Karishma Bansal, Department of Anesthesiology, MMU, Mullana, Haryana, Mullana,Haryana (India); E-mail: karishmabansal60@gmail.com
Madhavi Unmesh Santpur, Department of Anesthesiology, Maharishi Markandeshwar University, Mullana, Haryana (India); E-mail: madhavisantpur90@gmail.com
Utkarsh Garg, Department of Surgery, MMU, Mullana, Haryana (India); E-mail: drutarsh11@gmail.com
Kritesh Goel, Department of Surgery, Maharishi Markandeshwar University, Mullana, Haryana (India); E-mail: drkriteshgoel@yahoo.com
Divya Vijay, Department of Anesthesiology, Maharishi Markandeshwar University, Mullana, Haryana (India); E-mail: drdivyavijay45@gmail.com
Venugopal Tatineni, Department of Anesthesiology, Maharishi Markandeshwar University, Mullana, Haryana (India); E-mail: drtatinenivenu@gmail.com
Correspondence: Dr Madhavi Unmesh Santpur, Department of Anesthesiology, Maharishi Markandeshwar University, Mullana, Haryana (India); Phone: +91-9422406899; Mobile: +91-8059931425; E-mail: madhavisantpur90@gmail.com
ABSTRACT
Background and Aim: Pneumoperitoneum (PP) for laparoscopic surgery is known to induce a pressor response. It can be attenuated by drugs, like opioids, vasodilators, beta blocking agents and alpha-2 agonists, but these drugs have their side effects. This study investigated the efficacy of magnesium sulphate to attenuate hemodynamic response associated with pneumoperitoneum in patients undergoing laparoscopic cholecystectomy.
Methodology: This randomized, double blind, prospective study was carried out at Department of Anesthesiology, Maharishi Markandeshwar University, Mullana, Haryana (India). A total of 60 patients of ASA grade I or II, aged 20-60 y, of either sex, undergoing laparoscopic cholecystectomy, were randomly allocated into one of the two groups of 30 each. Standardized general anesthesia was administered to all patients. Group 1 patients received magnesium sulphate (30 mg/kg) intravenously as a bolus before induction of PP and Group 2 patients received same volume of 0.9% normal saline. Hemodynamic variables, e.g. heart rate (HR), systolic (SBP), diastolic (DBP), mean arterial pressures (MAP) were recorded from the start of surgery till extubation. Statistical analysis: SPSS version 17.0 for windows was used and p value of < 0.05 was considered significant.
Results: Mean HR was 81.50 ± 8.44 vs. 93.03 ± 6.93/min, SBP was 126.37 ± 13.03 vs. 150.20 ± 10.45 mmHg, DBP was 82.50 ± 11.20 vs. 94.73 ± 8.33 mmHg, and MAP 98.43 ± 10.29 vs.113.27 ± 9.16 mmHg in Group 1 and Group 2, respectively, at 10 min after PP. Statistically significant fall in HR, SBP, DBP, MAP was seen in Group 1 at 10 min after PP till extubation. (p < 0.05).
Conclusion: Intravenous magnesium sulphate effectively attenuates the hemodynamic response to pneumoperitoneum in laparoscopic cholecystectomy under general anesthesia.
Key words: Intravenous; Magnesium sulphate; Pneumoperitoneum; Laparoscopic cholecystectomy; Hemodynamics
Citation: Bansal K, Santpur MU, Garg U, Goel K, Vijay D, Tatineni Bansal. Effect of intravenous magnesium sulphate on hemodynamic response to pneumoperitoneum in laparoscopic cholecystectomy: A prospective, double blind study. Anaesth pain & intensiv care 2019;23(3):290-294
Received – 14 November 2018; Reviewed – 26, 28 December 2018, 30 April 2019; Accepted – 10 August 2019
INTRODUCTION
First laparoscopic cholecystectomy was performed by Phillipe Mouret and soon the procedure got wide-spread acceptance, as being less traumatic.1 The complications associated of pneumoperitoneum (PP) including neurohumoral stress response, however, continued to pose a challenge.2 PP causes an increase in plasma catecholamine levels2-4 and intrathoracic pressure, leading to release of vasopressin,5-7 which in turn results in an increased MAP without a significant change in HR.6,8 Hemodynamic stability can be achieved by the use of opioids,9 vasodilators,10 beta blockers,11 and alpha-2 agonists;6 however, none of these directly blocks catecholamine release.
Magnesium has been shown to inhibit the release of catecholamine’s from adrenergic nerves,12,13 produce vasodilatation, attenuate vasopressin-mediated vasoconstriction and normalize sensitivity to vasopressin.14
Our study aimed to evaluate the effect of intravenous magnesium sulphate on hemodynamic response to pneumoperitoneum in laparoscopic cholecystectomy as a primary outcome measure and to observe the adverse effects if any, as the secondary outcome measure.
