comorbidities and Impact on Longevity Following Bariatric and Metabolic Surgery. Surg Clin North Am. 2016;96:717-32. [Pubmed] DOI: 10.1016/j.suc.2016.03.007
- Torres-Landa S, Kannan U, Guajardo I, Pickett-Blakely OE, Dempsey DT, Williams NN, et al. Surgical management of obesity. Minerva Chir. 2018;73:41-54. [Pubmed] DOI: 10.23736/s0026-4733.17.07588-5
- Lopes EC, Heineck I, Athaydes G, Meinhardt NG, Souto KE, Stein AT. Is Bariatric Surgery Effective in Reducing Comorbidities and Drug Costs? A Systematic Review and Meta-Analysis. Obes Surg. 2015;25:1741-9. [Pubmed] DOI: 10.1007/s11695-015-1777-5
- Raaijmakers LC, Pouwels S, Thomassen SE, Nienhuijs SW. Quality of life and bariatric surgery: a systematic review of short- and long-term results and comparison with community norms. Eur J Clin Nutr. 2017;71:441-9. [Pubmed]
- Cardoso L, Rodrigues D, Gomes L, Carrilho F. Short- and long-term mortality after bariatric surgery: A systematic review and meta-analysis. Diabetes Obes Metab. 2017;19:1223-32. [Pubmed] DOI: 10.1111/dom.12922
- DeMaria EJ, Portenier D, Wolfe L. Obesity surgery mortality risk score: proposal for a clinically useful score to predict mortality risk in patients undergoing gastric bypass. Surg Obes Relat Dis. 2007;3:134-40. [Pubmed]
- Arterburn D, Johnson ES, Butler MG, Fisher D, Bayliss EA. Predicting 90-day mortality after bariatric surgery: an independent, external validation of the OS-MRS prognostic risk score. Surg Obes Relat Dis. 2014;10:774-9. [Pubmed] DOI: 10.1016/j.soard.2014.04.006
- Brolin RE, Cody RP, Marcella SW. Differences in open versus laparoscopic gastric bypass mortality risk using the Obesity Surgery Mortality Risk Score (OS-MRS). Surg Obes Relat Dis. 2015;11:1201-6. [Pubmed] DOI: 10.1016/j.soard.2015.02.001
- DeMaria EJ, Murr M, Byrne TK, Blackstone R, Grant JP, Budak A, et al. Validation of the obesity surgery mortality risk score in a multicenter study proves it stratifies mortality risk in patients undergoing gastric bypass for morbid obesity. Ann Surg. 2007;246:578-82; discussion 83-4. [Pubmed] DOI: 10.1097/SLA.0b013e318157206e
- Efthimiou E, Court O, Sampalis J, Christou N. Validation of Obesity Surgery Mortality Risk Score in patients undergoing gastric bypass in a Canadian center. Surg Obes Relat Dis. 2009;5:643-7. [Pubmed] DOI: 10.1016/j.soard.2009.08.010
- Sarela AI, Dexter SP, McMahon MJ. Use of the obesity surgery mortality risk score to predict complications of laparoscopic bariatric surgery. Obes Surg. 2011;21:1698-703. [Pubmed] DOI: 10.1007/s11695-011-0379-0
- Lorente L, Ramon JM, Vidal P, Goday A, Parri A, Lanzarini E, et al. Obesity surgery mortality risk score for the prediction of complications after laparoscopic bariatric surgery. Cir Esp. 2014;92:316-23. [Pubmed] DOI: 10.1016/j.ciresp.2013.09.014
- Coblijn UK, Lagarde SM, de Raaff CA, de Castro SM, van Tets WF, Jaap Bonjer H, et al. Evaluation of the obesity surgery mortality risk score for the prediction of postoperative complications after primary and revisional laparoscopic Roux-en-Y gastric bypass. Surg Obes Relat Dis. 2016;12:1504-12. [Pubmed]
- Garcia-Garcia ML, Martin-Lorenzo JG, Liron-Ruiz R, Torralba-Martinez JA, Garcia-Lopez JA, Aguayo-Albasini JL. Failure of the Obesity Surgery Mortality Risk Score (OS-MRS) to Predict Postoperative Complications After Bariatric Surgery. A Single-Center Series and Systematic Review. Obes Surg. 2017;27:1423-9. [Pubmed] DOI: 10.1007/s11695-016-2506-4
- Gilhooly DA, Cole M, Moonesinghe SR. The evaluation of risk prediction models in predicting outcomes after bariatric surgery: a prospective observational cohort pilot study. Perioper Med (Lond). 2018;7:6. [Pubmed] [Free Full Text]
- Major P, Wysocki M, Pedziwiatr M, Malczak P, Pisarska M, Migaczewski M, et al. Can the Obesity Surgery Mortality Risk Score predict postoperative complications other than mortality? Wideochir Inne Tech Maloinwazyjne. 2016;11:247-52. [Pubmed] [Free Full Text] DOI: 10.5114/wiitm.2016.64448