METHODOLOGY
After obtaining approval from the Institutional Ethical Committee, this prospective, randomized, double blind study was conducted at the department of anesthesiology, over a period of two years (2015-2017). The enrolled patients were allocated into one of the two groups of 30 each scheduled to undergo elective laparoscopic cholecystectomy.
Inclusion & exclusion criteria: Patients included were ASA grade I & II of either gender, aged between 20 to 60 years undergoing laparoscopic cholecystectomy.
Patients excluded were, ASA Grade III & IV, who refused, with bleeding disorders, on calcium channel blockers, with hepatic, renal or cardiovascular dysfunction and in whom laparoscopy was converted to open procedure.
Methodology: Preanesthetic checkup was done a day before surgery. Detailed history, physical examination including baseline HR, BP, respiratory rate (RR) and systemic examination was done. Routine investigations including hemoglobin (Hb), bleeding time (BT), clotting time (CT), liver function tests (LFT), renal function tests (RFT), complete urine examination, random blood sugar (RBS), electrocardiography (ECG) and chest x-ray were done. Informed and valid written consent was obtained both for conduct of study as well as for administration of general anesthesia. All patients were kept fasting overnight and premedicated with Tab alprazolam 0.25 mg and Tab ranitidine 150 mg on the night prior to surgery and in the morning of surgery with a sip of water.
Allocation of groups: We calculated the effect size, which was coming up to 1.82 at alpha level 0.05. The power of the study was 99%, which depicted that total sample size might be 60 (30 each for both the groups). G* power was used for calculating the sample size.
The patients were randomly divided into two groups of 30 each.
Group 1– MgSO4 group, patients received MgSO4 30 mg/kg IV as a bolus just before PP.
Group 2– control group, patients received 0.9% normal saline (NS) in equal volume.
The study medication was prepared in identical 20 ml syringe, randomization was done by computer generated number. The drug was prepared and given by a person other than the observer who kept the record. The results were decoded at the end of the study.
Intraoperative period:
After shifting the patient to the operating room, routine monitoring was started and baseline vital parameters (HR, BP, and SpO2) were recorded. IV access was secured with 18G cannula. Patients were premedicated with glycopyrrolate 0.01 mg/kg, midazolam 0.05 mg/kg, and fentanyl 2 µg/kg IV and induction was done with IV propofol 2 mg/kg and IV vecuronium 0.1 mg/kg. Patients were intubated with cuffed endotracheal tube of appropriate size and maintained on O2, N2O, isoflurane, vecuronium (additional doses of muscle relaxant were given as per neuromuscular monitoring) and intermittent positive pressure ventilation (IPPV). The group drug was administered intravenously over two to three minutes before PP.
Carbon dioxide (CO2) was insufflated into the peritoneal cavity to create PP. Intraabdominal pressure was maintained at 12 mmHg throughout the laparoscopic procedure. The patients were mechanically ventilated and end tidal CO2 (EtCO2) was maintained between 35-40 mmHg.
HR, SBP and DBP and MAP were recorded baseline, before PP, 10 min after PP till extubation.
At the end of the operation, ondansetron 4 mg IV was administered for prophylaxis against nausea and vomiting. Neuromuscular blockade was reversed by appropriate doses of neostigmine / glycopyrrolate and trachea was extubated.
Patients were observed for any adverse effects like bradycardia, hypotension, arrhythmias and delayed recovery in postoperative period.
Statistical analysis: The data from the above study was systematically collected, compiled and statistically analyzed in SPSS version 17.0 for windows to draw relevant conclusions. t and Chi square tests were used for different parameters. A p-value of < 0.05 was considered significant.
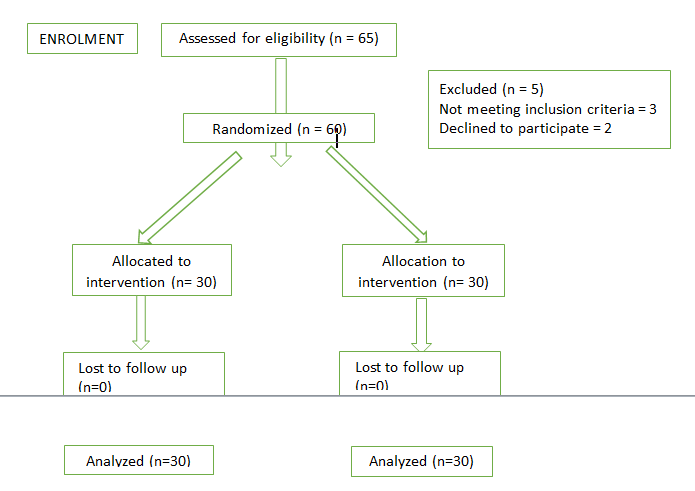
Figure 1: Consort flow diagram
RESULTS
The study was carried out on 60 patients between the age group 20-60 years to evaluate the effect of MgSO4 on hemodynamic response to PP.
Demographic profile of the patients, e.g., age, gender, weight, ASA grades were comparable in both the groups.
As evident from Table 1, the baseline HR and HR just before PP were comparable among both the groups as p > 0.05. Mean HR in Group 1 was 81.50 ± 8.44 bpm and it was 93.03 ± 6.93 bpm in Group 2 at 10 min after PP. Statistically significant fall in HR was seen in Group 1 at 10 min after PP till extubation (p < 0.05).
Table I: Comparative mean HR (BPM) in both groups
Comparative data of SBP is given in Table 2. Baseline SBP and SBP before PP were comparable among both the groups (p > 0.05). Mean SBP in Group 1 was 126.37 ± 13.03 mmHg and in Group 2 it was 150.20 ± 10.45 mmHg at 10 min after PP. Statistically significant fall in SBP was observed in Group 1 at 10 min after PP which persisted till extubation (p < 0.05).
Table 2: Comparison of SBP (mmHg) in both groups
Table 3: Comparison of DBP (mmHg) in both groups
As evident from the Table 3, baseline DBP and DBP before PP were comparable among both the groups (p > 0.05). Statistically significant fall in DBP was observed in Group 1 at 10 min after PP which persisted till extubation (p < 0.05).
Table 4 shows baseline MAP and MAP before PP were comparable among both the groups (p > 0.05). Statistically significant fall in MAP was observed in Group 1 at 10 min after PP which persisted till extubation (p < 0.05).
Table 4: Comparison of MAP (mmHg) in both groups
Mean distribution of EtCO2 was comparable in both the groups.
DISCUSSION
The present study was a randomized, double blind study, to evaluate the effect of IV MgSO4 on hemodynamic response to PP during laparoscopic cholecystectomy. PP causes rapid and immediate increase in plasma catecholamine’s,3-5 which activates renin-angiotensin-aldosterone system, possibly due to an increase in intraperitoneal pressure and stimulation of peritoneum by CO2.3 PP also leads to an increase in the intrathoracic pressure leading to a fall in transmural right atrial pressure which stimulates release of vasopressin.6-8
Cardiovascular response to PP is an increase in arterial pressures,7,9 decrease in cardiac output and marked increase in systemic vascular resistance.
Action of MgSO4 is multimodal; It inhibits the release of catecholamine’s from the adrenergic nerve terminals and adrenal glands,14-15 therefore, it is being used in managing cases of pheochromocytoma, pre-eclampsia, eclampsia and other conditions. It produces vasodilatation by acting directly on the blood vessels and thus, can attenuate the vasopressin mediated vasoconstriction. It is also used to attenuate the pressor response associated with tracheal intubation. It has antinociceptive effects due to the regulation of calcium influx into the cell and that is the natural physiological antagonism of the NMDA receptor. Therefore, by virtue of these properties the drug is being explored for varied clinical applications and was used to attenuate the hemodynamic response to PP in laparoscopic cholecystectomy in the present study.
In our study, the baseline HR and HR before PP was comparable among both the groups (p > 0.05). Statistically significant fall in HR was seen in Mg Group at 10 min after PP till extubation (p < 0.05). Kamble SP concluded that HR of patients in Group NS when compared with Groups M (IV MgSO4 50 mg/kg prior to PP) and C (clonidine), had significantly higher HR at five min after PP to 40 min after PP (p < 0.001) and, HR was significantly lower in Group M as compared to Group NS at all time intervals (p < 0.001).15 Paul S et al. concluded that there was a significant fall in HR in Group M (MgSO4 30 mg/kg bolus before PP) at 15 min post-PP till extubation as compared to Group C (NS) (p < 0.05).16 Both the studies were in accordance with the present study in terms of mean distribution of HR at various time intervals.
As shown in Table 4, in our study, baseline MAP and MAP before PP were comparable among both the groups (p > 0.05). Statistically significant fall in DBP was observed in Mg group at 10 min after PP which persisted till extubation (p < 0.05). Paul S. et al. concluded that there was a significant fall in MAP in Group MgSO4 at 15 min post PP till extubation as compared to Group C (NS) (p < 0.05). This study was in accordance with the present study in terms of MAP.
In our study, no significant change was seen in EtCO2 in both the groups at various time intervals, nor any adverse effect like bradycardia, hypotension, arrhythmias and delayed recovery from anesthesia were observed in either group.
CONCLUSION
Intravenous magnesium sulphate given just prior to induction of pneumoperitoneum significantly lowers the heart rate and arterial pressure, thus maintaining the hemodynamic stability throughout the duration of pneumoperitoneum. No adverse effects were seen with administration of magnesium sulphate, hence it can be used as an alternative drug to attenuate hemodynamic response to pneumoperitoneum in laparoscopic cholecystectomy.
Conflict of interest: None declared by the authors
Authors’ contribution:
KB, MS: Conduct of study, manuscript editing
UG, KG: Conduct of study, Literature search
DV, VT: Literature search, Statistical analysis
REFERENCES
Madhavi Unmesh Santpur, Department of Anesthesiology, Maharishi Markandeshwar University, Mullana, Haryana (India); E-mail: madhavisantpur90@gmail.com
Utkarsh Garg, Department of Surgery, MMU, Mullana, Haryana (India); E-mail: drutarsh11@gmail.com
Kritesh Goel, Department of Surgery, Maharishi Markandeshwar University, Mullana, Haryana (India); E-mail: drkriteshgoel@yahoo.com
Divya Vijay, Department of Anesthesiology, Maharishi Markandeshwar University, Mullana, Haryana (India); E-mail: drdivyavijay45@gmail.com
Venugopal Tatineni, Department of Anesthesiology, Maharishi Markandeshwar University, Mullana, Haryana (India); E-mail: drtatinenivenu@gmail.com
Correspondence: Dr Madhavi Unmesh Santpur, Department of Anesthesiology, Maharishi Markandeshwar University, Mullana, Haryana (India); Phone: +91-9422406899; Mobile: +91-8059931425; E-mail: madhavisantpur90@gmail.com
ABSTRACT
Background and Aim: Pneumoperitoneum (PP) for laparoscopic surgery is known to induce a pressor response. It can be attenuated by drugs, like opioids, vasodilators, beta blocking agents and alpha-2 agonists, but these drugs have their side effects. This study investigated the efficacy of magnesium sulphate to attenuate hemodynamic response associated with pneumoperitoneum in patients undergoing laparoscopic cholecystectomy.
Methodology: This randomized, double blind, prospective study was carried out at Department of Anesthesiology, Maharishi Markandeshwar University, Mullana, Haryana (India). A total of 60 patients of ASA grade I or II, aged 20-60 y, of either sex, undergoing laparoscopic cholecystectomy, were randomly allocated into one of the two groups of 30 each. Standardized general anesthesia was administered to all patients. Group 1 patients received magnesium sulphate (30 mg/kg) intravenously as a bolus before induction of PP and Group 2 patients received same volume of 0.9% normal saline. Hemodynamic variables, e.g. heart rate (HR), systolic (SBP), diastolic (DBP), mean arterial pressures (MAP) were recorded from the start of surgery till extubation. Statistical analysis: SPSS version 17.0 for windows was used and p value of < 0.05 was considered significant.
Results: Mean HR was 81.50 ± 8.44 vs. 93.03 ± 6.93/min, SBP was 126.37 ± 13.03 vs. 150.20 ± 10.45 mmHg, DBP was 82.50 ± 11.20 vs. 94.73 ± 8.33 mmHg, and MAP 98.43 ± 10.29 vs.113.27 ± 9.16 mmHg in Group 1 and Group 2, respectively, at 10 min after PP. Statistically significant fall in HR, SBP, DBP, MAP was seen in Group 1 at 10 min after PP till extubation. (p < 0.05).
Conclusion: Intravenous magnesium sulphate effectively attenuates the hemodynamic response to pneumoperitoneum in laparoscopic cholecystectomy under general anesthesia.
Key words: Intravenous; Magnesium sulphate; Pneumoperitoneum; Laparoscopic cholecystectomy; Hemodynamics
Citation: Bansal K, Santpur MU, Garg U, Goel K, Vijay D, Tatineni Bansal. Effect of intravenous magnesium sulphate on hemodynamic response to pneumoperitoneum in laparoscopic cholecystectomy: A prospective, double blind study. Anaesth pain & intensiv care 2019;23(3):290-294
Received – 14 November 2018; Reviewed – 26, 28 December 2018, 30 April 2019; Accepted – 10 August 2019
INTRODUCTION
First laparoscopic cholecystectomy was performed by Phillipe Mouret and soon the procedure got wide-spread acceptance, as being less traumatic.1 The complications associated of pneumoperitoneum (PP) including neurohumoral stress response, however, continued to pose a challenge.2 PP causes an increase in plasma catecholamine levels2-4 and intrathoracic pressure, leading to release of vasopressin,5-7 which in turn results in an increased MAP without a significant change in HR.6,8 Hemodynamic stability can be achieved by the use of opioids,9 vasodilators,10 beta blockers,11 and alpha-2 agonists;6 however, none of these directly blocks catecholamine release.
Magnesium has been shown to inhibit the release of catecholamine’s from adrenergic nerves,12,13 produce vasodilatation, attenuate vasopressin-mediated vasoconstriction and normalize sensitivity to vasopressin.14
Our study aimed to evaluate the effect of intravenous magnesium sulphate on hemodynamic response to pneumoperitoneum in laparoscopic cholecystectomy as a primary outcome measure and to observe the adverse effects if any, as the secondary outcome measure.
METHODOLOGY
After obtaining approval from the Institutional Ethical Committee, this prospective, randomized, double blind study was conducted at the department of anesthesiology, over a period of two years (2015-2017). The enrolled patients were allocated into one of the two groups of 30 each scheduled to undergo elective laparoscopic cholecystectomy.
Inclusion & exclusion criteria: Patients included were ASA grade I & II of either gender, aged between 20 to 60 years undergoing laparoscopic cholecystectomy.
Patients excluded were, ASA Grade III & IV, who refused, with bleeding disorders, on calcium channel blockers, with hepatic, renal or cardiovascular dysfunction and in whom laparoscopy was converted to open procedure.
Methodology: Preanesthetic checkup was done a day before surgery. Detailed history, physical examination including baseline HR, BP, respiratory rate (RR) and systemic examination was done. Routine investigations including hemoglobin (Hb), bleeding time (BT), clotting time (CT), liver function tests (LFT), renal function tests (RFT), complete urine examination, random blood sugar (RBS), electrocardiography (ECG) and chest x-ray were done. Informed and valid written consent was obtained both for conduct of study as well as for administration of general anesthesia. All patients were kept fasting overnight and premedicated with Tab alprazolam 0.25 mg and Tab ranitidine 150 mg on the night prior to surgery and in the morning of surgery with a sip of water.
Allocation of groups: We calculated the effect size, which was coming up to 1.82 at alpha level 0.05. The power of the study was 99%, which depicted that total sample size might be 60 (30 each for both the groups). G* power was used for calculating the sample size.
The patients were randomly divided into two groups of 30 each.
Group 1– MgSO4 group, patients received MgSO4 30 mg/kg IV as a bolus just before PP.
Group 2– control group, patients received 0.9% normal saline (NS) in equal volume.
The study medication was prepared in identical 20 ml syringe, randomization was done by computer generated number. The drug was prepared and given by a person other than the observer who kept the record. The results were decoded at the end of the study.
Intraoperative period:
After shifting the patient to the operating room, routine monitoring was started and baseline vital parameters (HR, BP, and SpO2) were recorded. IV access was secured with 18G cannula. Patients were premedicated with glycopyrrolate 0.01 mg/kg, midazolam 0.05 mg/kg, and fentanyl 2 µg/kg IV and induction was done with IV propofol 2 mg/kg and IV vecuronium 0.1 mg/kg. Patients were intubated with cuffed endotracheal tube of appropriate size and maintained on O2, N2O, isoflurane, vecuronium (additional doses of muscle relaxant were given as per neuromuscular monitoring) and intermittent positive pressure ventilation (IPPV). The group drug was administered intravenously over two to three minutes before PP.
Carbon dioxide (CO2) was insufflated into the peritoneal cavity to create PP. Intraabdominal pressure was maintained at 12 mmHg throughout the laparoscopic procedure. The patients were mechanically ventilated and end tidal CO2 (EtCO2) was maintained between 35-40 mmHg.
HR, SBP and DBP and MAP were recorded baseline, before PP, 10 min after PP till extubation.
At the end of the operation, ondansetron 4 mg IV was administered for prophylaxis against nausea and vomiting. Neuromuscular blockade was reversed by appropriate doses of neostigmine / glycopyrrolate and trachea was extubated.
Patients were observed for any adverse effects like bradycardia, hypotension, arrhythmias and delayed recovery in postoperative period.
Statistical analysis: The data from the above study was systematically collected, compiled and statistically analyzed in SPSS version 17.0 for windows to draw relevant conclusions. t and Chi square tests were used for different parameters. A p-value of < 0.05 was considered significant.
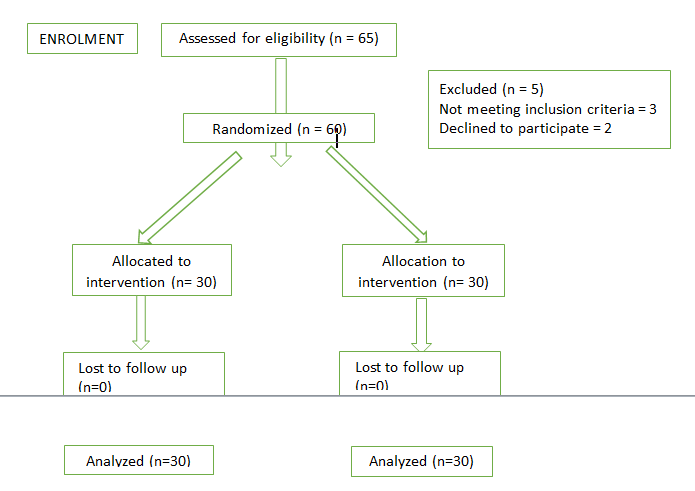
Figure 1: Consort flow diagram
RESULTS
The study was carried out on 60 patients between the age group 20-60 years to evaluate the effect of MgSO4 on hemodynamic response to PP.
Demographic profile of the patients, e.g., age, gender, weight, ASA grades were comparable in both the groups.
As evident from Table 1, the baseline HR and HR just before PP were comparable among both the groups as p > 0.05. Mean HR in Group 1 was 81.50 ± 8.44 bpm and it was 93.03 ± 6.93 bpm in Group 2 at 10 min after PP. Statistically significant fall in HR was seen in Group 1 at 10 min after PP till extubation (p < 0.05).
Table I: Comparative mean HR (BPM) in both groups
| Time | Group 1
Mean ± SD |
Group 2
Mean ± SD |
t | p-value |
| Baseline | 87.03 ± 13.08 | 81.47 ± 10.67 | 1.806 | 0.076 |
| Before PP | 88.63 ± 14.26 | 85.97 ± 9.83 | 0.843 | 0.402 |
| 10 min after PP | 81.50 ± 8.44 | 93.03 ± 6.93 | -5.785 | 0.000 |
| 20 min | 82.97 ± 11.61 | 90.50 ± 7.40 | -2.997 | 0.004 |
| 30 min | 80.37 ± 8.38 | 92.60 ± 11.04 | -4.834 | 0.000 |
| 45 min | 79.24 ± 9.29 | 92.47 ± 11.94 | -4.738 | 0.000 |
| 60 min | 77.55 ± 8.76 | 89.19 ± 11.86 | -3.387 | 0.002 |
| 75 min | 77.07 ± 7.53 | 90.40 ± 12.98 | -3.181 | 0.004 |
| 90 min | 77.33 ± 3.33 | 89.33 ± 9.87 | -2.840 | 0.025 |
| Release of PP | 77.60 ± 8.74 | 92.27 ± 12.04 | -5.401 | 0.000 |
| After extubation | 90.57 ± 10.68 | 101.07 ± 15.44 | -3.064 | 0.003 |
Comparative data of SBP is given in Table 2. Baseline SBP and SBP before PP were comparable among both the groups (p > 0.05). Mean SBP in Group 1 was 126.37 ± 13.03 mmHg and in Group 2 it was 150.20 ± 10.45 mmHg at 10 min after PP. Statistically significant fall in SBP was observed in Group 1 at 10 min after PP which persisted till extubation (p < 0.05).
Table 2: Comparison of SBP (mmHg) in both groups
| Time | Group 1
Mean ± SD |
Group 2
Mean ± SD |
t | p-value |
| Baseline | 130.37 ± 13.04 | 132.77 ± 10.78 | -0.777 | 0.440 |
| Before PP | 125.60 ± 12.94 | 120.87 ± 14.06 | 1.357 | 0.180 |
| 10 min after PP | 126.37 ± 13.03 | 150.20 ± 10.45 | -7.814 | 0.000 |
| 20 min | 120.47 ± 13.01 | 150.80 ± 9.70 | -10.239 | 0.000 |
| 30 min | 121.07 ± 8.99 | 152.63 ± 12.87 | -11.015 | 0.000 |
| 45 min | 119.45 ± 8.55 | 151.97 ± 13.86 | -10.798 | 0.000 |
| 60 min | 122.65 ± 9.03 | 152.25 ± 16.48 | -6.862 | 0.000 |
| 75 min | 121.50 ± 8.78 | 146.30 ± 12.50 | -5.726 | 0.000 |
| 90 min | 120.00 ± 10.56 | 146.33 ± 15.01 | -3.102 | 0.017 |
| Release of PP | 123.60 ± 10.62 | 147.70 ± 12.81 | -7.933 | 0.000 |
| After extubation | 139.73 ± 8.26 | 163.27 ± 21.98 | -5.489 | 0.000 |
Table 3: Comparison of DBP (mmHg) in both groups
| Time | Group 1
Mean ± SD |
Group 2
Mean ± SD |
t | p-value |
| Baseline | 82.47 ± 12.54 | 80.37 ± 8.93 | 0.747 | 0.458 |
| Before PP | 81.07 ± 10.42 | 82.90 ± 8.82 | -0.735 | 0.465 |
| 10 min after PP | 82.50 ± 11.20 | 94.73 ± 8.33 | -4.802 | 0.000 |
| 20 min | 75.53 ± 8.85 | 94.43 ± 7.60 | -8.874 | 0.000 |
| 30 min | 77.70 ± 8.47 | 96.73 ± 8.46 | -8.706 | 0.000 |
| 45 min | 74.34 ± 7.89 | 92.20 ± 9.35 | -7.913 | 0.000 |
| 60 min | 76.70 ± 9.68 | 92.94 ± 10.01 | -4.926 | 0.000 |
| 75 min | 79.07 ± 9.60 | 87.70 ± 9.02 | -2.226 | 0.037 |
| 90 min | 77.17 ± 9.33 | 93.33 ± 10.26 | -2.381 | 0.049 |
| Release of PP | 76.43 ± 9.02 | 91.60 ± 8.86 | -6.571 | 0.000 |
| After extubation | 86.30 ± 8.24 | 101.40 ± 8.90 | -6.821 | 0.000 |
As evident from the Table 3, baseline DBP and DBP before PP were comparable among both the groups (p > 0.05). Statistically significant fall in DBP was observed in Group 1 at 10 min after PP which persisted till extubation (p < 0.05).
Table 4 shows baseline MAP and MAP before PP were comparable among both the groups (p > 0.05). Statistically significant fall in MAP was observed in Group 1 at 10 min after PP which persisted till extubation (p < 0.05).
Table 4: Comparison of MAP (mmHg) in both groups
| Time | Group 1
Mean ± SD |
Group 2
Mean ± SD |
t | p-value |
| Baseline | 98.97 ± 13.22 | 95.73 ± 10.24 | 1.059 | 0.294 |
| Before PP | 95.93 ± 12.13 | 100.57 ± 7.34 | -1.789 | 0.079 |
| 10 min after PP | 98.43 ± 10.29 | 113.27 ± 9.16 | -5.898 | 0.000 |
| 20 min | 91.60 ± 9.63 | 113.40 ± 8.02 | -9.528 | 0.000 |
| 30 min | 93.30 ± 7.53 | 115.27 ± 10.87 | -9.101 | 0.000 |
| 45 min | 90.17 ± 7.05 | 113.50 ± 10.71 | -9.846 | 0.000 |
| 60 min | 93.75 ± 8.11 | 113.44 ± 14.07 | -5.270 | 0.000 |
| 75 min | 93.14 ± 9.21 | 106.80 ± 9.11 | -3.596 | 0.002 |
| 90 min | 91.17 ± 7.31 | 108.33 ± 10.12 | -2.958 | 0.021 |
| Release of PP | 92.83 ± 9.33 | 111.40 ± 10.65 | -7.184 | 0.000 |
| After extubation | 103.23 ± 7.75 | 123.67 ± 10.04 | -8.825 | 0.000 |
Mean distribution of EtCO2 was comparable in both the groups.
DISCUSSION
The present study was a randomized, double blind study, to evaluate the effect of IV MgSO4 on hemodynamic response to PP during laparoscopic cholecystectomy. PP causes rapid and immediate increase in plasma catecholamine’s,3-5 which activates renin-angiotensin-aldosterone system, possibly due to an increase in intraperitoneal pressure and stimulation of peritoneum by CO2.3 PP also leads to an increase in the intrathoracic pressure leading to a fall in transmural right atrial pressure which stimulates release of vasopressin.6-8
Cardiovascular response to PP is an increase in arterial pressures,7,9 decrease in cardiac output and marked increase in systemic vascular resistance.
Action of MgSO4 is multimodal; It inhibits the release of catecholamine’s from the adrenergic nerve terminals and adrenal glands,14-15 therefore, it is being used in managing cases of pheochromocytoma, pre-eclampsia, eclampsia and other conditions. It produces vasodilatation by acting directly on the blood vessels and thus, can attenuate the vasopressin mediated vasoconstriction. It is also used to attenuate the pressor response associated with tracheal intubation. It has antinociceptive effects due to the regulation of calcium influx into the cell and that is the natural physiological antagonism of the NMDA receptor. Therefore, by virtue of these properties the drug is being explored for varied clinical applications and was used to attenuate the hemodynamic response to PP in laparoscopic cholecystectomy in the present study.
In our study, the baseline HR and HR before PP was comparable among both the groups (p > 0.05). Statistically significant fall in HR was seen in Mg Group at 10 min after PP till extubation (p < 0.05). Kamble SP concluded that HR of patients in Group NS when compared with Groups M (IV MgSO4 50 mg/kg prior to PP) and C (clonidine), had significantly higher HR at five min after PP to 40 min after PP (p < 0.001) and, HR was significantly lower in Group M as compared to Group NS at all time intervals (p < 0.001).15 Paul S et al. concluded that there was a significant fall in HR in Group M (MgSO4 30 mg/kg bolus before PP) at 15 min post-PP till extubation as compared to Group C (NS) (p < 0.05).16 Both the studies were in accordance with the present study in terms of mean distribution of HR at various time intervals.
As shown in Table 4, in our study, baseline MAP and MAP before PP were comparable among both the groups (p > 0.05). Statistically significant fall in DBP was observed in Mg group at 10 min after PP which persisted till extubation (p < 0.05). Paul S. et al. concluded that there was a significant fall in MAP in Group MgSO4 at 15 min post PP till extubation as compared to Group C (NS) (p < 0.05). This study was in accordance with the present study in terms of MAP.
In our study, no significant change was seen in EtCO2 in both the groups at various time intervals, nor any adverse effect like bradycardia, hypotension, arrhythmias and delayed recovery from anesthesia were observed in either group.
CONCLUSION
Intravenous magnesium sulphate given just prior to induction of pneumoperitoneum significantly lowers the heart rate and arterial pressure, thus maintaining the hemodynamic stability throughout the duration of pneumoperitoneum. No adverse effects were seen with administration of magnesium sulphate, hence it can be used as an alternative drug to attenuate hemodynamic response to pneumoperitoneum in laparoscopic cholecystectomy.
Conflict of interest: None declared by the authors
Authors’ contribution:
KB, MS: Conduct of study, manuscript editing
UG, KG: Conduct of study, Literature search
DV, VT: Literature search, Statistical analysis
REFERENCES
- Vecchio R, Macfayden BV, Palazzo F. History of laparoscopic surgery.Panminerva Med. 2000:42:87-90. [PubMed]
- Myre K, Rostrup M, Buanes T, Stokland O. Plasma catecholamines and haemodynamic changes during pneumoperitoneum. Acta Anaesthesiol Scand. 1998;42:343–7. [PubMed] DOI: 1111/j.1399-6576.1998.tb04927.x
- Mikami O, Kawakita S, Fujise K, Shingu K, Takahashi H, Matsuda T. Catecholamine release caused by carbon dioxide insufflation during laparoscopic surgery. J Urol. 1996;155:1368–71. [PubMed]
- Koivusalo AM, Kellokumpu I, Scheinin M, Tikkanen I, Halme L, Lindgren L. Randomized comparison of the neuroendocrine response to laparoscopic cholecystectomy using either conventional or abdominal wall lift techniques. Br J Surg. 1996;83:1532–6. [PubMed] DOI: 1002/bjs.1800831112
- Joris JL, Chiche JD, Canivet JL, Jacquet NJ, Legros JJ, Lamy ML. Haemodynamic changes induced by laparoscopy and their endocrine correlates: effects of clonidine. J Am Coll Cardiol. 1998;32:1389-96. [PubMed] DOI: 1016/s0735-1097(98)00406-9
- Walder AD, Aitkenhead AR. Role of vasopressin in the haemodynamic response to laparoscopic cholecystectomy. Br J Anaesth. 1997;78:264-6. [PubMed] DOI: 1093/bja/78.3.264
- Mann C, Boccara G, Pouzeratte Y, Eliet J, Serradel-Le Gal C, Vergnes C, et al. The relationship among carbon dioxide pneumoperitoneum, vasopressin release, and haemodynamic changes. Anesth Analg. 1999;89:278-83. [PubMed] DOI: 1097/00000539-199908000-00003
- Sharma KC, Brandstetter RD, Brensilver JM, Jung LD. Cardiopulmonary physiology and pathophysiology as a consequence of laparoscopic surgery. Chest. 1996;110:810–5. [PubMed] DOI: 1378/chest.110.3.810
- Lentschener C, Axler O, Fernandez H, Megarbane B, Billard V, Fouqueray B, et al. Haemodynamic changes and vasopressin release are not consistently associated with carbon dioxide pneumoperitoneum in humans. Acta Anaesthesiol Scand. 2001;45:527-35. [PubMed] DOI: 1034/j.1399-6576.2001.045005527.x
- Joris JL, Hamoir EE, Hartstein GM, Meurisse MR, Hubert BM, Charlier CJ, et al. Haemodynamic changes and catecholamine release during laparoscopic adrenalectomy for pheochromocytoma. Anesth Analg. 1999;88 16-21. [PubMed] DOI: 1097/00000539-199901000-00004
- Koivusalo AM, Scheinin M, Tikkanen I, Yli-Suomu T, Ristkari S, Laakso J, et al. Effects of esmolol on haemodynamic response to CO2 pneumoperitoneum for laparoscopic surgery. Acta Anaesthesiol Scand. 1998;42:510-7. [PubMed] DOI: 1111/j.1399-6576.1998.tb05159.x
- Douglas WW, Rubin RP. The mechanism of catecholamine release from the adrenal medulla and the role of calcium in stimulus-secretion coupling. J Physiol. 1963;167:288-310. [PubMed] DOI: 1113/jphysiol.1963.sp007150
- Lishajko F. Releasing effect of calcium and phosphate on catecholamine’s, ATP, and protein from chromaffin cell granules. Acta Physiol Scand. 1970;79(4):575-85. [PubMed] DOI: 1111/j.1748-1716.1970.tb04760.x
- Laurant P, Touyz RM, Schiffrin EL. Effect of magnesium on vascular tone and reactivity in pressurized mesenteric resistance arteries from spontaneously hypertensive rats. Can J Physiol Pharmacol. 1997;75:293–300. [PubMed]
- Kamble SP, Bevinaguddaiah Y, Nagaraja DC, Pujar VS, Anandaswamy Effect of magnesium sulfate and clonidine in attenuating haemodynamic response to pneumoperitoneum in laparoscopic cholecystectomy. Anesth Essays Res. 2017;11(1):67-71. [PubMed] DOI: 10.4103/0259-1162.200228
- Paul S, Biswas P, Bhattacharjee DP, Sengupta J. Effects of magnesium sulphate on haemodynamic response to carbon dioxide pneumoperitoneum in patients undergoing laparoscopic cholecystectomy. Anesth Essays Res. 2013;7(2):228-31. [PubMed] DOI: 4103/0259-1162.118970